Abstract
Purpose
Women treated for cervical cancer with radiotherapy and chemotherapy have reported serious bowel, vaginal, and sexual late effects. The purpose of this study was to describe late adverse effects, health-related quality of life, and self-efficacy in a representative Danish cervical cancer population in order to describe rehabilitation needs.
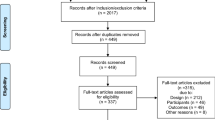
Methods
Women, mean age 55 years, treated for cervical cancer from January 2010 to July 2013, who were alive and without known relapse/metastases were included in this cross-sectional study. EORTC QLQ C30 and CX24 and self-efficacy questionnaires were sent to all participants.
Results
The participation rate was 85/107 (79%). Participants below 45 years had significantly more menopausal symptoms and lower body image scores compared to elderly women. The frequency of participants with menopausal symptoms decreased with time since diagnosis. Symptom experience was significantly higher in participants with locally advanced disease than in those with local disease. Self-efficacy was significantly lower in participants with locally advanced disease. The incidence of lymphedema was significantly higher among participants who were obese. Multiple analyses showed impaired quality of life, e.g., a lower body image and self-efficacy score, correlated with increasing BMI. Women who had surgery had greater risk of lymphedema, and women who received chemotherapy during treatment had a lower quality of life. All but one received radiotherapy.
Conclusion
This study found that young, obese survivors with locally advanced cervical cancer and survivors who received chemotherapy may have a serious risk of developing late adverse effects; thus, rehabilitation should target these needs.


Similar content being viewed by others
References
Lynge E, Rygaard C, Baillet MV, Dugue PA, Sander BB, Bonde J, Rebolj M (2014) Cervical cancer screening at crossroads. APMIS: Acta Pathol, Microbiol, et Immunologica Scandinavica 122(8):667–673. doi:10.1111/apm.12279
Statens Serum Institut (2013) Cancerregisteret. Tal og analyse
NORDCAN (2016) Cancer incidence, mortality, prevalence and survival in the Nordic countries, Version 7.2 (16.12.2015). Association of the Nordic Cancer Registries. Danish Cancer Society. Accessed 18. Jan 2016
Park SY, Bae DS, Nam JH, Park CT, Cho CH, Lee JM, Lee MK, Kim SH, Park SM, Yun YH (2007) Quality of life and sexual problems in disease-free survivors of cervical cancer compared with the general population. Cancer 110(12):2716–2725. doi:10.1002/cncr.23094
Bifulco G, De Rosa N, Tornesello ML, Piccoli R, Bertrando A, Lavitola G, Morra I, Di Spiezio SA, Buonaguro FM, Nappi C (2012) Quality of life, lifestyle behavior and employment experience: a comparison between young and midlife survivors of gynecology early stage cancers. Gynecol Oncol 124(3):444–451. doi:10.1016/j.ygyno.2011.11.033
Froeding LP, Ottosen C, Rung-Hansen H, Svane D, Mosgaard BJ, Jensen PT (2014) Sexual functioning and vaginal changes after radical vaginal trachelectomy in early stage cervical cancer patients: a longitudinal study. J Sex Med 11(2):595–604. doi:10.1111/jsm.12399
Pieterse QD, Kenter GG, Maas CP, de Kroon CD, Creutzberg CL, Trimbos JB, Ter Kuile MM (2013) Self-reported sexual, bowel and bladder function in cervical cancer patients following different treatment modalities: longitudinal prospective cohort study. Int J Gynecol Cancer: Off J Int Gynecol Cancer Soc 23(9):1717–1725. doi:10.1097/IGC.0b013e3182a80a65
Barker CL, Routledge JA, Farnell DJ, Swindell R, Davidson SE (2009) The impact of radiotherapy late effects on quality of life in gynaecological cancer patients. Br J Cancer 100(10):1558–1565. doi:10.1038/sj.bjc.6605050
Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D (2003) Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. Int J Radiat Oncology*Biology*Physics 56(4):937–949. doi:10.1016/s0360-3016(03)00362-6
Froding LP, Ottosen C, Mosgaard BJ, Jensen PT (2015) Quality of life, urogynecological morbidity, and lymphedema after radical vaginal trachelectomy for early-stage cervical cancer. Int J Gynecol Cancer: Off J Int Gynecol Cancer Soc 25(4):699–706. doi:10.1097/IGC.0000000000000395
Mantegna G, Petrillo M, Fuoco G, Venditti L, Terzano S, Anchora LP, Scambia G, Ferrandina G (2013) Long-term prospective longitudinal evaluation of emotional distress and quality of life in cervical cancer patients who remained disease-free 2-years from diagnosis. BMC cancer 13(127) doi:10.1186/1471-2407-13-127
