Abstract
Purpose
We evaluated the hemodynamic and respiratory effects of dexmedetomidine in intubated, spontaneously breathing patients after endoscopic submucosal dissection (ESD) for cervical esophageal or pharyngeal cancer.
Methods
This retrospective study included 129 patients aged 66.5 ± 8.3 years, who underwent ESD under general anesthesia, and who were kept intubated overnight to prevent airway obstruction, receiving sedation with dexmedetomidine. Constant dexmedetomidine infusion at 0.51 ± 0.16 μg/kg/h was started intraoperatively (n = 109) or postoperatively (n = 20), following (n = 29) or not following (n = 100) loading doses, and continued until extubation. Hemodynamic and respiratory variables, and Richmond Agitation-Sedation Scale (RASS) score, were recorded.
Results
Postoperatively, 129 patients remained intubated while breathing spontaneously for 16.4 ± 3.3 h, and 124 patients could be sedated solely with dexmedetomidine, whereas 5 required rescue sedatives. During infusion, blood pressure decreased progressively until 12 h, whereas heart rate decreased only at 3 h. Hemodynamic alterations during dexmedetomidine infusion greatly depended not only on its hemodynamic effects but also on baseline hemodynamics before anesthesia. No serious adverse effect was noted.
Conclusion
Dexmedetomidine in intubated, spontaneously breathing patients after ESD was safe and effective. Patient baseline hemodynamics could significantly affect hemodynamics during drug infusion. Without loading doses, plasma drug concentrations were expected to increase progressively. A progressive decrease in blood pressure and unchanged heart rate after an initial decrease suggested that hemodynamic effects of dexmedetomidine in our patients might differ from those reported in young volunteers, although further studies are required to elucidate these points.
Similar content being viewed by others
Introduction
Endoscopic submucosal dissection (ESD), when compared with conventional endoscopic mucosal resection (EMR) for early esophageal cancer, has considerable advantages regarding the en bloc resection rate, complete resection rate, and local recurrence rate [1, 2]. Therefore, EMR has been replaced by ESD for the treatment of early esophageal cancer. However, ESD requires higher skill levels of the endoscopists, a more complicated intervention, and a longer procedure time compared with EMR [1, 2]. Therefore, at some institutions, ESD is performed under general anesthesia to reduce the discomfort of patients, to shorten the procedure time, and to decrease the risk of complications such as perforation [3–5].
At our institution, ESD for early esophageal or pharyngeal cancer is commonly performed under general anesthesia. In addition, in patients whose cervical esophageal or pharyngeal cancer is located quite close to the airway, the tracheal tube is left in place overnight to protect the airway from possible obstruction caused by airway edema. Postoperatively, patients are allowed to breathe spontaneously via the tracheal tube while being sedated in the intensive care unit (ICU). Previously, we used propofol to sedate such patients. However, propofol, which is associated with dose-dependent respiratory depression [6, 7], caused significant respiratory depression in some patients. Therefore, in 2007, we began to use dexmedetomidine, which is associated with less respiratory depression [6, 7].
Previous studies showed that dexmedetomidine was not inferior to propofol or midazolam in maintaining light to moderate sedation in mechanically ventilated patients [8, 9]. A previous study showed that dexmedetomidine was as efficacious as propofol in intubated patients after extensive cervical spine surgery whose spontaneous breathing was supported by pressure support ventilation [10]. However, no study has been conducted to evaluate the effects of dexmedetomidine in intubated patients after ESD who are just spontaneously breathing without any ventilatory support. We conducted the present study to evaluate effects of dexmedetomidine on hemodynamics and respiration in intubated, spontaneously breathing patients after ESD.
Methods
Before this retrospective study, approval was obtained from the institutional review board (IRB) of Juntendo University Hospital. Because of the anonymous and retrospective fashion of this study, the IRB waived the need for patient consent.
