Abstract
Purpose
Because as many as 30 % of cancer patients who receive chemotherapy of moderate or high emetogenic potential suffer from chemotherapy-induced nausea and vomiting (CINV), we undertook a multinational survey to identify health care providers’ perceived knowledge gaps, barriers, and educational interests relevant to CINV.
Methods
An Internet-based survey was developed and was electronically disseminated to members of Medscape, an international Internet-based continuing medical education provider.
Results
A total of 2,388 health care providers responded to the survey. Although breakthrough nausea and vomiting was the most common CINV-related issue they managed in the preceding year, managing delayed nausea was the most problematic in that time period. Thirty-two percent of health care providers delayed or discontinued a patient’s chemotherapy because of CINV. Cost of antiemetics, patients’ poor adherence to antiemetic regimens, and health care providers’ underestimation of risk for CINV were all barriers to effective management. Health care providers expressed a wide range of educational interests, including managing breakthrough CINV, keeping up with novel antiemetic agents, and learning about emerging approaches for CINV prevention/management.
Conclusions
This survey of health care providers uncovered key barriers and educational needs relevant to the management of CINV. The findings from this survey can be used to develop educational initiatives focused on improving the care of cancer patients at risk for or suffering from CINV.
Similar content being viewed by others
Introduction
Nitrogen mustard (HN-2) is approaching its 65th anniversary as the first cancer chemotherapy drug to gain approval by the US Food and Drug Administration (FDA). Apropos, an early clinical report about this agent serves to highlight many decades’ worth of subsequent progress in cancer care [1]:
The most important toxic effect of HN2 is the gastrointestinal disturbance that occurs in almost all patients. Nausea, usually with vomiting, begins one to three hours after injection and lasts for two to three hours, occasionally until the next day…. In our hands rather heavy sedation has been the most effective means of controlling the nausea and vomiting. Ordinarily we have used 0.2 gm of sodium amytal…. Sleep may be interrupted by nausea and even vomiting but some rest is obtained….
When this report was first published, patients were hospitalized and sedated to control chemotherapy-induced nausea and vomiting (CINV). Today, however, this approach is rarely necessary. Contemporary drugs—which include selective serotonin 5-HT3 receptor antagonists and neurokinin-1 receptor antagonists—have replaced amytal sodium as the preferred therapy for CINV [2, 3]. These newer drugs are mechanism-based, well tolerated, and far more effective than older treatment modalities. Moreover, such improvements as the use of combination antiemetic regimens, health care providers’ increasing awareness of anticipatory and delayed nausea and vomiting, ranking all chemotherapy regimens by their emetogenic potential, premedicating patients with the most appropriate antiemetics based on emetogenic risk, and the development, implementation, and dissemination of practice guidelines for preventing and controlling CINV illustrate more than 65 years’ worth of progress in cancer care [2, 3]. The foregoing advances represent major strides in the management of CINV.
Despite such improvements, a notable percentage of patients continue to experience CINV. Although patients participating in CINV clinical trials can manifest better outcomes, as has been observed in other clinical trial settings, even in this setting, approximately 10 to 30 % of cancer patients treated with chemotherapy of moderate to high emetogenic potential develop CINV [4, 5]. Thus, patients are still contending with these chemotherapy-related adverse effects and in general clinical practice, the proportion of patients affected is likely higher than reported. The unmet goal is to reduce the percentage of cancer patients experiencing CINV to zero. However, questions arise when working to achieve this goal and need to be addressed: Do all health care providers feel prepared to manage nausea and vomiting effectively in cancer patients receiving chemotherapy? What do health care providers identify as educational gaps that can be addressed and thereby lead to improvements in CINV management?
To answer these questions, a survey-based project was undertaken to query health care providers to learn of their educational needs and interests relevant to CINV. The premise of the project was that if lack of knowledge precludes the implementation of the advanced anti-CINV therapies described above, then educational efforts are of paramount importance for improvement in patient care. Hence, the goal of this survey was to gain a broad international perspective to enable educators to home in on areas of need. Such survey findings would allow the development of educational programs that address these needs and ultimately improve the care of cancer patients at risk for or actively experiencing CINV.
