Abstract
Purpose
We retrospectively investigated the incidence of postoperative nightmares and evaluated the impact of postoperative intensive care on the incidence of during subsequent hospital stay. To reduce the effect of selection bias, we compared the incidence of nightmares in propensity-matched pairs with postoperative management in ICUs or in surgical wards.
Methods
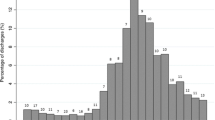
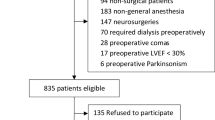
This is a retrospective review of an institutional registry containing 21,606 anesthesia cases and was conducted with ethics board approval. Outcomes of surgical patients treated in ICUs and in postsurgical wards (ICU admission vs non ICU admission) were compared first for nightmares using the initial 12,508 patients. To avoid channeling bias, propensity score analysis was used to generate a set of matched cases (ICU admission) and controls (non ICU admission), yielding 642 matched patient pairs. The incidence rate of nightmares was compared as the primary outcome.
Results
Before adjusting patients’ characteristics, ICU environment exposure increased the incidence of nightmares compared with non-ICU environment during subsequent hospital stay [ICU vs non-ICU: 101/718 (12.3 %) vs 1147/10,542 (9.81 %)]. The odds ratio (95 % CIs) for ICU was 1.29 (1.03–1.61) for nightmares (p = 0.022). After propensity score matching, however, an equal rate of nightmares occurred in the ICU environment exposure compared to the non-ICU environment [ICU vs non-ICU: 81/561 (12.6 %) vs 73/569 (11.4 %)]. The odds ratio and 95 % CIs for ICU were 1.13 (0.80–1.58) for nightmares (p = 0.54).
Conclusions
The incidence of nightmares did not become more evident during subsequent hospital stay after ICU environment exposure.

Similar content being viewed by others
References
McGuire BE, Basten CJ, Ryan CJ, Gallagher J. Intensive care unit syndrome: a dangerous misnomer. Arch Intern Med. 2000;160:906–9.
Roberts B, Chaboyer W. Patients’ dreams and unreal experiences following intensive care unit admission. Nurs Crit Care. 2004;9:173–80.
Rundshagen I, Schnabel K, Wegner C, am Esch S. Incidence of recall, nightmares, and hallucinations during analgosedation in intensive care. Intensive Care Med. 2002;28:38–43.
Reynolds CF III, O’Hara RM, Morin CM, Pack AI, Parker KP, Redine S Riemann D. Nightmare disorder. In: The DSM-5 task force. Diagnostic and statistical manual of mental disorders, 5th ed. Virginia: American Psychiatric Association; 2013. p. 404–7.
Eagle KA, Berger PB, Calkins H, Chaitman BR, Ewy GA, Fleischmann KE, Fleisher LA, Froehlich JB, Gusberg RJ, Leppo JA, Ryan T, Schlant RC, Winters WL Jr, Gibbons RJ, Antman EM, Alpert JS, Faxon DP, Fuster V, Gregoratos G, Jacobs AK, Hiratzka LF, Russell RO, Smith SC Jr, American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). Circulation. 2002;105:1257–67.
Devlin JW, Fong JJ, Fraser GL, Riker RR. Delirium assessment in the critically ill. Intensive Care Med. 2007;33:929–40.
Girard TD, Pandharipande PP, Ely EW. Delirium in the intensive care unit. Crit Care. 2008;12(Suppl 3):S3.
Banh HL. Management of delirium in adult critically ill patients: an overview. J Pharm Pharm Sci. 2012;15:499–509.
Austin PC. Propensity-score matching in the cardiovascular surgery literature from 2004 to 2006: a systematic review and suggestions for improvement. J Thorac Cardiovasc Surg. 2007;134:1128–35.
Austin PC, Grootendorst P, Anderson GM. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med. 2007;26:734–53.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9.
Knauert MP, Haspel JA, Pisani MA. Sleep loss and circadian rhythm disruption in the intensive care unit. Clin Chest Med. 2015;36:419–29.
Pisani MA, Friese RS, Gehlbach BK, Schwab RJ, Weinhouse GL, Jones SF. Sleep in the intensive care unit. Am J Respir Crit Care Med. 2015;191:731–8.
Pick J, Chen Y, Moore JT, Sun Y, Wyner AJ, Friedman EB, Kelz MB. Rapid eye movement sleep debt accrues in mice exposed to volatile anesthetics. Anesthesiology. 2011;115:702–12.
Krishnan V, Collop NA. Gender differences in sleep disorders. Curr Opin Pulm Med. 2006;12:383–9.
Been H. Dreams: the convergence of neurobiologic and psychoanalytic perspectives. J Am Acad Psychoanal. 1997;25:639–54.
Jones C, Griffiths RD, Humphris G. Disturbed memory and amnesia related to intensive care. Memory. 2000;8:79–94.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Sonobe, S., Inoue, S. & Kawaguchi, M. The effects of intensive care environment on postoperative nightmare. J Anesth 30, 970–976 (2016). https://doi.org/10.1007/s00540-016-2237-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-016-2237-7