Kirchheiner K, Nout R, Lindegaard J, Petric P, Limbergen EV, Jurgenliemk-Schulz IM, Haie-Meder C, Pötter R, Dorr W (2012) Do clinicians and patients agree regarding symptoms? A comparison after definitive radiochemotherapy in 223 uterine cervical cancer patients. Strahlentherapie und Onkologie: Organ der Deutschen Rontgengesellschaft 188(10):933–939. doi:10.1007/s00066-012-0156-6
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Greimel ER, Kuljanic Vlasic K, Waldenstrom AC, Duric VM, Jensen PT, Singer S, Chie W, Nordin A, Bjelic Radisic V, Wydra D, European Organization for R, Treatment of Cancer Quality-of-Life G (2006) The European Organization for Research and Treatment of Cancer (EORTC) quality-of-life questionnaire cervical cancer module: EORTC QLQ-CX24. Cancer 107(8):1812–1822. doi:10.1002/cncr.22217
Kjaer TK, Johansen C, Ibfelt E, Christensen J, Rottmann N, Hoybye MT, Ross L, Svendsen M, Dalton SO (2011) Impact of symptom burden on health related quality of life of cancer survivors in a Danish cancer rehabilitation program: a longitudinal study. Acta Oncol 50(2):223–232. doi:10.3109/0284186X.2010.530689
DGCG (2011) Retningslinier for visitation, diagnostik, behandling og kontrol af cervixcancer. DGCG
Schwarzer R, Jerusalem M (1995) Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M (eds) Measures in health psychology: a user’s portfolio. Causal and control beliefs. NFER-NELSON, Windsor, pp. 35–37
Fayers PM, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A, Group obotEQoL (2001) The EORTC QLQ-C30 scoring manual, 3rd edn. European Organisation for Research and Treatment of Cancer, Brussels
Sundhedsstyrelsen (2010) Den nationale sundhedsprofil 2010—Hvordan har du det? Sundhedsstyrelsen
Juul T, Petersen MA, Holzner B, Laurberg S, Christensen P, Gronvold M (2014) Danish population-based reference data for the EORTC QLQ-C30: associations with gender, age and morbidity. Qual Life Res: Int J Quality Life Aspects Treat, Care Rehabil 23(8):2183–2193. doi:10.1007/s11136-014-0675-y
Hinz A, Singer S, Brahler E (2014) European reference values for the quality of life questionnaire EORTC QLQ-C30: results of a German investigation and a summarizing analysis of six European general population normative studies. Acta Oncol 53(7):958–965. doi:10.3109/0284186X.2013.879998
Schmitz KH, Neuhouser ML, Agurs-Collins T, Zanetti KA, Cadmus-Bertram L, Dean LT, Drake BF (2013) Impact of obesity on cancer survivorship and the potential relevance of race and ethnicity. J Natl Cancer Inst 105(18):1344–1354. doi:10.1093/jnci/djt223
Beesley V, Janda M, Eakin E, Obermair A, Battistutta D (2007) Lymphedema after gynecological cancer treatment: prevalence, correlates, and supportive care needs. Cancer 109(12):2607–2614. doi:10.1002/cncr.22684
Kizer NT, Thaker PH, Gao F, Zighelboim I, Powell MA, Rader JS, Mutch DG, Grigsby PW (2011) The effects of body mass index on complications and survival outcomes in patients with cervical carcinoma undergoing curative chemoradiation therapy. Cancer 117(5):948–956. doi:10.1002/cncr.25544
Schlumbrecht MP, Sun CC, Huang MS, Zandstra F, Bodurka DC (2014) Lifestyle modification in cervical cancer survivors: an ongoing need. Int J Gynecol Cancer: Off J Int Gynecol Cancer Soc 24(3):570–575. doi:10.1097/IGC.0000000000000081
Acknowledgements
We especially wish to thank the women who participated in the study for their valuable contributions and Lærke Kjær Tolstrup for linguistic corrections. On behalf of the Danish Knowledge Centre for Rehabilitation and Palliative Care (REHPA) www.rehpa.dk and the Academy of Geriatric Cancer Research (AgeCare) www.agecare.org.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics and data protection
In Denmark, this kind of research does not require approval from an ethics committee; however, the study was approved by the Danish National Data Protection Agency (File number 2008-58-0035, journal number 14/4754).
Conflict of interest
The authors declare that they have no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Rights and permissions
About this article
Cite this article
Mikkelsen, T.B., Sørensen, B. & Dieperink, K.B. Prediction of rehabilitation needs after treatment of cervical cancer: what do late adverse effects tell us?. Support Care Cancer 25, 823–831 (2017). https://doi.org/10.1007/s00520-016-3466-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3466-x