Abstract
Purpose
Propofol is commonly used with remifentanil for induction of general anesthesia (GA); however, it often leads to hypotension. Intraoperative hypotension is associated with postoperative adverse events. By contrast, thiopental has less negative inotropic effects on hemodynamics compared to propofol, which could be suitable to prevent hypotension during GA induction. In the present age-stratified, randomized, assessor-blinded study, using the ClearSight® system, we compared the hemodynamic effects of propofol and thiopental during GA induction under remifentanil infusion in non-cardiac surgery.
Methods
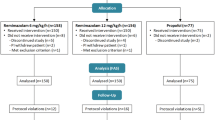
Patients were divided into young (20–40 year), middle (41–70 year), and elderly (> 70 year) groups (n = 20, each group). General anesthesia was induced with remifentanil 0.3 μg/kg/min, followed by propofol (2.0, 1.5, and 1.2 mg/kg) or thiopental (5.0, 4.0, and 3.0 mg/kg) in the young, middle, and elderly groups, respectively. The primary outcome was the difference in the decrease in mean arterial blood pressure between patients receiving propofol and thiopental in each age group. The secondary outcomes included other hemodynamic parameters and minimal bispectral index values measured up to 10 min after tracheal intubation.
Results
The decrease in mean arterial blood pressure was greater in patients receiving propofol than those receiving thiopental (− 45.4 vs − 26.6 mmHg and − 45.7 vs − 28.9 mmHg, P = 0.003 and 0.007, respectively), whereas no significant difference was observed in the young age group (P = 0.96).
Conclusions
Thiopental is a more suitable agent than propofol for avoiding hypotension during GA induction under remifentanil infusion in the middle and elderly patients.


Similar content being viewed by others
References
Poterman M, Scheeren TWL, van der Velde MI, Buisman PL, Allaert S, Struys M, Kalmar AF. Prophylactic atropine administration attenuates the negative haemodynamic effects of induction of anaesthesia with propofol and high-dose remifentanil: a randomised controlled trial. Eur J Anaesthesiol. 2017;34:695–701.
Reich DL, Hossain S, Krol M, Baez B, Patel P, Bernstein A, Bodian CA. Predictors of hypotension after induction of general anesthesia. Anesth Analg. 2005;101:622–8.
van Waes JA, van Klei WA, Wijeysundera DN, van Wolfswinkel L, Lindsay TF, Beattie WS. Association between intraoperative hypotension and myocardial injury after vascular surgery. Anesthesiology. 2016;124:35–44.
Walsh M, Devereaux PJ, Garg AX, Kurz A, Turan A, Rodseth RN, Cywinski J, Thabane L, Sessler DI. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology. 2013;119:507–15.
Blacker DJ, Flemming KD, Wijdicks EF. Risk of ischemic stroke in patients with symptomatic vertebrobasilar stenosis undergoing surgical procedures. Stroke. 2003;34:2659–63.
Bateman BT, Schumacher HC, Wang S, Shaefi S, Berman MF. Perioperative acute ischemic stroke in noncardiac and nonvascular surgery: incidence, risk factors, and outcomes. Anesthesiology. 2009;110:231–8.
Futier E, Lefrant JY, Guinot PG, Godet T, Lorne E, Cuvillon P, Bertran S, Leone M, Pastene B, Piriou V, Molliex S, Albanese J, Julia JM, Tavernier B, Imhoff E, Bazin JE, Constantin JM, Pereira B, Jaber S. Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: a randomized clinical trial. JAMA. 2017;318:1346–57.
Vuyk J, Sitsen E, Reekers M. Intravenous anesthetics. In: Miller RD, Cohen NH, Eriksson LI, editors. Miller's anesthesia. 8th ed. Philadelphia: Elsevier; 2015. p. 821-61.
Harris CE, Murray AM, Anderson JM, Grounds RM, Morgan M. Effects of thiopentone, etomidate and propofol on the haemodynamic response to tracheal intubation. Anaesthesia. 1988;43(Suppl):32–6.
Komatsu R, Turan AM, Orhan-Sungur M, McGuire J, Radke OC, Apfel CC. Remifentanil for general anaesthesia: a systematic review. Anaesthesia. 2007;62:1266–80.
