Abstract
Purpose
Bioreactance is a non-invasive technology for measuring stroke volume (SV) in the operating room and critical care setting. We evaluated how the NICOM® bioreactance device performed against the CardioQ® esophageal Doppler monitor in patients undergoing major abdominal–pelvic surgery, focusing on the effect of different hemodynamic interventions.
Methods
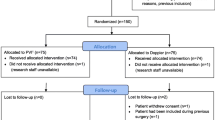
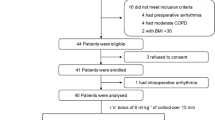
SVNICOM and SVODM were simultaneously measured intraoperatively, including before and after interventions including fluid challenge, vasopressor boluses, peritoneal gas insufflation/removal, and Trendelenburg/reverse Trendelenburg patient positioning.
Results
A total of 768 values were collected from 21 patients. Pre- and post-intervention measures were recorded on 155 occasions. Bland–Altman analysis revealed a bias of 8.6 ml and poor precision with wide limits of agreement (54 and −37 ml) and a percentage error of 50.6%. No improvement in precision was detected after taking into account repeated measurements for each patient (bias: 8 ml; limits of agreement: 74 and −59 ml). Concordance between changes in SVNICOM and SVODM before and after interventions was also poor: 78.7% (all measures), 82.4% (after vasopressor administration), and 74.3% (after fluid challenge). Using Doppler SV as the reference technique, the area under the receiver operating characteristic curve assessing the ability of the NICOM device to predict fluid responsiveness was 0.81 (0.7–0.9).
Conclusions
In patients undergoing major abdomino-pelvic surgery, SV values obtained by NICOM showed neither clinically or statistically acceptable agreement with those obtained by esophageal Doppler. Although, in the setting of this study, bioreactance technology cannot reliably replace esophageal Doppler monitoring, its accuracy for predicting fluid responsiveness was higher, up to approximately 80%.
Trial registration
Observational study.



Similar content being viewed by others
References
Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988;94:1176–86.
Boyd O, Grounds RM, Bennett ED. A randomized clinical trial of the effect of deliberate perioperative increase of oxygen delivery on mortality in high-risk surgical patients. JAMA. 1993;270:2699–707.
Saugel B, Cecconi M, Wagner JY, Reuter DA. Non-invasive continuous cardiac output monitoring in perioperative and intensive care medicine. Br J Anaesth. 2015;114:562–75.
Singer M. Oesophageal Doppler monitoring: should it be routine for high-risk surgical patients? Curr Opin Anaesthesiol. 2011;24:171–6.
Singer M. Oesophageal Doppler. Curr Opin Crit Care. 2009;15:244–8.
Dark PM, Singer M. The validity of trans-oesophageal Doppler ultrasonography as a measure of cardiac output in critically ill adults. Intensive Care Med. 2004;30:2060–6.
Tomlin PJ, Duck FA. Transoesophageal aortic velography in man. Can Anaesth Soc J. 1975;22:561–71.
Raval NY, Squara P, Cleman M, Yalamanchili K, Winklmaier M, Burkhoff D. Multicenter evaluation of noninvasive cardiac output measurement by bioreactance technique. J Clin Monit Comput. 2008;22:113–9.
Marqué S, Cariou A, Chiche JD, Squara P. Comparison between Flotrac-Vigileo and Bioreactance, a totally noninvasive method for cardiac output monitoring. Crit Care. 2009;13:R73.
Squara P, Rotcajg D, Denjean D, Estagnasie P, Brusset A. Comparison of monitoring performance of Bioreactance vs. pulse contour during lung recruitment manoeuvres. Crit Care. 2009;13:R125.
Conway DH, Hussain OA, Gall I. A comparison of noninvasive bioreactance with oesophageal Doppler estimation of stroke volume during open abdominal surgery: an observational study. Eur J Anaesthesiol. 2013;30:501–8.
Kupersztych-Hagege E, Teboul JL, Artigas A, Talbot A, Sabatier C, Richard C, Monnet X. Bioreactance is not reliable for estimating cardiac output and the effects of passive leg raising in critically ill patients. Br J Anaesth. 2013;111:961–6.
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15:85–91.
Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–60.
Critchley LA, Lee A, Ho AM. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111:1180–92.
Weisz DE, Jain A, McNamara PJ. EL-Khuffash A. Non-invasive cardiac output monitoring in neonates using bioreactance: a comparison with echocardiography. Neonatology. 2012;102:61–7.
Dunham CM, Chirichella TJ, Gruber BS, Ferrari JP, Martin JA, Luchs BA, Hileman BM, Merrell R. Emergency department noninvasive (NICOM) cardiac outputs are associated with trauma activation, patient injury severity and host conditions and mortality. J Trauma Acute Care Surg. 2012;73:479–85.
Cheung H, Dong Q, Dong R, Yu B. Correlation of cardiac output measured by non-invasive continuous cardiac output monitoring (NICOM) and thermodilution in patients undergoing off-pump coronary artery bypass surgery. J Anesth. 2015;29:416–20.
Waldron NH, Miller TE, Thacker JK, Manchester AK, White WD, Nardiello J, Elgasim MA, Moon RE, Gan TJ. A prospective comparison of a noninvasive cardiac output monitor versus esophageal Doppler monitor for goal-directed fluid therapy in colorectal surgery patients. Anesth Analg. 2014;118:966–75.
Huang L, Critchley LA, Zhang J. Major upper abdominal surgery alters the calibration of bioreactance cardiac output readings, the NICOM, when comparisons are made against suprasternal and oesophageal Doppler intraoperatively. Anesth Analg. 2015;121:936–45.
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL, Vincent JL, Rhodes A. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(12):1795–1815.
Cecconi M, Arulkumaran N, Kilic J, Ebm C, Rhodes A. Update on hemodynamic monitoring and management in septic patients. Minerva Anestesiol. 2014;80:701–11.
Author information
Authors and Affiliations
Contributions
Dr. De Pascale takes responsibility for the content of the manuscript, including the data and analysis. Dr. De Pascale and Dr. Brealey contributed to conception and design, acquisition of data, or analysis and interpretation of data; drafted the submitted article, revised it critically for important intellectual content and provided final approval of the version to be published. Prof Singer contributed to the design of the study, critically revised the paper for important intellectual content and provided final approval of the version to be published.
Corresponding author
Ethics declarations
Funding
No funding was received from either Deltex (CardioQ manufacturer) or Cheetah (NICOM manufacturer) for this study. NICOM electrodes were provided free for this evaluation by Cheetah.
Conflict of interest
Mervyn Singer sits on an advisory board for Deltex; his academic fund at UCL receives an annual unrestricted donation from Deltex. UCL also hold shares in Deltex donated by the Pauline Thomas Charitable Trust. He was not involved in the collection of data for this study. The other authors declare no conflict of interests regarding this study.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors. The monitoring, interventions and data collected were part of standard care. In addition, the analyzed data were fully anonymized and, as such, specific ethics committee permission was not required.
Informed consent
For this type of study formal consent was not required.
About this article
Cite this article
De Pascale, G., Singer, M. & Brealey, D. Comparison of stroke volume measurement between non-invasive bioreactance and esophageal Doppler in patients undergoing major abdominal–pelvic surgery. J Anesth 31, 545–551 (2017). https://doi.org/10.1007/s00540-017-2351-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-017-2351-1