Abstract
Purpose
Recent studies have shown that pain sensitivity has a significant relationship with clinical pain and may also predict the intensity of pain and analgesic consumption after surgery. However, the correlation between pre-operative pain sensitivity and stress response during anesthesia has not been investigated. Therefore, we aimed to explore the relationship between pre-operative pain sensitivity and stress responses during intubation and skin incision in this study.
Methods
Fifty women (ASA I–II) aged 20–55 years, undergoing elective abdominal surgery requiring at least a 10-cm-long skin incision were studied. Pain sensitivity, including pain threshold and pain tolerance was measured before surgery. In this study, experimental pain was induced by potassium ion conducted via continuous current. When patients reported feeling pain or acted to stop pain, the intensity of the current was recorded to register pain threshold and pain tolerance. The State-Trait Anxiety Inventory (STAI) was used to examine the pre-operative mental status. General anesthesia was induced with intravenous fentanyl and a target-controlled infusion of propofol. Blood samples for norepinephrine (NE) detection were collected at 10 min after entering the operating theater, immediately before intubation, 2 min after intubation, immediately before skin incision and 2 min after incision. Mean arterial blood pressure (MAP) and heart rate (HR) were recorded at the same time. Pearson’s correlation test (SPSS 13.0) was then used to analyze the relationship between pain sensitivity and the changes in MAP, HR and NE level.
Results
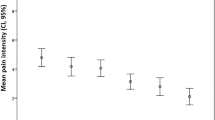
A total of fifty women were enrolled in the study. Their pre-operative pain threshold and pain tolerance were 0.90 ± 0.40 mA and 2.53 ± 0.77 mA,respectively. Changes in MAP, HR and NE before and after intubation or skin incision were significantly related with pre-operative pain tolerance (P < 0.05); however, pain threshold was not correlated with changes in MAP, HR and NE (P > 0.05). The STAI score did not correlate with the stress response either (P > 0.05).
Conclusions
Pain tolerance had a significant relationship with stress response during intubation and skin incision. We may initially use pain tolerance to direct opioid usage in the future.


Similar content being viewed by others
References
Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85(1):109–17.
Philbin DM, Rosow CE, Schneider RC, Koski G, D’Ambra MN. Fentanyl and sufentanil anesthesia revisited: how much is enough? Anesthesiology. 1990;73(1):5–11.
Guignard B, Bossard AE, Coste C, Sessler DI, Lebrault C, Alfonsi P, Fletcher D, Chauvin M. Acute opioid tolerance: intraoperative remifentanil increases postoperative pain and morphine requirement. Anesthesiology. 2000;93(2):409–17.
Salinas AS, Lorenzo-Romero J, Segura M, Calero MR, Hernandez-Millan I, Martinez-Martin M, Virseda JA. Factors determining analgesic and sedative drug requirements during extracorporeal shock wave lithotripsy. Urol Int. 1999;63(2):92–101.
de Jong RH. Body mass index: risk predictor for cosmetic day surgery. Plastic Reconstr Surg. 2001;108(2):556–61 discussion 562–553.
Edwards RR, Doleys DM, Fillingim RB, Lowery D. Ethnic differences in pain tolerance: clinical implications in a chronic pain population. Psychosom Med. 2001;63(2):316–23.
Edwards RR, Haythornthwaite JA, Tella P, Max MB, Raja S. Basal heat pain thresholds predict opioid analgesia in patients with postherpetic neuralgia. Anesthesiology. 2006;104(6):1243–8.
Granot M, Lowenstein L, Yarnitsky D, Tamir A, Zimmer EZ. Postcesarean section pain prediction by preoperative experimental pain assessment. Anesthesiology. 2003;98(6):1422–6.
Jones A, Zachariae R. Gender, anxiety, and experimental pain sensitivity: an overview. J Am Med Womens Assoc. 2002;57(2):91–4.
De Cosmo G, Congedo E, Lai C, Primieri P, Dottarelli A, Aceto P. Preoperative psychologic and demographic predictors of pain perception and tramadol consumption using intravenous patient-controlled analgesia. Clin J Pain. 2008;24(5):399–405.
Munafo MR, Stevenson J. Anxiety and surgical recovery. Reinterpreting the literature. J Psychosom Res. 2001;51(4):589–96.
Zheng Z, Wang LW, Zuo CT, Guan YH, Tao MY, Shi SX. A self comparison of the pain threshold of healthy people in the alert state and hypnotic state. Shanghai Arch Psychiatry. 2005;17(6):331–3.