Sorensen MK, Dolven TL, Rasmussen LS. Onset time and haemodynamic response after thiopental vs. propofol in the elderly: a randomized trial. Acta Anaesthesiol Scand. 2011;55:429–34.
Vohra A, Thomas AN, Harper NJ, Pollard BJ. Non-invasive measurement of cardiac output during induction of anaesthesia and tracheal intubation: thiopentone and propofol compared. Br J Anaesth. 1991;67:64–8.
Grounds RM, Twigley AJ, Carli F, Whitwam JG, Morgan M. The haemodynamic effects of intravenous induction. Comparison of the effects of thiopentone and propofol. Anaesthesia. 1985;40:735–40.
Kurokawa H, Murray PA, Damron DS. Propofol attenuates beta-adrenoreceptor-mediated signal transduction via a protein kinase C-dependent pathway in cardiomyocytes. Anesthesiology. 2002;96:688–98.
Rouby JJ, Andreev A, Leger P, Arthaud M, Landault C, Vicaut E, Maistre G, Eurin J, Gandjbakch I, Viars P. Peripheral vascular effects of thiopental and propofol in humans with artificial hearts. Anesthesiology. 1991;75:32–42.
Naguib M, Sari-Kouzel A, Seraj M, el-Gammal M, Gomma M. Induction dose-responses studies with propofol and thiopentone. Br J Anaesth. 1992;68:308–10.
Homer TD, Stanski DR. The effect of increasing age on thiopental disposition and anesthetic requirement. Anesthesiology. 1985;62:714–24.
Schnider TW, Minto CF, Shafer SL, Gambus PL, Andresen C, Goodale DB, Youngs EJ. The influence of age on propofol pharmacodynamics. Anesthesiology. 1999;90:1502–16.
Dundee JW, Robinson FP, McCollum JS, Patterson CC. Sensitivity to propofol in the elderly. Anaesthesia. 1986;41:482–5.
Rivera R, Antognini JF. Perioperative drug therapy in elderly patients. Anesthesiology. 2009;110:1176–81.
Steib A, Freys G, Beller JP, Curzola U, Otteni JC. Propofol in elderly high risk patients. A comparison of haemodynamic effects with thiopentone during induction of anaesthesia. Anaesthesia. 1988;43(Suppl):111–4.
Albertin A, Casati A, Federica L, Roberto V, Travaglini V, Bergonzi P, Torri G. The effect-site concentration of remifentanil blunting cardiovascular responses to tracheal intubation and skin incision during bispectral index-guided propofol anesthesia. Anesth Analg. 2005;101:125–30.
Joosten A, Desebbe O, Suehiro K, Murphy LS, Essiet M, Alexander B, Fischer MO, Barvais L, Van Obbergh L, Maucort-Boulch D, Cannesson M. Accuracy and precision of non-invasive cardiac output monitoring devices in perioperative medicine: a systematic review and meta-analysis. Br J Anaesth. 2017;118:298–310.
Ameloot K, Palmers PJ, Malbrain ML. The accuracy of noninvasive cardiac output and pressure measurements with finger cuff: a concise review. Curr Opin Crit Care. 2015;21:232–9.
Acknowledgements
The authors would like to thank Associate Professor Mitsuru Fukui (Laboratory of Statistics, Osaka City University Graduate School of Medicine, Osaka, Japan) for help with statistics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
540_2019_2657_MOESM1_ESM.tif
Figure S1 Hemodynamic changes in the propofol group (green line) and the thiopental group (red line) in each age group. (a) (g) (m) MAP, (b) (h) (n) heart rate, (c) (i) (o) cardiac index, (d) (j) (p) stroke volume index, (e) (k) (q) systemic vascular resistance index, (f) (l) (r) stroke volume variation for the young, middle, and elderly age groups, respectively (TIFF 245 kb)
About this article
Cite this article
Hino, H., Matsuura, T., Kihara, Y. et al. Comparison between hemodynamic effects of propofol and thiopental during general anesthesia induction with remifentanil infusion: a double-blind, age-stratified, randomized study. J Anesth 33, 509–515 (2019). https://doi.org/10.1007/s00540-019-02657-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-019-02657-x