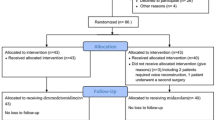
From May 2007 to December 2015, 244 patients underwent ESD for cervical esophageal or pharyngeal cancer under general anesthesia. Among them, 98 patients were extubated in the operating room (OR), whereas 146 patients with surgical sites very close to the airway were not extubated and were transferred to the intensive care unit (ICU), receiving continuous infusion of dexmedetomidine alone (n = 131) or with other sedatives such as propofol, midazolam, or a combination of dexmedetomidine and fentanyl (n = 15). Primarily, surgeons decided whether patients were likely to be extubated safely in the OR, depending on the site of ESD relative to the airway, before, during, or after surgery.
In the first step, 98 patients who were extubated in the OR were excluded. In the second step, 15 patients who received sedatives other than dexmedetomidine alone were excluded. In the third step, 2 patients who received dexmedetomidine alone but for less than 12 h were excluded. Consequently, 129 patients who were sedated with dexmedetomidine alone, at least initially, and for at least 12 h in the ICU were included in this study (Table 1).
No patient was premedicated. After baseline measurements of the heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and percutaneous oxygen saturation (SpO2), general anesthesia was induced with propofol and remifentanil and/or fentanyl. Rocuronium was used to facilitate orotracheal intubation. Anesthesia was maintained with sevoflurane and remifentanil (n = 108), desflurane and remifentanil (n = 14), sevoflurane and fentanyl (n = 4), and propofol and remifentanil (n = 3). When the surgeon decided the nonextubation policy, infusion of dexmedetomidine was initiated. After anesthesia, patients were allowed to breathe spontaneously via the tracheal tube left in place, and transferred to the ICU. In the ICU, patients spontaneously breathed oxygen-enriched air via a T-piece system (TRACH-VENT and OXY-VENT; Teleflex Medical Japan, Tokyo) without any ventilatory support. Constant infusion of dexmedetomidine was continued until extubation. Hemodynamic variables (HR, SBP, DBP) and respiratory variables [SpO2 and the respiratory rate (RR)] were measured every hour, but these variables were measured every 3 h during the dark period (2100–600). The Richmond Agitation-Sedation Scale (RASS) (+4, combative; +3, very agitated; +2, agitated; +1, restless; 0, alert and calm; −1, drowsy; −2, lightly sedated; −3, moderately sedated; −4, deeply sedated; −5, unarousable) [11] and a 5-point verbal rating pain scale (VRS) (0, no pain; 1, mild pain; 2, moderate pain; 3, severe pain; 4, intolerable pain) were assessed every 3 h. The patients were extubated on the first postoperative day after surgeons endoscopically confirmed the patency of the upper airway. Drug infusion was discontinued upon extubation.
Effectiveness of dexmedetomidine was assessed primarily based on change in RASS scores during tracheal intubation. Safety of dexmedetomidine was evaluated by noticing adverse events, such as hypotension (SBP <80 mmHg), hypertension (SBP >160 mmHg), bradycardia (HR <40 bpm), tachycardia (HR >100 bpm), bradypnea (RR <10 bpm), and desaturation (SpO2 <95 %). Criteria for defining these adverse events were based on our surgeons’ indications to the nurses that doctors should be called in the event. The estimated plasma dexmedetomidine concentration after entering the ICU was calculated based on Dyck’s pharmacokinetic model [12].
Data are expressed as the mean ± SD and range, or the median, percentiles, and range, according to data types. Changes in RASS scores, VRS scores, and SpO2 were analyzed with the Wilcoxon signed-rank test with the Bonferroni correction. Changes in SBP, DBP, HR, and RR were analyzed with repeated-measures analysis of variance (ANOVA) with Bonferroni correction. To evaluate correlation between any two variables, a simple linear regression analysis was used. To evaluate effects of the use or non-use of initial loading doses on RASS scores, ANOVA was used. Values of P < 0.05 were considered statistically significant, unless otherwise stated. All data analyses were performed with SPSS ver. 19 software package (SPSS Japan, Tokyo, Japan).
Results
The demographic, anesthetic, and surgical data of 129 patients are shown in Table 1. Complications of ESD occurred in 14 patients, including subcutaneous emphysema (n = 4), minor bleeding (n = 1), neck swelling and pain (n = 1), and upper airway edema, which could postpone extubation for several hours (n = 8). However, no patient needed special treatment for these self-limited complications.
