Abstract
Background
There is evidence for the efficacy of psycho-oncological interventions (POI) in randomized controlled trials for cancer patients. Our objective was to explore, under naturalistic conditions (using propensity score matching), whether POI are effective to decrease anxiety, depression, distress and overall psychopathological symptoms within cancer patients and their partners.
Methods
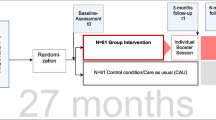
This study was conducted in the Oncology and Hematology Center of a University clinic in Switzerland with a group of 186 patients and 117 partners. Outcome measures of mental health were the Hospital Anxiety and Depression Scale and the Symptom Checklist (SCL-9-K). Repeated-measures ANOVAs were used to analyze change over time and group effects between individuals with POI vs. without POI.
Results
Highly distressed patients and their partners participating in POI reported better mental health over time. Among moderately distressed patients, a decrease over time emerged in depression and distress independent of POI. No effectiveness of POI could be demonstrated in moderately distressed patients and partners.
Conclusion
Most of the highly distressed patients receive additional POI and therefore conclusions about the efficacy of POI are difficult. For moderately distressed individuals, POI as implemented in Switzerland does not improve mental health in such patients and their partners, which may be caused by very time limited POI treatments. Studies with more intense POI treatments are needed.

Similar content being viewed by others
References
Kruse J, Grinschgl A, Wöller W, Söllner W, Keller M (2003) Psychosoziale Interventionen bei Patientinnen mit Brustkrebs. Psychotherapeut 48:93–99
Holland JC (2004) IPOS Sutherland Memorial Lecture: an international perspective on the development of psychosocial oncology: overcoming cultural and attitudinal barriers to improve psychosocial care. Psycho-Oncology 13(7):445–459. doi:10.1002/pon.812
Herschbach P, Heussner P (2008) Einführung in die psychoonkologische Behandlungspraxis. Klett-Cotta, Stuttgart
Kiss A (1995) Psychosocial/psychotherapeutic interventions in cancer patients: consensus statement. Supportive Care in Cancer 3:270–271. doi:10.1007/BF00335903
Künzler A, Lenz G (2010) Psychoonkologie. In: Künzler A, Böttcher C, Hartmann R, Nussbaum MH (eds) Körperzentrierte Psychotherapie im Dialog. Springer, Heidelberg, pp 261–273
Verres R, Schweitzer J, Seemann H, Stammer H, Wischmann T (2002) Minimal-invasives Vorgehen bei der Psychotherapie körperlicher Störungen. In: Strauss B (ed) Psychotherapie bei körperlichen Erkrankungen. Hogrefe, Göttingen, pp 64–78
Rehse B, Pukrop R (2003) Effects of psychosocial interventions on quality of life in adult cancer patients: meta analysis of 37 published controlled outcome studies. Patient Education and Counseling 50:179–186. doi:10.1016/s0738-3991(02)00149-0
Sheard T, Maguire P (1999) The effect of psychological interventions on anxiety and depression in cancer patients: results of two meta-analyses. British Journal of Cancer 80(11):1770–1780
Allen TW (1991) Guide to clinical preventive services. Report of the US Preventive Services Task Force. The Journal of the American Osteopathic Association 91(3):281–289
Shadish WR, Matt GE, Navarro AM, Phillips G (2000) The effects of psychological therapies under clinically representative conditions: a meta-analysis. Psychological Bulletin 126(4):512–529. doi:10.1037//0033-2909.126.4.512
Moynihan C, Bliss JM, Davidson J, Burchell L, Horwich A (1998) Evaluation of adjuvant psychological therapy in patients with testicular cancer: randomised controlled trial. BMJ 316(7129):429–435
Gross CP, Mallory R, Heiat A, Krumholz HM (2002) Reporting the recruitment process in clinical trials: who are these patients and how did they get there? Annals of Internal Medicine 137(1):10–16
