Abstract
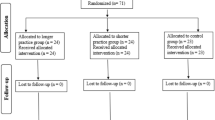
Health-related quality of life (HRQoL) is often substantially reduced among individuals who have undergone hematopoietic stem cell transplantation (HSCT), and incidences of depression, fatigue, and anxiety are elevated. We examined effects of a mindfulness-based intervention (MBI) compared to psycho-oncological telephone consultation upon HRQoL, depression, anxiety, and fatigue among HSCT survivors. Sixty-two medically stable patients participated in the study; they had completed HSCT ≥6 months previously. Thirty-two were randomly assigned to intervention arms, and 30 were offered their treatment preference. MBI consisted of a structured 8-week program of mindfulness training. Assessments were made at baseline, post-intervention and 3 months follow-up. Primary outcome was HRQoL. Depression, fatigue, anxiety, and personal goal attainment were secondary measures. Non-completion of interventions was low in both groups (9 %, MBI; 7 % control). Employing intention-to-treat analysis, MBI, compared with comparison procedure, improved HRQoL and reduced depression and anxiety at post-intervention (p’s < 0.05); Cohen’s d effect sizes, 0.6–0.7; 3-month follow-up benefits were modest. These findings demonstrate broad feasibility and acceptance of, as well as satisfaction and adherence with, a program of mindfulness training for HSCT survivors; findings also suggest improved HRQoL and well-being as a consequence of MBI. Nevertheless, this is a preliminary study; a larger trial with more prolonged intervention phase is warranted.

Similar content being viewed by others
References
Carlson LE, Doll R, Stephen J, Faris P, Tamagawa R, Drysdale E et al (2013) Randomized controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer. J Clin Oncol 31(25):3119–3126
Hoffman CJ, Ersser SJ, Hopkinson JB, Nicholls PG, Harrington JE, Thomas PW (2012) Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: a randomized, controlled trial. J Clin Oncol 30(12):1335–1342
Wurtzen H, Dalton SO, Elsass P, Sumbundu AD, Steding-Jensen M, Karlsen RV et al (2013) Mindfulness significantly reduces self-reported levels of anxiety and depression: results of a randomised controlled trial among 336 Danish women treated for stage I-III breast cancer. Eur J Cancer 49(6):1365–1373
Carlson LE, Ursuliak Z, Goodey E, Angen M, Speca M (2001) The effects of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients: 6-month follow-up. Support Care Cancer 9(2):112–123
Speca M, Carlson LE, Goodey E, Angen M (2000) A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med 62(5):613–622
Bauer-Wu S, Sullivan AM, Rosenbaum E, Ott MJ, Powell M, McLoughlin M et al (2008) Facing the challenges of hematopoietic stem cell transplantation with mindfulness meditation: a pilot study. Integr Cancer Ther 7(2):62–69
McArdle JR (2009) Critical care outcomes in the hematologic transplant recipient. Clin Chest Med 30(1):155–167
Michlitsch JG, Walters MC (2008) Recent advances in bone marrow transplantation in hemoglobinopathies. Curr Mol Med 8(7):675–689
Porta F, Locatelli F, Burgio GR (2008) Hematopoietic stem cell transplantation: 40 years of continuous progress and evolution. Haematologica 93(11):1607–1610
Petersdorf EW, Hansen JA (2008) New advances in hematopoietic cell transplantation. Curr Opin Hematol 15(6):549–554
Ferrara JL (2008) Advances in the clinical management of GVHD. Best Pract Res Clin Haematol 21(4):677–682
Gratwohl A (2002) New developments in hematopoietic stem cell transplantation. Ther Umsch 59(11):571–6
Passweg J, Baldomero H, Chapuis B, Leibundgut K, Schanz U, Gratwohl A (2006) Haematopoietic stem cell transplantation in Switzerland. Report from the Swiss Transplant Working Group Blood and Marrow Transplantation (STABMT) Registry 1997–2003. Swiss Med Wkly 136(3–4):50–58
Carlson LE, Smith D, Russell J, Fibich C, Whittaker T (2006) Individualized exercise program for the treatment of severe fatigue in patients after allogeneic hematopoietic stem-cell transplant: a pilot study. Bone Marrow Transplant 37(10):945–954
Carr D, Goudas L, Lawrence D et al (2002) Management of cancer symptoms: pain, depression, and fatigue. Agency for Healthcare Research and Quality, Rockville, MD
Butt Z, Rosenbloom SK, Abernethy AP, Beaumont JL, Paul D, Hampton D et al (2008) Fatigue is the most important symptom for advanced cancer patients who have had chemotherapy. J Natl Compr Canc Netw 6(5):448–455
Syrjala KL, Kurland BF, Abrams JR, Sanders JE, Heiman JR (2008) Sexual function changes during the 5 years after high-dose treatment and hematopoietic cell transplantation for malignancy, with case-matched controls at 5 years. Blood 111(3):989–996
Tichelli A, Rovo A, Gratwohl A (2008) Late pulmonary, cardiovascular, and renal complications after hematopoietic stem cell transplantation and recommended screening practices. Hematol Am Soc Hematol Educ Program 2008:125–133