Methods
Overview
The current report describes an online, Medscape-sponsored, and conducted survey that garnered health care providers’ self-reported demographic information, perceived gaps in knowledge in the management of CINV, and preferences with respect to specific educational topics on CINV.
Survey development
A 16-question survey was developed and subsequently formatted using commercially available survey software (www.surveymonkey.com). This survey included four questions about health care providers’ demographic information, nine questions about health care providers’ clinical experiences and institutional practice patterns related to controlling or failing to control CINV, and three questions about the educational resources that health care providers believe would help them better prevent or manage CINV. Survey questions were drafted, shared with other educators and CINV specialists, and then revised for clarity.
Health care provider recruitment
Using Medscape membership e-mail distribution lists, Medscape staff included a link to the survey in the organization’s weekly eNewsletter and also posted a link to the survey on its website. This survey was posted on May 20, 2013, and advertised via the weekly eNewsletter for 12 weeks, with a final closing of the survey on August 9, 2013. Health care providers were able to complete the survey only once. Survey answers were confidential and individual respondents were not identifiable. No compensation was provided for survey completion.
Analyses of results
Data are presented descriptively with numbers, percentages, and frequencies. Data were organized and put in tabular format with the software available on www.surveymonkey.com. Data specific to hematology/oncology specialists and nurses were analyzed, compared, and presented separately, as this specialty represents the largest group of respondents and the subset most likely to maintain a steadfast interest in this topic. Descriptive and nonparametric statistics were used for the analysis and conducted with IBM SPSS Statistics Version 22 (Armonk, New York, USA). A P value of < .05 is considered statistically significant.
Results
Demographics
A total of 2,388 health care providers completed the survey (Table 1). The largest proportion of respondents consisted of nurses or advanced practice nurses and comprised 1,651 respondents (69 %). Four hundred forty-one respondents (19 %) described their area of interest as hematology/oncology from among 71 categories of disciplines provided. However, a spectrum of other specialties was represented, including critical/intensive care (118 [5 %]), emergency medicine (115 [5 %]), geriatrics (114 ([5 %]), and family medicine (99 [4 %]) as well as others (Table 1). Twenty-one percent of respondents identified their practice as within an academic setting, whereas 51 % indicated it was within a community setting. The majority of respondents identified the USA as their primary practice location (70 %) from a list of 248 countries.
Clinical gaps in CINV management
Among all the health care providers, 903 (50 %) reported that breakthrough nausea and vomiting was the most commonly encountered type of CINV, and 483 (33 %) reported that delayed nausea was the most problematic to manage (Table 2). A notable percentage of hematology/oncology physicians and hematology/oncology nurses also reported that delayed nausea was problematic (61 and 50 %, respectively). Interestingly, a higher proportion of hematology/oncology nurses indicated that acute nausea was the most problematic to manage compared with hematology/oncology physicians (20 vs 9 %, respectively, P < .0001). The percentage of hematology/oncology physicians and hematology/oncology nurses who strongly agreed/agreed that CINV is well controlled in their patients was 95 and 88 %, respectively (P = .01). As many as 32 % of the hematology/oncology respondents reported that they delayed or discontinued chemotherapy in their patients during the past year because of nausea or vomiting.
Reported barriers to effective management of CINV included the following: cost of antiemetics, poor patient adherence to antiemetic regimens, limited formulary antiemetic options, and health care providers’ poor adherence to guidelines. In addition, respondents selected intravenous (IV) as the preferred route of administration of antiemetics primarily because of “convenience for the patient” (Table 2). A greater percentage of hematology/oncology nurses preferred IV antiemetics compared with hematology/oncology physicians (60 vs 42 %; P = .002).
Educational topics of interest and importance
Most respondents expressed a strong interest in learning more about all of the 24 CINV-related educational topics listed as choices (Table 3). The topics that garnered the strongest interest (“strongly agree”) were the prevention/management of breakthrough nausea and vomiting, keeping abreast of emerging clinical data on CINV, and preventive strategies. Among hematology/oncology physicians, the topics of strongest interest (strongly agree) were integrating novel therapies for the prevention and treatment of CINV, keeping up to date on new clinical data on the topic, preventing/managing CINV with multiagent chemotherapy, breakthrough nausea and vomiting, and the treatment of refractory CINV (Table 4).