Infusion of dexmedetomidine was initiated intraoperatively, 69 ± 66 (1–284) min before ending surgery (n = 109); or postoperatively, 8.5 ± 5.5 (3–20) min after ending surgery (n = 20), depending on the time when surgeons decided the nonextubation policy. Overall, dexmedetomidine infusion was initiated 89.1 ± 66.9 (10–309) min before entering the ICU. A loading dose was used in 29 patients, including 6 µg/kg/h for 10 min (n = 13), 3 µg/kg/h for 20 min (n = 3), and 1 µg/kg/h for 60–120 min (n = 13), whereas it was not used in 100 patients. The initial maintenance dose of dexmedetomidine was 0.505 ± 0.164 (0.20–1.01) μg/kg/h. At the end of anesthesia, fentanyl [106 ± 48 (25–250) µg] was given to 68 patients for immediate postoperative analgesia, whereas it was not given to 61 patients.
All 129 patients remained intubated for 16.4 ± 3.3 h (12.0–23.5 h) in the ICU. Dexmedetomidine infusion was continued throughout the intubation period in all 129 patients. However, in 21 patients, a drug dose was increased to augment sedation, whereas in 7 patients, it was decreased for adjustment of too-high doses (>0.8 μg/kg/h) (n = 2) and because of bradycardia (n = 4) and hypotension (n = 1). Consequently, the initial and final doses in the ICU were 0.505 ± 0.164 (0.20–1.01) μg/kg/h and 0.526 ± 0.178 (0.18–1.00) μg/kg/h, respectively. Total duration of drug infusion in the OR and ICU was 17.9 ± 3.5 h (12.5–26.5 h). During infusion, the estimated dexmedetomidine plasma concentration increased progressively as follows: 0.32 ± 0.14 (0.10–0.60), 0.54 ± 0.14 (0.33–0.80), 0.72 ± 0.19 (0.47–1.07), 0.86 ± 0.23 (0.57–1.27), 0.95 ± 0.24 (0.63–1.42), and 1.00 ± 0.26 (0.63–1.67) ng/ml at 0, 3, 6, 9, 12, and 16 ± 3 (12.0–23.5) h, respectively. Rescue sedatives in addition to dexmedetomidine were required in 5 patients (3.9 %), including propofol (n = 4) and midazolam (n = 1). Therefore, 124 patients (96.1 %) could be sedated with dexmedetomidine alone until extubation.
RASS scores were significantly less at 6 and 9 h compared with 0, 3, and 16 ± 3 h (P < 0.0033) (Fig. 1a). RASS scores were 0 or less in 117 (90.7 %), 117 (90.7 %), 126 (97.7 %), 125 (96.9 %), 123 (95.3 %), and 122 (94.6 %) of 129 patients at 0, 3, 6, 9, 12, and 16 ± 3 h, respectively. Using regression analysis or ANOVA, no determinant factor significantly correlating with RASS scores could be identified, including the use or non-use of loading doses, maintenance doses, duration of drug infusion, and accumulated drug doses.
Changes in Richmond Agitation-Sedation Scale (RASS) (a), 5-point verbal rating pain scale (b), percutaneous oxygen saturation (SpO2) (c), respiratory rate (d), heart rate (e), and systolic and diastolic blood pressures (f) before and/or during dexmedetomidine infusion. Data are shown in median (bar), quartiles (box), 10th and 90th percentiles (whiskers), and range (open circles) (a–c), or mean ± SD (d– f). *P < 0.0033 versus 0, 3, and 16 ± 3 h (a), # P < 0.0024 versus 0, 3, 6, 9, 12, and 16 ± 3 h (c), $ P < 0.0024 versus baseline and 0 h (e), and & P < 0.0024 versus a previous value 3 h earlier (f). BL baseline before induction general anesthesia in the operating room
Five-point VRS pain scores were recorded in 99 patients. The median VRS pain score was 0 (no pain) throughout drug infusion, but 35–40 patients reported pain at each assessment time (Fig. 1b). Analgesics were required in 43 patients, including pentazocine (15 mg) in 28 patients [once (n = 15), twice (n = 8), three times (n = 4), four times (n = 1)], pethidine (50 mg) in 8 patients [once (n = 5), twice (n = 2), three times (n = 1)], and fentanyl (100 µg) in 7 patients [once (n = 4), twice (n = 1), three times (n = 2)]. Of note, surgeons preferring pentazocine indicated that pain should be treated with pentazocine (15 mg) alone during the light period (600–2100) but should be treated with a combination of pentazocine (15 mg) and hydroxyzine hydrochloride (25 mg) during the dark period (2100–600). Consequently, hydroxyzine was given in 24 patients once (n = 18) or twice (n = 6) during the dark period, although RASS scores were 0 or less in 22 patients even before hydroxyzine was given.