Rovo A, Daikeler T, Stern M, Halter J, Studt JD, Buser A et al (2008) Physical and not mental health is impaired in very long-term survivors after HSCT compared with their respective donors: a paired analysis. Blood 111(3):1740–1741
Tichelli A, Bucher C, Rovo A, Stussi G, Stern M, Paulussen M et al (2007) Premature cardiovascular disease after allogeneic hematopoietic stem-cell transplantation. Blood 110(9):3463–3471
Hjermstad MJ, Knobel H, Brinch L, Fayers PM, Loge JH, Holte H et al (2004) A prospective study of health-related quality of life, fatigue, anxiety and depression 3–5 years after stem cell transplantation. Bone Marrow Transplant 34:257–266
Stein KD, Syrjala KL, Andrykowski MA (2008) Physical and psychological long-term and late effects of cancer. Cancer 112(11 Suppl):2577–2592
Bhatia S, Robison LL, Francisco L, Carter A, Liu Y, Grant M et al (2005) Late mortality in survivors of autologous hematopoietic-cell transplantation: report from the Bone Marrow Transplant Survivor Study. Blood 105(11):4215–4222
Bhatia S, Francisco L, Carter A, Sun CL, Baker KS, Gurney JG et al (2007) Late mortality after allogeneic hematopoietic cell transplantation and functional status of long-term survivors: report from the Bone Marrow Transplant Survivor Study. Blood 110(10):3784–3792
Khera N, Storer B, Flowers ME, Carpenter PA, Inamoto Y, Sandmaier BM et al (2012) Nonmalignant late effects and compromised functional status in survivors of hematopoietic cell transplantation. J Clin Oncol 30(1):71–77
Ness KK, Bhatia S, Baker KS, Francisco L, Carter A, Forman SJ et al (2005) Performance limitations and participation restrictions among childhood cancer survivors treated with hematopoietic stem cell transplantation: the bone marrow transplant survivor study. Arch Pediatr Adolesc Med 159(8):706–713
Norkin M, Hsu JW, Wingard JR (2012) Quality of life, social challenges, and psychosocial support for long-term survivors after allogeneic hematopoietic stem-cell transplantation. Semin Hematol 49(1):104–109
Shanis D, Merideth M, Pulanic TK, Savani BN, Battiwalla M, Stratton P (2012) Female long-term survivors after allogeneic hematopoietic stem cell transplantation: evaluation and management. Semin Hematol 49(1):83–93
Sun CL, Francisco L, Baker KS, Weisdorf DJ, Forman SJ, Bhatia S (2011) Adverse psychological outcomes in long-term survivors of hematopoietic cell transplantation: a report from the Bone Marrow Transplant Survivor Study (BMTSS). Blood 118(17):4723–4731
Bevans MF, Mitchell SA, Barrett J, Bishop MR, Childs R, Fowler D et al (2013) Symptom distress predicts long-term health and well-being in allogeneic stem cell transplantation survivors. Biol Blood Marrow Transplant 20(3):387–395
Mitchell AJ, Benito-Leon J, Gonzalez JM, Rivera-Navarro J (2005) Quality of life and its assessment in multiple sclerosis: integrating physical and psychological components of wellbeing. Lancet Neurol 4(9):556–566
Mosher CE, Redd WH, Rini CM, Burkhalter JE, Duhamel KN (2008) Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psychooncology 18(2):113–127
Wiskemann J, Huber G (2008) Physical exercise as adjuvant therapy for patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant 41(4):321–329
Kim SD, Kim HS (2005) Effects of a relaxation breathing exercise on anxiety, depression, and leukocyte in hemopoietic stem cell transplantation patients. Cancer Nurs 28(1):79–83
Kim SD, Kim HS (2005) Effects of a relaxation breathing exercise on fatigue in haemopoietic stem cell transplantation patients. J Clin Nurs 14:51–55
DuHamel KN, Mosher CE, Winkel G, Labay LE, Rini C, Meschian YM et al (2010) Randomized clinical trial of telephone-administered cognitive-behavioral therapy to reduce post-traumatic stress disorder and distress symptoms after hematopoietic stem-cell transplantation. J Clin Oncol 28(23):3754–3761
Mock V (2004) Evidence-based treatment for cancer-related fatigue. J Nat Cancer Inst Monographs 32:112–118
Hoodin F, Uberti JP, Lynch TJ, Steele P, Ratanatharathorn V (2006) Do negative or positive emotions differentially impact mortality after adult stem cell transplant? Bone Marrow Transplant 38(4):255–264
Akaho R, Sasaki T, Mori S-I, Akiyama H, Yoshino M, Hagiya K et al (2003) Psychological factors and survival after bone marrow transplantation in patients with leukemia. Psychiatry Clin Neurosci 57(1):91–96
Hochhausen N, Altmaier EM, McQuellon R, Davies SM, Papadopolous E, Carter S et al (2007) Social support, optimism, and self-efficacy predict physical and emotional well-being after bone marrow transplantation. J Psychosoc Oncol 25(1):87–101
Jenks Kettmann JD, Altmaier EM (2008) Social support and depression among bone marrow transplant patients. J Health Psychol 13(1):39–46
Grossman P, Niemann L, Schmidt S, Walach H (2004) Mindfulness-based stress reduction and health benefits: a meta-analysis. J Psychosom Res 57(1):35–43
Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain and Illness. Revised Edition New York: Delacorte; 2013.
