Abstract
Purpose
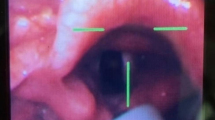
Inexperienced physicians frequently have difficulty performing nasal fiberoptic intubation. A pre-inserted tracheal tube of the appropriate length allows an excellent view of the laryngeal opening. The purpose of this study was to determine the ideal length of a pre-inserted tracheal tube for nasal fiberoptic intubation and to investigate if it could be predicted from easily measureable patient parameters.
Methods
This was an observational study in which data on adult patients (n = 150) requiring nasal intubation were collected and analyzed by stepwise regression. During the pre-anesthesia examination, a right-angled gauge was used to measure the distance from the mid-point of the lateral border of the nares to the tragus of the ear (NT distance) and to the mandibular angle (NM distance). The distance from the tragus to the mandibular angle (TM distance) was also measured. The age, sex, height, and weight of each patient were recorded. After induction of anesthesia, the minimum and maximum lengths of the pre-inserted tracheal tube that provided an excellent view of laryngeal opening during nasal fiberoptic intubation were measured. The optimal length was calculated, and an equation was derived through stepwise regression analysis.
Results
The optimal length for each patient could be reliably predicted using the equation (distances in cm, weight in kg): optimal length (cm) = 1.952 + 0.051 × height (cm) + 0.354 × NM distance (cm) − 0.011 × weight (kg) (r 2 = 0.460, P < 0.001).
Conclusion
The optimal length of pre-inserted tracheal tube for nasal fiberoptic intubation can be predicted using a newly developed formula with three patient parameters, namely, height, the NM distance, and weight. Application of this equation in the clinical setting should facilitate nasal fiberoptic intubation.





Similar content being viewed by others
Change history
30 April 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00540-022-03069-0
References
Machata AM, Gonano C, Holzer A, Andel D, Spiss CK, Zimpfer M, Illievich UM. Awake nasotracheal fiberoptic intubation: patient comfort, intubating conditions, and hemodynamic stability during conscious sedation with remifentanil. Anesth Anal. 2003;97:904–8.
Stackhouse RA. Fiberoptic airway management. Anesth Clin North Am. 2002;20:933–51.
Ovassapian A, Ovassapian A. Fiberoptic endoscopy and the difficult airway. 2nd ed. Philadelphia: Lippincott-Raven; 1996.
Tabachnick BGFL. Using multiplevariate statistics. 5th ed. Boston: Pearson; 2007.
Han DW, Shim YH, Shin CS, Lee YW, Lee JS, Ahn SW. Estimation of the length of the nares-vocal cord. Anesth Anal. 2005;100:1533–5.
Stoneham MD. The nasopharyngeal airway. Assessment of position by fibreoptic laryngoscopy. Anaesthesia. 1993;48:575–80.
Kim SH, Kim DH, Kang H, Park JJ, Seong SH, Suk EH, Hwang JH. Estimation of the nares-to-epiglottis distance and the nares-to-vocal cords distance in young children. Br J Anaesth. 2012;109:816–20.
Mohammadzadeh A, Haghighi M, Naderi B, Chaudhry A, Khan ZH, Rasouli MR, Saadat S. Comparison of two different methods of fiber-optic nasal intubation: conventional method versus facilitated method (NASAL-18). Ups J Med Sci. 2011;116:138–41.
Durga VK, Millns JP, Smith JE. Manoeuvres used to clear the airway during fibreoptic intubation. Br J Anaesth. 2001;87:207–11.
Stacey MR, Rassam S, Sivasankar R, Hall JE, Latto IP. A comparison of direct laryngoscopy and jaw thrust to aid fibreoptic intubation. Anaesthesia. 2005;60:445–8.
Albrecht E, Schoettker P. Images in clinical medicine. The jaw-thrust maneuver. N Engl J Med. 2010;363:e32.
Aoyama K, Takenaka I, Nagaoka E, Kadoya T. Jaw thrust maneuver for endotracheal intubation using a fiberoptic stylet. Anesth Analg. 2000;90:1457–8.
Reber A, Paganoni R, Frei FJ. Effect of common airway manoeuvres on upper airway dimensions and clinical signs in anaesthetized, spontaneously breathing children. Br J Anaesth. 2001;86:217–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jiwon Lee has no conflict of interest. Jung-Man Lee has no conflict of interest. Jeong Jin Min has no conflict of interest. Chang-Hoon Koo has no conflict of interest. Hyun Jeong Kim has no conflict of interest.
About this article
Cite this article
Lee, J., Lee, JM., Min, J.J. et al. Optimal length of the pre-inserted tracheal tube for excellent view in nasal fiberoptic intubation. J Anesth 30, 187–192 (2016). https://doi.org/10.1007/s00540-015-2088-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-015-2088-7