After entering the ICU, patients breathed oxygen-enriched air via a T-piece system, which could provide fractions of inspiratory oxygen (FiO2) of 0.24 to 0.40 at an oxygen flow rate of 1–6 l/min in the standard respiratory condition, according to the manufacturer’s instruction. The initial and final oxygen flow rates during intubation were 3.1 ± 1.1 (3–6) l/min and 2.9 ± 1.1 (0–6) l/min, respectively, which corresponded to estimated FiO2 of 0.319 ± 0.034 (0.24–0.40) and 0.314 ± 0.034 (0.21–0.40), respectively. The arterial blood oxygen tension (PaO2), PaO2/FiO2 ratio, and carbon dioxide tension (PaCO2), measured shortly after entering the ICU, were 143.4 ± 35.0 (80.6–219.0), 442.0 ± 103.8 (230–626), and 44.5 ± 5.6 (25.8–56.4) mmHg, respectively (n = 113), whereas those values measured immediately before extubation were 139.9 ± 32.8 (59.1–235.1), 446.8 ± 99.1 (201–641), and 42.6 ± 4.2 (31.6–52.6) mmHg, respectively (n = 108).
SpO2 remained at 95 % or more throughout drug infusion in all but three patients with lung disease, who recorded SpO2 of 93 % or 94 % transiently or intermittently, but SpO2 in the ICU was always higher than that at baseline in the OR and remained unchanged in the ICU (Fig. 1c). Otherwise, no episode of significant desaturation was documented. The RR remained unchanged throughout drug infusion (Fig. 1d), and no patient experienced bradypnea. All patients could be extubated uneventfully on the first postoperative day.
HR decreased significantly at 3 h through 16 ± 3 h, compared with baseline before induction of general anesthesia (P < 0.0024), and compared with 0 h in the ICU (P < 0.0024), but remained unchanged after 3 h (Fig. 1e). SBP and DBP decreased significantly at 3 h through 16 ± 3 h, compared with baseline and 0 h (P < 0.0024). During drug infusion, SBP and DBP decreased progressively until 12 h, but they did not decrease further afterward (Fig. 1f).
Hemodynamic alterations occurred in 45 patients (34.9 %), including hypertension (n = 25), bradycardia (n = 11), hypotension (n = 10), and/or tachycardia (n = 3). Hypertension was noticed in 28, 18, 8, 4, 1, 1, and 0 of 129 patients at baseline, 0, 3, 6, 9, 12, and 16 ± 3 h, respectively. It was noted during the first 6 ICU hours in 23 patients, while being newly noted at 9 h or later in 2 patients. Hypertension was just observed (n = 9) or treated with isosorbide dinitrate tape (40 mg) (n = 9). Tachycardia was noted in 7, 3, and 2 patients at baseline, 0 h, and 3 h, respectively. Tachycardia was just observed. Bradycardia, occurring at 6 h or later in 11 patients, was just observed in all patients, although drug doses were reduced in 4 patients. Hypotension, occurring at 9 h or later in 10 patients, were treated just by raising patients’ legs for all patients, although a drug dose was reduced in one patient.
There was no significant correlation between any hemodynamic variable and a RASS score at each assessment time. In contrast, there was a significant correlation between a baseline hemodynamic variable in the OR and that in the ICU at each assessment time (Figs. 2, 3).