Grossman P, Kappos L, Gensicke H, D’Souza M, Mohr DC, Penner IK et al (2010) MS quality of life, depression, and fatigue improve after mindfulness training: a randomized trial. Neurology 75(13):1141–1149
Beaver K, Tysver-Robinson D, Campbell M, Twomey M, Williamson S, Hindley A et al (2009) Comparing hospital and telephone follow-up after treatment for breast cancer: randomised equivalence trial. BMJ 338:a3147
Chamberlain Wilmoth M, Tulman L, Coleman EA, Stewart CB, Samarel N (2006) Women’s perceptions of the effectiveness of telephone support and education on their adjustment to breast cancer. Oncol Nurs Forum 33(1):138–144
Chumbler NR, Mkanta WN, Richardson LC, Harris L, Darkins A, Kobb R et al (2007) Remote patient-provider communication and quality of life: empirical test of a dialogic model of cancer care. J Telemed Telecare 13(1):20–25
Coleman EA, Tulman L, Samarel N, Wilmoth MC, Rickel L, Rickel M et al (2005) The effect of telephone social support and education on adaptation to breast cancer during the year following diagnosis. Oncol Nurs Forum 32(4):822–829
Siegrist J, Broer M, Junge A (1996) Profil der Lebensqualität chronisch Kranker. Manual. [Profile of Quality of Life for the Chronically Ill]. Beltz Test, Göttingen
Hart S, Fonareva I, Merluzzi N, Mohr DC (2005) Treatment for depression and its relationship to improvement in quality of life and psychological well-being in multiple sclerosis patients. Qual Life Res 14(3):695–703
Grossman P, Tiefenthaler U, Raysz A, Kesper U (2007) Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychother Psychosom 76(4):226–233
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A et al (1993) The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 11(3):570–579
Victorson D, Barocas J, Song J, Cella D (2008) Reliability across studies from the functional assessment of cancer therapy-general (FACT-G) and its subscales: a reliability generalization. Qual Life Res 17(9):1137–1146
Hautzinger M, Bailer M (1991) Allgemeine Depressionsskala (ADS). Die deutsche Version des CES-D. Weinheim, Beltz
Radloff LS (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D et al (1993) Development of a fatigue scale. J Psychosom Res 37(2):147–153
Cohen J (1988) Statistical power analysis for the behavioral sciences. Academic, New York
Schmoor C, Olschewski M, Schumacher M (1996) Randomized and non-randomized patients in clinical trials: experiences with comprehensive cohort studies. Stat Med 15:263–271
Lin P, Campbell DG, Chaney EF, Liu CF, Heagerty P, Felker BL et al (2005) The influence of patient preference on depression treatment in primary care. Ann Behav Med 30:164–173
Preference-Collaborative-Review-Group. Patients’ preferences within randomised trials: systematic review and patient level meta-analysis. BMJ 2008;337:a1864
Howard L, Thornicroft G (2006) Patient preference randomised controlled trials in mental health research. Br J Psychiatry 188:303–304
Torgerson DJ, Sibbald B (1998) Understanding controlled trials. What is a patient preference trial? BMJ 316:360
Acknowledgments
We express deepest gratitude to all the patients who participated in this study, the mindfulness teachers Barbara Dietz-Waschkowski and Silvia Wiesmann as well to Silke Purschke and Susanne Müller, study nurses from the Clinical Trial Unit of our institution, who tirelessly recruited our participants. This study is dedicated to the memory of the investigation’s lead MBI teacher Ulrike Kesper-Grossman (1953-2012).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grossman, P., Zwahlen, D., Halter, J.P. et al. A mindfulness-based program for improving quality of life among hematopoietic stem cell transplantation survivors: feasibility and preliminary findings. Support Care Cancer 23, 1105–1112 (2015). https://doi.org/10.1007/s00520-014-2452-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2452-4