Abstract
Background
Ampullary early stage cancer (early CA) potentially harbors lymphovascular invasion; there are few data on markers that could differentiate adenoma and early CA.
Aim
To investigate those markers, we compared the tumor diameter and Ki-67 expression in endoscopy biopsy specimens of adenoma with those of early CA.
Methods
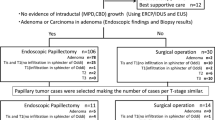
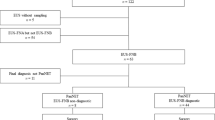
Patients on whom endoscopic papillectomy (EP) was performed (n = 35) with histopathologically proven adenomas and with low/high grade dysplasia and early CA were studied. We made pre-procedure evaluations of ampullary tumors by using endoscopic ultrasonography (EUS) and transpapillary intraductal ultrasonography. Tumor diameter was measured by EUS. Endoscopic biopsy using immunostaining of Ki-67 labeling index (LI) prior to EP were evaluated.
Results
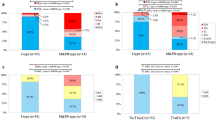
The areas under the receiver-operating characteristic (AUROC) curves for tumor diameter and Ki-67 expression were 0.824 and 0.873, respectively. Cut-off values calculated based on AUROC data were 15 mm in tumor diameter and 32 cells/high-power field (HPF) in Ki-67. Early CA (n = 11) was diagnosed by using a cut-off value for tumor diameter in 8 out of 11 patients (sensitivity 72.7 %, specificity 66.7 %, accuracy 68.6 %). Significant infiltration of the major duodenal papilla by Ki-67 positive tumor cells (>31/HPF) was recognized in 8 of the 11 patients with early CA (sensitivity 100 %, specificity 54.2 %, accuracy 62.9 %).
Conclusions
Observation of tumor diameter and Ki-67 LI would be helpful for safety EP. EP should not be indicated for ampullary tumors more than 15 mm in diameter and/or Ki-67 LI 31/HPF.






Similar content being viewed by others
References
Yoon SM, Kim MH, Kim MJ, Jang SJ, Lee TY, Kwon S, et al. Focal early stage cancer in ampullary adenoma: surgery or endoscopic papillectomy? GIE. 2007;66:701–7.
Salmi S, Ezzedine S, Vitton V, Menard C, Gonzales JM, Desjeux A, et al. Can papillary carcinomas be treated by endoscopic ampullectomy? Surg Endosc. 2012;26:920–5.
Winter JM, Cameron JL, Olono K, Herman JM, de Jong MC, Hruban RH, et al. Clinicopathologic analysis of ampullary neoplasms in 450 patients: implication for surgical strategy and long-term prognosis. J Gastrointest Surg. 2010;14:379–87.
Irani S, Arai A, Ayub K, Biehl T, Brandabur JJ, Dorerr, R et al. Papillectomy for ampullary neoplasm: results of a single referral center over a 10-year period. GIE. 2009;70:923–32.
Ito K, Fujita N, Noda N, Kobayashi G, Horaguchi J, Takazawa O, et al. Preoperative evaluation of ampullary neoplasm with endoscopic ultrasonography (EUS) and transpapillary intraductal ultrasonography (IDUS)—a prospective and histopathologically controlled study. GIE. 2007;60:740–47.
Yamaguchi K, Enjoji M, Kitamura K. Endoscopic biopsy has limited accuracy in diagnosis of ampullary tumors. GIE. 1990;36:588–92.
Kubota K, Kakuta Y, Kawamura S, Saito S, Seki H, et al. Usefulness of endoscopic biopsy using immunostaining of p53 and Ki-67 in tumor of the ampulla of Vater. Pathol Int. 2003;53:361–70.
Patel R, Varadarajulu S, Wilcox CM. Endoscopic ampullectomy techniques and outcomes. J Clin Gastoenterol. 2012;46:8–15.
Woo SM, Ryu JK, Lee SH, Lee WJ, Hwang JH, Yoo JW, et al. Feasibility of endoscopic papillectomy in early stage ampulla of Vater cancer. GIE. 2008;24:120–4.
Itoh A, Tsukamoto Y, Naitoh Y, Gotoh H, et al. Intraductal ultrasonography in diagnosing tumor extension of cancer the papilla of Vater. GIE. 1997;45:251–60.
Schlemper AD, Riddle RH, Kato Y, Borchard F, Cooper HS, Dawsey SM, et al. The Vienna classification of the gastrointestinal epithelial neoplasia. GUT. 2000;47:251–5.
Igarashi Y, Okano N, Ito K, Miura T, Nakano S. Endoscopic snare excision of a major duodenal papillary tumor. Dig Surg. 2010;27:119–22.
Kim JH, Kim JH, Han JH, Yoo BM, Kim MW, Kim WH. Is endoscopic papillectomy safe for ampullary adenomas with high-grade dysplasia? Ann Surg Oncol. 2009;16:2547–54.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kubota, K., Fujita, Y., Sato, T. et al. Tumor diameter and Ki-67 expression in biopsy could be diagnostic markers discriminating from adenoma and early stage cancer in patients with ampullary tumors. J Hepatobiliary Pancreat Sci 20, 531–537 (2013). https://doi.org/10.1007/s00534-013-0594-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-013-0594-2