Correlation between blood pressure (BP) at baseline before induction of general anesthesia and BP at 0 h (a), 3 h (b), 6 h (c), 9 h (d), 12 h (e), or 16 ± 3 h (f) in the intensive care unit. Black closed circles indicate systolic blood pressure (SBP); gray open circles indicate diastolic blood pressure (DBP)
Discussion
In this study, 96.1 % of intubated, spontaneously breathing patients after ESD could be sedated solely with dexmedetomidine during the intubation period over 16.4 ± 3.3 h. In addition, 90.7–97.7 % of patients remained calm or sedated at each assessment time. Although minor hemodynamic alterations were observed, dexmedetomidine infusion could be continued until extubation in all 129 patients. Further, respiratory depression did not occur in any patients. Our data suggested that sedation with dexmedetomidine was safe and effective in intubated, spontaneously breathing patients after ESD.
In general, the use of initial loading doses is recommended to facilitate increases in plasma dexmedetomidine concentrations. When a drug is infused at a constant rate without a loading dose, plasma concentration increases exponentially over time until it reaches 97 % of steady-state plasma concentration after five elimination half-lives [13]. Because the elimination half-life of dexmedetomidine is 2–3 h [14–17], the time to reach steady-state concentration will be 10–15 h. Actually, by omitting loading doses in many patients (n = 100), the mean estimated plasma concentration progressively increased from 0.32 ng/ml at 0 h to 0.95 ng/ml at 12 h. Without loading doses in many patients, sufficient sedative effects could be achieved in a majority of patients, probably because postoperative pain was generally mild after ESD, mechanical ventilation associated with bucking was not used, and patients undergoing ESD were older in age, compared with volunteers in previous studies [7, 15, 18]. Although earlier studies found no effect of age on pharmacokinetics of dexmedetomidine [12, 19], recent studies reported a prolonged elimination half-life in the elderly, thereby recommending reduced dosing [17, 20]. Further, ED95 of a single dose of dexmedetomidine for achieving light sedation was 33 % lower in the older patients compared to young patients, suggesting a pharmacodynamic difference by age [21]. Because our patients were relatively old in age, it was probable that small doses without loading doses could induce adequate sedation. Successful sedation with dexmedetomidine without loading doses has been reported previously [22, 23].
Previous studies showed that sedative effects of dexmedetomidine increased progressively as actual or target plasma drug concentrations increased from 0.1 to 5.1 ng/ml in a stepwise fashion in volunteers [7, 15, 18]. The threshold concentration for inducing sedation was 0.1 or 0.2 ng/ml depending on sedation assessment methods [18]. In our study, RASS scores decreased significantly only at 6 and 9 h, compared with 0 h, indicating RASS scores did not decrease progressively, although plasma concentrations were expected to increase progressively. The reasons for this discrepancy were not clear. However, it was plausible that RASS scores did not decrease significantly at 3 h, compared with 0 h, because RASS scores at 0 h, assessed shortly after the end of anesthesia, might have been affected by residual effects of anesthetics and/or fentanyl given in the OR. In contrast, significantly decreased RASS scores at 6 and 9 h might reflect a progressive increase in drug concentrations. In addition, a light–dark cycle might also contribute to decreased RASS at 6 and 9 h. In many patients, 6 and 9 h in the ICU corresponded to a relatively silent, dark period, which could facilitate patients’ natural sleep. Conversely, in most patients, 12 h or later corresponded to a relatively noisy, light period, when patients underwent many interventions, such as blood examinations, oral and tracheal suctioning, and endoscopic examinations, in preparation for extubation, all of which might easily arouse patients under dexmedetomidine sedation. Further, not only opioid analgesics given in 43 patients but also hydroxyzine coadministered with pentazocine only during the dark period in 24 patients might affect sedation levels. These reasons might explain why RASS scores did not decrease progressively although drug concentrations were expected to increase progressively.
In this study, clinically relevant respiratory depression occurred in none of the patients. The alpha-2 adrenoceptor does not have an active role in the respiratory center [24]. Actually, many studies have reported that dexmedetomidine did not cause clinically relevant adverse effects on respiration [6, 7, 15, 18, 25]. The present study reconfirmed the safety aspect of dexmedetomidine regarding respiration in intubated, spontaneously breathing patients without any ventilator support.
