Abstract
Introduction
To determine whether the annual case volume of general surgeons (greater or less than 200 colonoscopies) is associated with quality outcomes.
Methods
This retrospective cohort study involved all adults who underwent colonoscopy by a surgeon in the city of St. John’s, NL, during the first 6 months of 2012. Subjects were identified through records from the health authority, and data were recorded on a standardized data sheet. Univariate analysis followed by stepwise multivariable logistic regression was performed to determine whether there was an association between quality outcomes (colonoscopy completion rate, adenoma detection rate) and predictors of these outcomes including annual colonoscopy volume, patient age, gender, indication for colonoscopy, and ASA score. A Chi-squared test was used to determine whether other outcomes were associated with annual colonoscopy volume.
Results
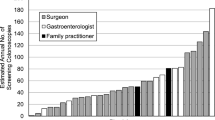
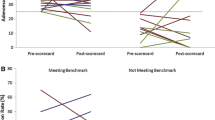
Data were collected on 1060 patients. Mean age was 59.5 (sd 12.2) years with 550 females. A total of 13 surgeons were studied, of which 7 performed less than 200 annual colonoscopies over the previous 2 years (low-volume group) and 6 performed more than 200 annual colonoscopies over the previous 2 years (high-volume group). While there was a significant difference in the colonoscopy completion rate favoring the high-volume group (82.2 vs. 91.1 %, p < 0.001), no difference was noted in the adenoma detection rate between groups (16.7 vs. 17.7 %, p = 0.762). The regression model revealed that colonoscopy completion was also associated with an indication of screening or surveillance and an ASA score of 1 or 2. The adenoma detection rate was associated with older age and male gender. There was no statistically significant association between annual colonoscopy volume and other safety outcome measures.
Conclusion
Performing over 200 colonoscopies annually is associated with higher colonoscopy completion rates, but does not appear to be associated with other quality measures.
Similar content being viewed by others
References
Winawer SJ, Zauber AG, Ho MN, O’Brien MJ, Gottlieb LS, Sternberg SS, Waye JD, Schapiro M, Bond JH, Panish JF, Ackroyd F, Shike M, Kurtz RC, Hornsby-Lewis L, Gerdes H, Stewart ET (1993) Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med 329:1977–1981
Muller AD, Sonnenberg A (2005) Prevention of colorectal cancer by flexible endoscopy and polypectomy. Ann Intern Med 123:904–910
Loeve F, van Ballegooijen M, Snel Habbema JD (2005) Colorectal cancer risk after colonoscopic polypectomy: a population based study and literature search. Eur J Cancer 41:416–422
Robertson DJ, Greenberg ER, Beach M, Sandler RS, Ahnen D, Haile RW, Burke CA, Snover DC, Church TR, Cole BF, Byers T, Mott L, Baron JA (2005) Colorectal cancer in patients under close surveillance. Gastroenterology 129:34–41
Baxter NN, Sutradhar R, Forbes SS, Raszat LF, Saskin R, Rabeneck L (2011) Analysis of administrative data finds endoscopist quality measures associated with post colonoscopy colorectal cancer. Gastroenterology 140(1):65–72
Kaminski MF, Regula J, Kraszewski E, Rupinski M, Pachlewsk J, Wronska E, Bretthawer M, Thomas-Gibson S, Kulper EJ, Rugula J (2010) Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med 362(19):1795–1803
Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, Zauber AG, de Boers J, Firena BH, Schottinger JE, Quinn VP, Ghai NR, Levin TR, Quesenberry CP (2014) Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 370(14):1298–1301
Wexner SD, Garbus JE, Singh JJ (2001) SAGES Colonoscopy Outcomes Group. A prospective analysis of 13,580 colonoscopies. Reevaluation of credentialing guidelines. Surg Endosc 15:251–261
Bhangu A, Bowley M, Horner R, Baranowski E, Raman S, Karandikar S (2012) Volume and accreditation, but not speciality, affect quality standards in colonoscopy. Br J Surg 99:1436–1444
