Abstract
Objective
To compare the effectiveness and safety of single-port versus multi-port laparoscopic surgery for treating liver diseases.
Methods
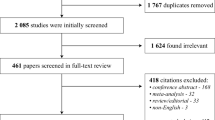
Several databases were systematically searched for randomized controlled trials, cohort studies, and case–control studies on the use of single-port versus multi-port laparoscopic surgery to treat liver diseases from their inception until March 24, 2016. The primary outcomes were the operative time, volume of intraoperative blood loss, rate of postoperative complications, median length of postoperative stay, recovery time of gastrointestinal function, volume of postoperative drainage, and postoperative drainage time. The study-specific effect sizes and their 95 % confidence interval were all combined to calculate the pooled value by using a random-effects model.
Results
A total of nine studies were included, which involved 277 patients. The total and subgroup data were combined by meta-analysis. This meta-analysis showed that single-port and multi-port laparoscopic liver surgery for treating liver diseases did not differ in terms of operative time (P = 0.48), rate of postoperative complications (P = 0.56), median length of postoperative stay (P = 0.80), and recovery time of gastrointestinal function (P = 0.54). For liver diseases, the single-port group exhibited a lower volume of intraoperative blood loss than that presented by the multi-port group (P = 0.0006). In the hepatic resection subgroup, a lower volume of intraoperative blood loss was noted in the single-port group (P < 0.0001). By contrast, in the hepatic cyst subgroup, the single-port group showed a higher volume of intraoperative blood loss (P = 0.02) but a shorter median length of postoperative stay (P = 0.02). The findings of the potential subgroup analysis in these outcomes were consistent with the total data.
Conclusion
Compared with multi-port laparoscopic surgery, the single-port method showed comparable effectiveness and safety for the treatment of liver diseases in terms of current evidence.







Similar content being viewed by others
References
Zhou YM, Shao WY, Zhao YF, Xu DH, Li B (2011) Meta-analysis of laparoscopic versus open resection for hepatocellular carcinoma. Dig Dis Sci 56(7):1937–1943. doi:10.1007/s10620-011-1572-7 (Epub 2011 Jan 23)
Yin Z, Fan X, Ye H, Yin D, Wang J (2013) Short- and long-term outcomes after laparoscopic and open hepatectomy for hepatocellular carcinoma: a global systematic review and meta-analysis. Ann Surg Oncol 20(4):1203–1215. doi:10.1245/s10434-012-2705-8 (Epub 2012 Oct 26)
Xiong JJ, Altaf K, Javed MA, Huang W, Mukherjee R, Mai G, Sutton R, Liu XB, Hu WM (2012) Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. World J Gastroenterol 18(45):6657–6668. doi:10.3748/wjg.v18.i45.6657
Chen J, Bai T, Zhang Y, Xie ZB, Wang XB, Wu FX, Li LQ (2015) The safety and efficacy of laparoscopic and open hepatectomy in hepatocellular carcinoma patients with liver cirrhosis: a systematic review. Int J Clin Exp Med 8(11):20679–20689. http://europepmc.org/abstract/MED/26884991 (eCollection 2015)
Rao A, Rao G, Ahmed I (2011) Laparoscopic left lateral liver resection should be a standard operation. Surg Endosc 25(5):1603–1610. doi:10.1007/s00464-010-1459-2 (Epub 2010 Dec 7)
Edwin B, Nordin A, Kazaryan AM (2011) Laparoscopic liver surgery: new frontiers. Scand J Surg 100(1):54–65. http://www.ncbi.nlm.nih.gov/pubmed/21482506
You Y, Choi H, Na G, Han J, Kim E, Lee S, Hong T, Yoon Y, Kim S, Kim D (2013) Single-port laparoscopic liver resection for hepatocellular carcinoma. Hepatol Int 7:S623. http://www.embase.com.libproxy.tulane.edu:2048/search/results?subaction=viewrecord&rid=6&page=1&id=L71309171
You YK, Kim EY, Lee SH, Park SK, Han JH, Na GH, Choi HJ, Hong TH, Yoon YC, Kim SJ, Kim DG (2015) Single-port laparoscopic liver surgery. Surg Endosc 29:S12. http://www.embase.com.libproxy.tulane.edu:2048/search/results?subaction=viewrecord&rid=7&page=1&id=L71872300
Gkegkes ID, Iavazzo C (2014) Single incision laparoscopic hepatectomy: a systematic review. J Minim Access Surg 10(3):107–112. doi:10.4103/0972-9941.134872
Benzing C, Krenzien F, Atanasov G, Seehofer D, Sucher R, Zorron R, Pratschke J, Schmelzle M (2015) Single incision laparoscopic liver resection (sill)—a systematic review. GMS Interdiscip Plast Reconstr Surg DGPW. doi:10.3205/iprs000076 (eCollection 2015)
Hu M, Zhao G, Wang F, Xu D, Liu R (2014) Single-port and multi-port laparoscopic left lateral liver sectionectomy for treating benign liver diseases: a prospective, randomized, controlled study. World J Surg 38(10):2668–2673. doi:10.1007/s00268-014-2610-3