In this study, HR decreased significantly at 3 h, compared with 0 h, but it remained unchanged afterward. In contrast, SBP and DBP decreased progressively until 12 h. Previous studies in human volunteers showed that HR decreased progressively as plasma drug concentrations increased progressively from low (0.1 ng/ml) to high (5.1 ng/ml) levels, whereas changes in blood pressure (BP) were biphasic; as concentrations increased progressively, BP initially decreased dose dependently in a low concentration range (0.1–0.5 ng/ml), but it remained unchanged in an intermediate concentration range (0.5–1.2 ng/ml), and increased back toward or beyond baseline BP dose dependently in a high concentration range (1.2–5.1 ng/ml) [15, 18]. Results of our study seemed to somewhat differ from those in volunteers [15, 18], in that BP continued to decrease until 12 h, although the mean estimated drug concentration had already reached the intermediate concentration range by 6 h, and in that HR did not decrease progressively while the mean estimated concentration increased progressively. These differences might be attributable to changes in the autonomic systems with aging, which include an increase in sympathetic nerve activity and a decrease in response to β-adrenoceptor stimulation secondary to both decreased β-receptor affinity and alterations in signal transduction [26, 27]. Reportedly, a low concentration of dexmedetomidine predominantly induces centrally mediated sympatholytic effects, thereby resulting in hypotension, whereas a high concentration predominantly induces α2-adrenoceptor-mediated vasoconstrictions, thereby resulting in hypertension [15]. Increased resting sympathetic nervous system activity with aging may be associated with the exquisite sensitivity of older patients to interventions that decrease sympathetic tone [26–28]. Such alterations with aging might explain why BP continued to decrease in our patients, in contrast to young volunteers [15, 18]. Further, although dexmedetomidine-induced slowing of HR is attributed to sympatholysis and a possible increase in cardiac vagal activity [15], older patients with decreased β-adrenoceptor responsiveness [26, 27] might mimic patients taking β-blockers who did not experience HR slowing when receiving dexmedetomidine [29]. This result might explain why our patients did not exhibit progressive decreases in HR with increasing concentrations, again contrasting with young volunteers [15, 18]. Results of our study suggested that the hemodynamic effects of dexmedetomidine observed in our patients might somewhat differ from those observed in young volunteers.
In this study, hemodynamic alterations occurred in 47 patients (36.4 %). Previous studies showed that the most common side effects of dexmedetomidine were bradycardia and hypotension [30]. In our study, however, hypertension was the most common hemodynamic alteration observed in 25 patients. Because continuous infusion was started without loading doses in many patients and hypertension was most commonly observed within 6 h in 23 patients, one may argue that plasma concentrations of dexmedetomidine had not reached a therapeutic concentration to induce adequate sedation, thereby resulting in initial hypertension and tachycardia as manifestations of stress responses to discomfort from the tracheal tube and/or postoperative pain. However, BP and HR at 0 h in the ICU were no higher than those at baseline before the induction of general anesthesia, and the number of patients who were hypertensive (n = 18) and/or tachycardic (n = 3) at 0 h was no greater than that of patients who were hypertensive (n = 28) and/or tachycardic (n = 7) at baseline in the OR. These results suggested that under sedation with dexmedetomidine, stress responses at 0 h in the ICU were no greater than stress responses caused by mental strains in the OR. In addition, there was no correlation between any hemodynamic variable and RASS score at each assessment time, again suggesting that neither hypertension nor tachycardia was associated with inadequate sedation. In our study, initial BP and HR in the ICU significantly correlated with those at baseline in the OR. These results suggested that initial hypertension and tachycardia could be interpreted merely as a reflection of patient baseline hemodynamics. Such significant correlations persisted throughout the drug infusion period, indicating that baseline hemodynamics continued to exert a significant impact on hemodynamics during drug infusion. Thus, initial hypertension (n = 23) and tachycardia (n = 3) were not attributable to effects of dexmedetomidine, although late-onset hypertension (n = 2) might result from dexmedetomidine-induced vasoconstriction [15].
On the other hand, bradycardia and hypotension as occurring in 11 and 10 patients, respectively, at 6 h or later were probably attributable to effects of dexmedetomidine. However, bradycardia and hypotension were minor events not requiring active pharmacological intervention or discontinuation of drug infusion. Our findings were in agreement with previous authors’ summary that although dexmedetomidine was associated with hypotension and bradycardia, both usually resolved without intervention [30].