Among the ten emerging antiemetic agents or approaches included in the survey, most respondents described interest in learning more about all of them (Table 5). The top choices for all health care providers included gabapentin, olanzapine, and transdermal granisetron. Most hematology/oncology physicians were interested in combination approaches, and most hematology/oncology nurses were interested in the netupitant/palonosetron fixed-dose combination and transdermal granisetron.
Discussion
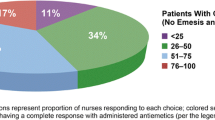
This multinational survey was undertaken with the goal of identifying health care providers’ self-reported knowledge gaps and educational needs in the management of CINV. Perhaps the most noteworthy aspect of this survey is that more than 2,000 health care providers responded and provided in-depth information on their educational needs and interests related to CINV. A growing body of literature describes how survey response rates have been decreasing over time and how some groups of health care providers are reluctant to respond to requests for survey completion [6]. However, the fact that more than 2,000 health care providers responded to this survey attests to the actuality that a well-designed survey targeted to the most relevant audience can engage health care providers. Furthermore, the fact that 47 % of respondents conveyed that more than 25 % of their patients suffered from CINV over the past year underscores the persistent prevalence of this problem and may also explain their willingness to complete this survey (data not shown).
Another noteworthy aspect of this report is the fact that a highly diverse group of health care providers responded to the survey. As anticipated, hematology/oncology physicians and hematology/oncology nurses represented the largest groups of respondents, but health care providers from multiple other specialties and disciplines also participated in the survey. In view of the anticipated shortage of hematologists and medical oncologists in the near future, this finding suggests that future educational initiatives for CINV should be far-reaching and should seek to capture an audience that includes health care providers from multiple disciplines [7]. Although the educational interests and barriers to effective treatment differed among disciplines, these shared interests can be used to develop educational initiatives that serve the needs of a broad range of health care providers. These findings suggest that both focused educational programming that addresses the specific needs and interests of the hematology/oncology community and broader education that addresses the needs of the health care community at large are likely to garner the interest of their intended target audiences.
Relevant to the above observation is the fact that only 10 % of physicians completed the survey. As alluded to above, several large organizations, such as the American Society of Clinical Oncology, have predicted a shortage of oncologists for several years [7]. The fact that the physician response rate to this survey was relatively low may reflect a shift or anticipated shift in cancer supportive care to nursing staff and other health care providers. This low physician response rate only further emphasizes the importance of designing educational efforts that meet the needs of a broad range of health care providers.
This survey identified several gaps that invite the development of educational programs. First, breakthrough nausea and vomiting was a commonly reported area of concern, and delayed nausea appears to be the most problematic from a management standpoint. Health care providers could potentially benefit from educational programs focused on both of these topics, with a discussion of newer antiemetic treatment modalities and their role in management. Second, most respondents indicated that CINV was well controlled in their patients, but a notable percentage also reported the need to delay or stop chemotherapy because of it. This latter survey finding indicates that even fundamental educational initiatives that review guidelines on the prevention and control of CINV may be of value. It also underscores the fact that effective CINV management plays a crucial role in enabling patients to continue to receive chemotherapy. Third, despite the data that demonstrate the comparable efficacy of some oral antiemetics [8], many health care providers voiced a preference for IV administration. Further probing into the reasons for this preference might result in modifications to current curricula in order to provide better understanding of the appropriate role of oral antiemetics. Fourth, identification of numerous barriers to managing CINV could give rise to a vast array of educational efforts on how to overcome such barriers. One such barrier, physician adherence to treatment guidelines, has been reported previously and represents a key target for education intervention [9]. Because one barrier was patients’ poor adherence to CINV treatment, educational tools could serve a dual role of helping inform both patients and health care providers. Lastly, health care providers described a strong interest in learning about newer antiemetics, perhaps illustrating that the cornerstone of management of CINV through the years has been pharmacologic therapy and that expectations run high for learning about new agents that will advance the state of the science and provide practical palliation of symptoms to cancer patients.