Cancer Care Ontario (2012) ColonCancerCheck 2010 Program Report. www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=156747. Accessed January 2016
The American Board of Surgery (2011) ABS Statement on GI Endoscopy. www.absurgery.org/default.jsp?newsgiresponse. Accessed January 2016
The Canadian Association of General Surgery (2009) Canadian Association of General Surgery Statement on Endoscopy. www.cags-accg.ca/docs/CAGS_Statement_endorsed_june_24.pdf. Accessed January 2016
Ko C, Dominitz J, Green P, Kreuter W, Baldwin L (2010) Speciality differences in polyp detection, removal, and biopsy during colonoscopy. Am J Med 123:528–535
Tinmouth J, Patel J, Hilsden RJ, Ivers N, Llovet D (2016) Audit and feedback interventions to improve endoscopist performance: principles and effectiveness. Best Pract Res Clin Gastroenterol 30(3):473–485
Adler A, Wegscheider K, Leiberman D, Aminalai A, Aschenbeck J, Drossel R, Mayr M, Mrob M, Schee M, Scroder A, Gerber K, Stange G, Roll S, Gauger U, Wiedenmann B, Altenhofen L, Rosch T (2013) Factors determining the quality of screening colonoscopy: a prospective study on adenoma detection rates, from 12,134 examinations (Berlin colonoscopy project, BECOP-3). Gut 62(2):236–241
Aranda-Hernández J, Hwang J, Kandel G (2016) Seeing better-evidence based recommendations on optimizing colonoscopy adenoma detection rate. World J Gastroenterol 22(5):1767–1778
Shah HA, Paszat LF, Saskin R, Strukel TA, Rabeneck L (2007) Factors associated with incomplete colonoscopy: a population based study. Gastroenterology 132:297–303
Chen SC, Rex DK (2007) Endoscopist can be more powerful than age and male gender in predicting adenoma detection at colonoscopy. Gastroenterology 102:1–6
Lee TJ, Rees CJ, Blanks RE, Moss SM, Nickerson C, Wright KC, James PW, McNally RJ, Patrick J, Rutter MD (2014) Colonoscopic factors associated with adenoma detection in a national colorectal cancer screening program. Endoscopy 46(3):203–211
Soulis-Munoz P, Soiis-Herruzo JA, Rodriguez-Munoz S (2014) Experience of the endoscopist increases detection rates of smaller size and higher histological grade polyps. J Gastroenterol Hepatol 29(6):1237–1241
Kaminski MF, Anderson J, Valori R, Kraszewska E, Rupinski M, Pachlewski J, Wronska E, Bretthauer M, Thomas-Gibson S, Kuipers EJ, Regula J (2015) Leadership training to improve adenoma detection rate in screening colonoscopy: a randomised trial. Gut 0:1–9
The Canadian Association of Gastroenterology (2011) Skills Enhancement for Endoscopy. www.cag-acg.org/skills-enhancement-for-endoscopy. Accessed January 2016
Joint Advisory Group (JAG) on GI Endoscopy (2009) JAG Curriculum for Training in Endoscopy Version 2.0. www.thejag.org.uk/LinkClick.aspx?fileticket=sFCpFaN818M%3d&tabid=164. Accessed January 2016
Rabeneck L, Paszat LF, Hilsden RJ, Saskin R, Leddin D, Grunfeld E, Wai E, Goldwasser M, Sutradhar R, Stukle TA (2008) Bleeding and perforation after outpatient colonoscopy and their risk factors in usual clinical practice. Gastroenterology 135(6):1899–1906
Rex DK, Schoenfeld PS, Cohen J, Pike IM, Adler DG, Fennerty MB, Lieb JG, Park WG, Rizk MK, Sawhney MS, Shaheen NJ, Wani S, Weinberg DS (2015) Quality indicators for colonoscopy. Gastrointest Endosc 81:31–53
Moritz V, Bretthauer M, Ruud HK, Glomsaker T, de Lange T, Sandvei P, Huppertz-Hauss G, Kjellevold Ø, Hoff G (2012) Withdrawal time as a quality indicator for colonoscopy—a nationwide analysis. Endoscopy 44:476–481
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr.’s D. Pace, M. Borgaonkar, B. Evans, V. Falk, N. Hickey, M. O’Leary, J. McGrath, D. Boone and medical students M. Lougheed and C. Marcoux have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Pace, D., Borgaonkar, M., Evans, B. et al. Annual colonoscopy volume and maintenance of competency for surgeons. Surg Endosc 31, 2630–2635 (2017). https://doi.org/10.1007/s00464-016-5275-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5275-1