There are limitations of this study. First, we could not find any dose–response relationships between drug doses and RASS scores, probably because many clinical factors other than drug doses could affect RASS scores. Second, we did not measure actual plasma drug concentrations, and thus we could not reach any definite conclusions regarding concentration–effect relationships. Further studies are required to determine the optimal dosing protocol in our patient population and to clarify the effects of actual plasma drug concentrations on hemodynamics in the elderly.
In conclusion, sedation with dexmedetomidine in intubated, spontaneously breathing patients after ESD was safe and effective. Hemodynamic alterations during dexmedetomidine infusion greatly depended not only on hemodynamic effects of dexmedetomidine but also on baseline hemodynamics before anesthesia. Without loading doses in many patients, plasma drug concentrations were expected to increase progressively. A progressive decrease in blood pressure and unchanged heart rate after an initial decrease suggested that hemodynamic effects of dexmedetomidine in our patients might somewhat differ from those reported in young volunteers, although further studies are required to elucidate these points.
References
Kume K. Endoscopic mucosal resection and endoscopic submucosal dissection for early gastric cancer: current and original devices. World J Gastrointest Endosc. 2009;1:21–31.
Gotoda T, Jung HY. Endoscopic resection (endoscopic mucosal resection/endoscopic submucosal dissection) for early gastric cancer. Dig Endosc. 2013;25(suppl 1):55–63.
Rong QH, Zhao GL, Xie JP, Wang LX. Feasibility and safety of endoscopic submucosal dissection of esophageal or gastric carcinomas under general anesthesia. Med Princ Pract. 2013;22:280–4.
Suzuki T, Minami H, Komatsu T, Masusda R, Kobayashi Y, Sakamoto A, Sato Y, Inoue H, Serada K. Prolonged carbon dioxide insufflation under general anesthesia for endoscopic submucosal dissection. Endoscopy. 2010;42:1021–9.
Mori H, Kobara H, Muramatsu A, Inoue H, Kobayashi M, Nomura T, Hagiike M, Izuishi K, Suzuki Y, Gong J, Masaki T, et al. Comparison of postoperative complications after endoscopic submucosal dissection: differences of insufflations and anesthesias. Diagn Ther Endosc. 2011;2011:709237.
Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, Davidson JE, Devlin JW, Kress JP, Joffe AM, Coursin DB. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41:263–306.
Kasuya Y, Govinda R, Rauch S, Mascha EJ, Sessler DI, Turan A. The correlation between bispectral index and observational sedation scale in volunteers sedated with dexmedetomidine and propofol. Anesth Analg. 2009;109:1811–5.
Riker RR, Shehabi Y, Bokesch PM, Ceraso D, Wisemandle W, Koura F, Whitten P, Margolis BD, Byrne DW, Ely EW, Rocha MG. Dexmedetomidine vs. midazolam for sedation of critically ill patients: a randomized trial. JAMA. 2009;301:489–99.
Jakob SM, Ruokonen E, Grounds RM, Sarapohja T, Garratt C, Pocock SJ, Bratty JR, Takala J. Dexmedetomidine vs. midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA. 2012;307:1151–60.
Terao Y, Ichinomiya T, Higashijima U, Tanise T, Miura K, Fukusaki M, Sumikawa K. Comparison between propofol and dexmedetomidine in postoperative sedation after extensive cervical spine surgery. J Anesth. 2012;26:179–86.
Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, Francis J, Speroff T, Gautam S, Margolin R, Sessler CN. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA. 2003;289:2983–91.
Dyck JB, Maze M, Haack C, Azarnoff DL, Vuorilehto L, Shafer SL. Computer-controlled infusion of intravenous dexmedetomidine hydrochloride in adult human volunteers. Anesthesiology. 1993;78:821–8.
Sikka PK. Basic pharmacologic principles. In: Stoelting RK, Miller RD, editors. Basics of anesthesia, 5th edn. 5th ed. Philadelphia: Churchill-Livingstone; 2007. p. 37–48.