This study has both strengths and limitations. With regard to the latter, this survey was developed for this unique project and did not rely on a long list of extensively validated survey questions. Because the survey was aimed at expeditiously assessing educational gaps and quickly acting upon findings, a multistep process of survey validation was not implemented. A second limitation is that several issues, such as adherence to published guidelines, treatment limitations sometimes enforced by institutional guidelines, current cost benefits and disadvantages related to guidelines adherence, and a broader understanding of the patient morbidity associated with poor guideline adherence (extra clinic visits, emergency department visits, or hospitalizations), were not addressed in this survey. Such topics are important and merit further study. A third limitation is that this survey does not have a denominator that permits reporting on the percentage of health care providers who declined to complete the survey. We also recognize that nurses represent the largest proportion of participants and, as a result, their stated educational needs might be setting the agenda for future educational efforts. Nonetheless, with some exceptions, as noted in this manuscript, the needs of hematology/oncology nurses and hematology/oncology physicians were often in alignment or very close. Thus, we believe that the findings reported here have educational value for a broad swath of health care providers.
In summary, this report catalogs responses from more than 2,000 health care providers worldwide and offers valuable information that enables educators to create programs aimed at advancing knowledge and honing the skills of health care providers with the ultimate goal of enabling them to more successfully prevent/manage CINV in patients with cancer.
References
Wintrobe MM, Huguley CM (1948) Nitrogen mustard therapy for Hodgkin’s disease, lymphosarcoma, the leukemias, and other disorders. Cancer 1:357–382
Grunberg SM, Slusher B, Rugo HS (2013) Emerging treatments in chemotherapy-induced nausea and vomiting. Clin Adv Hematol Oncol 11(2 Suppl 1):1–18
Basch E, Hesketh PJ, Kris MG, Prestrud AA, Temin S, Lyman GH (2011) Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 31:4189–4198
Unger JM, Barlow WE, Martin DP, Ramsey SD, Leblanc M, Etzoni R, Hershman DL (2014) Comparison of survival outcomes among cancer patients treated in and out of clinical trials. J Natl Cancer Inst 1;106(3):dju002. doi: 10.1093/jnci/dju002
Grunberg SM, Clark-Snow RA, Koeller J (2010) Chemotherapy-induced nausea and vomiting: contemporary approaches to optimal management: proceedings from a symposium at the 2008 Multinational Association of Supportive Care in Cancer (MASCC) annual meeting. Support Care Cancer 18(Suppl 1):S1–S10
Klabunde CN, Willis GB, Casalino LP (2013) Facilitators and barriers to survey participation by physicians: a call to action for researchers. Eval Health Prof 36:279–295
Hortobagyi GN (2007) A shortage of oncologists? The American Society of Clinical Oncology Workforce Study. J Clin Oncol 25:1468–1469
Boccia R, Grunberg S, Franco-Gonzales E, Rubenstein E, Voisin D (2013) Efficacy of oral palonosetron compared to intravenous palonosetron for the prevention of chemotherapy-induced nausea and vomiting associated with moderately emetogenic chemotherapy: a phase 3 trial. Support Care Cancer 21:1453–1460
Salsman JM, Grunberg SM, Beaumont JL et al (2012) Communicating about chemotherapy-induced nausea and vomiting: a comparison of patient and provider perspectives. J Natl Compr Canc Netw 10:149–157
Conflict of interest
Emily van Laar and Jayashri Desai are employed by Medscape, the company that funded this research. Aminah Jatoi had previously received payment for participation in Medscape educational events that have no relationship to the current study. All the authors have had full access to the primary data and would be willing to share it with the journal upon request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Laar, E.S., Desai, J.M. & Jatoi, A. Professional educational needs for chemotherapy-induced nausea and vomiting (CINV): multinational survey results from 2,388 health care providers. Support Care Cancer 23, 151–157 (2015). https://doi.org/10.1007/s00520-014-2325-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2325-x