Leichsenring F (2004) Randomized controlled versus naturalistic studies: a new research agenda. Bulletin of the Menninger Clinic 68(2):137–151. doi:10.1521/bumc.68.2.137.35952
Seligman ME (1995) The effectiveness of psychotherapy. The Consumer Reports study The American psychologist 50(12):965–974
Heinze G, Juni P (2011) An overview of the objectives of and the approaches to propensity score analyses. European Heart Journal 32(14):1704–1708. doi:10.1093/eurheartj/ehr031
Rosenbaum PM, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70(1):41–55
Herrmann C, Buss U, Snaith RP (1995) Hospital Anxiety and Depression Scale—Deutsche Version (HADS-D). Hans Huber, Bern
Herrmann C (1997) International experiences with the Hospital Anxiety and Depression Scale—a review of validation data and clinical results. Journal of Psychosomatic Research 42(1):17–41
Härter M, Woll S, Wunsch A, Bengel J, Reuter K (2006) Screening for mental disorders in cancer, cardiovascular and musculoskeletal diseases. Comparison of HADS and GHQ-12. Social Psychiatry and Psychiatric Epidemiology 41(1):56–62. doi:10.1007/s00127-005-0992-0
Klaghofer R, Brähler E (2001) Konstruktion und teststatistische Prüfung einer Kurzform der SCL-90-R. Zeitschrift für Klinische Psychologie, Psychiatrie und Psychotherapie 49:115–124
Derogatis L (1992) SCL-90-R, administration, scoring and procedures manual-II for the revised Version. Clinical Psychometric Research, Townson
Sobin LH, Wittekind CH (1997) In: Sobin LH, Wittekind CH (eds) UICC TNM classification of malignant tumours. Wiley-Liss, New York
Herschbach P, Brandl T, Knight L, Keller M (2004) Standardized description of cancer patients' subjective health. Development of a basic documentation for psycho-oncology. Deutsches Ärzteblatt 101:A799–802
Coyne JC, Lepore SJ, Palmer SC (2006) Efficacy of psychosocial interventions in cancer care: evidence is weaker than it first looks. Annals of Behavioral Medicine 32(2):104–110. doi:10.1207/s15324796abm3202_5
Ernstmann N, Neumann M, Ommen O, Galushko M, Wirtz M, Voltz R, Hallek M, Pfaff H (2009) Determinants and implications of cancer patients’ psychosocial needs. Support Care Cancer 17:1417–1423. doi:10.1007/s00520-009-0605-7
Andrykowski MA, Manne SL (2006) Are psychological interventions effective and accepted by cancer patients? I. Standards and levels of evidence. Annals of Behavioral Medicine 32(2):93–97. doi:10.1207/s15324796abm3202_3
Jacobsen PB, Jim HS (2008) Psychosocial interventions for anxiety and depression in adult cancer patients: achievements and challenges. CA: A Cancer Journal for Clinicians 58(4):214–230. doi:10.3322/CA.2008.0003
Luellen JK, Shadish WR, Clark MH (2005) Propensity scores: an introduction and experimental test. Evaluation Review 29(6):530–558. doi:10.1177/0193841x05275596
Zimmermann T, Heinrichs N, Baucom DH (2007) “Does one size fit all?” moderators in psychosocial interventions for breast cancer patients: a meta-analysis. Annals of Behavioral Medicine 34(3):225–239. doi:10.1080/08836610701677188
Acknowledgments
This study was supported by a grant from Krebsliga Aargau (Grant holder; Alfred Künzler, Jürgen Barth). Analysis and interpretation of the results was done independent of the funding institution.
Conflict of interest
No conflict of interest. All authors have full access to the data and take full responsibility for data analysis and interpretation of results. Data from this study can be requested from the Journal.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barth, J., Delfino, S. & Künzler, A. Naturalistic study on the effectiveness of psycho-oncological interventions in cancer patients and their partners. Support Care Cancer 21, 1587–1595 (2013). https://doi.org/10.1007/s00520-012-1700-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-012-1700-8