Lund I, Lundeberg T, Kowalski J, Sandberg L, Budh CN, Svensson E. Evaluation of variations in sensory and pain threshold assessments by electrocutaneous stimulation. Physiotherapy Theory Pract. 2005;21(2):81–92.
Mitchell S, Reading I, Walker-Bone K, Palmer K, Cooper C, Coggon D. Pain tolerance in upper limb disorders: findings from a community survey. Occup Environ Med. 2003;60(3):217–21.
Nie Y, Liu Y, Luo Q, Huang S. Effect of dexmedetomidine combined with sufentanil for post-caesarean section intravenous analgesia: a randomised, placebo-controlled study. Eur J Anaesthesiol. 2014;31(4):197–203.
Tao KM, Tao Y, Chen CY, Yang LQ, Lu ZJ, Sun YM, Huang SD, Yu WF. Proteinase-activated receptor 1 contributed to up-regulation of enkephalin in keratinocytes of patients with obstructive jaundice. Anesthesiology. 2014;121(1):127–39.
Kanto J, Scheinin M. Biochemical assessment of preoperative stress: a study with diazepam and measurement of monoamine metabolites and catecholamines in cerebrospinal fluid and plasma. Br J Anaesth. 1991;66(5):587–90.
Parker SD, Breslow MJ, Frank SM, Rosenfeld BA, Norris EJ, Christopherson R, Rock P, Gottlieb SO, Raff H, Perler BA. Catecholamine and cortisol responses to lower extremity revascularization: correlation with outcome variables. Perioperative Ischemia Randomized Anesthesia Trial Study Group. Crit Care Med. 1995;23(12):1954–61.
Hamberger B, Jarnberg PO. Plasma catecholamines during surgical stress: differences between neurolept and enflurane anaesthesia. Acta Anaesthesiol Scand. 1983;27(4):307–10.
Oehmke MJ, Podranski T, Mann M, Frickey N, Kuhn DF, Hempelmann G. Perioperative concentrations of catecholamines in the cerebrospinal fluid and plasma during spinal anesthesia. Acta Anaesthesiol Scand. 2008;52(4):487–92.
Kono K, Philbin DM, Coggins CH, Moss J, Rosow CE, Schneider RC, Slater EE. Renal function and stress response during halothane or fentanyl anesthesia. Anesth Analg. 1981;60(8):552–6.
Rosa C, Ghione S, Mezzasalma L, Pellegrini M, Fasolo CB, Giaconi S, Gazzetti P, Ferdeghini M. Relationship between pain sensitivity, cardiovascular reactivity to cold pressor test and indexes of activity of the adrenergic and opioid system. Clin Exp Hypertens A. 1988;10:383–90.
Duschek S, Schwarzkopf W, Schandry R. Increased pain sensitivity in low blood pressure. J Psychophysiol. 2008;22(1):20–7.
Coghill R, McHaffie J, Yen YF. Supraspinal correlates of inter-individual differences in pain sensitivity. Neuroimage. 2001;13(6):S873.
Ozalp G, Sarioglu R, Tuncel G, Aslan K, Kadiogullari N. Preoperative emotional states in patients with breast cancer and postoperative pain. Acta Anaesthesiol Scand. 2003;47(1):26–9.
Thompson T, Keogh E, French CC, Davis R. Anxiety sensitivity and pain: generalisability across noxious stimuli. Pain. 2008;134(1–2):187–96.
Arntz A, Dreessen L, Merckelbach H. Attention, not anxiety, influences pain. Behav Res Ther. 1991;29(1):41–50.
James JE, Hardardottir D. Influence of attention focus and trait anxiety on tolerance of acute pain. Br J Health Psychol. 2002;7(Pt 2):149–62.
Ledowski T, Pascoe E, Ang B, Schmarbeck T, Clarke MW, Fuller C, Kapoor V. Monitoring of intra-operative nociception: skin conductance and surgical stress index versus stress hormone plasma levels. Anaesthesia. 2010;65(10):1001–6.
Acknowledgments
Dr. Haitang Wang and Dr. Yehua Cai are the co-first authors.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Wang, H., Cai, Y., Liu, J. et al. Pain sensitivity: a feasible way to predict the intensity of stress reaction caused by endotracheal intubation and skin incision?. J Anesth 29, 904–911 (2015). https://doi.org/10.1007/s00540-015-2040-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-015-2040-x