Hall JE, Uhrich TD, Barney JA, Arain SR, Ebert TJ. Sedative, amnestic, and analgesic property of small-dose dexmedetomidine infusions. Anesth Analg. 2000;90:699–705.
Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000;93:382–94.
Venn RM, Karol MD, Grounds RM. Pharmacokinetics of dexmedetomidine infusions for sedations of postoperative patients requiring intensive care. Br J Anaesth. 2002;88:669–75.
Iirola T, Ihmsen H, Laitio R, Kentala E, Aantaa R, Kurvinen JP, Scheinin M, Schwilden H, Schüttler J, Olkkola KT. Population pharmacokinetics of dexmedetomidine during long-term sedation in intensive care patients. Br J Anaesth. 2012;108:460–8.
Angst MS, Ramaswamy B, Davies MF, Maze M. Comparative analgesic and mental effects of increasing plasma concentrations of dexmedetomidine and alfentanil in humans. Anesthesiology. 2004;101:744–52.
Lin L, Guo X, Zhang MZ, Qu CJ, Sun Y, Bai J. Pharmacokinetics of dexmedetomidine in Chinese post-surgical intensive care unit patients. Acta Anaesthesiol Scand. 2011;55:359–67.
Kuang Y, Zhang RR, Pei Q, Tan HY, Guo CX, Huang J, Xiang YX, Ouyang W, Duan KM, Wang SY, Yang GP. Pharmacokinetic and pharmacodynamic study of dexmedetomidine in elderly patients during spinal anesthesia. Int J Clin Pharmacol Ther. 2015;53:1005–14.
Kim J, Kim WO, Kim HB. Adequate sedation with single-dose dexmedetomidine in patients undergoing transurethral resection of the prostate with spinal anaesthesia: a dose–response study by age group. BMC Anesthesiol. 2015;15:17.
Ickeringill M, Shehabi Y, Adamson H, Ruettimann U. Dexmedetomidine infusion without loading dose in surgical patients requiring mechanical ventilation: haemodynamic effects and efficacy. Anaesth Intensive Care. 2004;32:741–5.
Fujita Y, Inoue K, Sakamoto T, Yoshizawa T, Tomita M, Maeda Y, Taka H, Muramatsu A, Hattori Y, Hirate H, Toyóoka T. A comparison between dosages and plasma concentrations of dexmedetomidine in clinically ill patients: a prospective, observational, cohort study in Japan. J Intensive Care. 2013;1:15.
Eisenach JC, Lysak SZ, Viscomi CM. Epidural clonidine analgesia following surgery: phase I. Anesthesiology. 1989;71:640–6.
Venn RM, Hell J, Grounds RM. Respiratory effects of dexmedetomidine in the surgical patient requiring intensive care. Crit Care. 2000;4:302–8.
Rooke GA. Autonomic and cardiovascular function in the geriatric patients. Anesthesiol Clin N Am. 2000;18:31–46.
Rooke GA. Cardiovascular aging and anesthetic implications. J Cardiothorac Vasc Anesth. 2003;17:512–23.
Priebe HJ. The aged cardiovascular risk patients. Br J Anaesthesiol. 2000;85:763–78.
Jalonen J, Hynynen M, Kuitunen A, Heikkila H, Perttila J, Salmenpera M, Valtonen M, Aantaa R, Kallio A. Dexmedetomidine as an anesthetic adjunct in coronary artery bypass grafting. Anesthesiology. 1997;86:331–45.
Hoy SM, Keating GM. Dexmedetomidine: a review of its use for sedation in mechanically ventilated patients in an intensive care setting and for procedural sedation. Drugs. 2011;71:1481–501.
Acknowledgments
We thank all the staff for their valuable assistance in conducting the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This research received no specific grants from any funding agency in the public, commercial, or not-for-profit sectors.
About this article
Cite this article
Ishibashi, C., Hayashida, M., Sugasawa, Y. et al. Effects of dexmedetomidine on hemodynamics and respiration in intubated, spontaneously breathing patients after endoscopic submucosal dissection for cervical esophageal or pharyngeal cancer. J Anesth 30, 628–636 (2016). https://doi.org/10.1007/s00540-016-2175-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-016-2175-4