Higgins JPT, Green S (eds) (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. www.cochrane-handbook.org
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. doi:10.1007/s10654-010-9491-z (Epub 2010 Jul 22)
Aldrighetti L, Ratti F, Catena M, Pulitanò C, Ferla F, Cipriani F, Ferla G (2012) Laparoendoscopic single site (LESS) surgery for left-lateral hepatic sectionectomy as an alternative to traditional laparoscopy: case-matched analysis from a single center. Surg Endosc 26(7):2016–2022. doi:10.1007/s00464-012-2147-1
Choi HJ, You YK, Na GH, Hong TH, Shetty GS, Kim DG (2012) Single-port laparoscopy-assisted donor right hepatectomy in living donor liver transplantation: sensible approach or unnecessary hindrance? Transplant Proc 44(2):347–352. doi:10.1016/j.transproceed.2012.01.018
Wu S, Li Y, Tian Y, Li M (2014) Single-incision laparoscopic surgery versus standard laparoscopic surgery for unroofing of hepatic cysts. JSLS 18(2):246–251. doi:10.4293/108680813X13753907291512
Yu XP, Wu SD, Wang P, Su Y, Yu H, Chen YS, Lv C (2013) Comparison of single-incision and multi-incision laparoscopic liver resection. Chin J Curr Adv Gen Surg 16(08):602–605. doi:10.3969/j.issn.1009-9905.2013.08.005
Li YN, Wu SD, Tian Y, Xie B, Li M (2013) Retrospective control study of single-incision vs multi-incision laparoscopic fenestration in nonparasitic hepatic cysts. Chin J Curr Adv Gen Surg 16(1):31–35. doi:10.3969/j.issn.1009-9905.2013.01.010
Wu ZY, Hu H, Jin CG, Ouyang CG, Zhang LG, Gao W, Wei XJ, An FD (2015) Clinical application of the laparoscopic hepatic resection in 29 patients through different surgical routes. China J Endosc 21(6):657–660. http://d.wanfangdata.com.cn/Periodical/zgnjzz201506024
Xiao ZY (2014) Comparison of the clinical outcomes of the transumbilical versus multi-port laparoscopic liver resection. J Bethune Med Sci 12(1):67–68. http://d.wanfangdata.com.cn/Periodical/bqnjyxyxb201401048
Zhang F (2015) Clinical application of the single-port laparoscopic surgery. China Contemp Med 21(36):79–80. http://d.wanfangdata.com.cn/Periodical/ddyx201536048
Jimenez Rodriguez RM, Segura-Sampedro JJ, Flores-Cortés M, López-Bernal F, Martín C, Diaz VP, Ciuro FP, Ruiz JP (2016) Laparoscopic approach in gastrointestinal emergencies. World J Gastroenterol 22(9):2701–2710. doi:10.3748/wjg.v22.i9.2701
Magge D, Zureikat A, Hogg M, Zeh HJ 3rd (2016) Minimally invasive approaches to pancreatic surgery. Surg Oncol Clin N Am 25(2):273–286. doi:10.1016/j.soc.2015.11.001
Machado MA, Surjan RC, Makdissi FF (2014) Intrahepatic glissonian approach for single-port laparoscopic liver resection. J Laparoendosc Adv Surg Tech A 24(8):534–537. doi:10.1089/lap.2013.0539 (Epub 2014 Jun 13)
Ban D, Kudo A, Irie T, Ochiai T, Aihara A, Matsumura S, Tanaka S, Tanabe M (2015) Advances in reduced port laparoscopic liver resection. Asian J Endosc Surg 8(1):11–15. doi:10.1111/ases.12164 (Epub 2014 Dec 15)
Tayar C, Subar D, Salloum C, Malek A, Laurent A, Azoulay D (2014) Single incision laparoscopic hepatectomy: advances in laparoscopic liver surgery. J Minim Access Surg 10(1):14–17. doi:10.4103/0972-9941.124454
Kimura T, Matuda Y, Inoue M, Koida S, Matsuoka N, Ushimaru Y, Kato Y (2015) Introduction of single site laparoscopic partial hepatectomy in patient with hepatocellular carcinoma. Surg Endosc 29:S194. http://www.embase.com.libproxy.tulane.edu:2048/search/results?subaction=viewrecord&rid=1&page=1&id=L71873028
You Y, Kim EY, Lee SH, Lee JS, Park SK, Han JH, Na GH, Choi HJ, Hong TH, Yoon YC, Kim DG, Park JH, Lee SK, Kim SJ, Park IY, Ryeu DD, Kim KW, Baek KY, Park JW (2015) Single center experience of 120 single-port laparoscopic liver resections. HPB (Oxford) 17:278. http://www.embase.com.libproxy.tulane.edu:2048/search/results?subaction=viewrecord&rid=1&page=1&id=L71822125
Lee SH, Kim EY, Park SK, Han JH, Na GH, Choi HJ, Hong TH, Yoon YC, Kim DG, You YK (2014) Single-port laparoscopic liver surgeries. Surg Endosc 28:374. http://www.embase.com.libproxy.tulane.edu:2048/search/results?subaction=viewrecord&rid=4&page=1&id=L71480283
Weiss M, Mittermair C, Brunner E, Schirnhofer J, Obrist C, Pimpl K, Hell T, Weiss H (2015) Inline radiofrequency pre-coagulation simplifies single-incision laparoscopic minor liver resection. J Hepatobiliary Pancreat Sci 22(12):831–836. doi:10.1002/jhbp.295 (Epub 2015 Nov 18)
Miyazawa M, Aikawa M, Okada K, Toshimitsu Y, Okamoto K, Takase K, Yamaguchi S, Koyama I (2011) Method of expanding applications in single incisional laparoscopic hepatectomy: the utility of radio wave pre-coagulation and soft coagulation. Surg Endosc 25:S370. http://www.embase.com.libproxy.tulane.edu:2048/search/results?subaction=viewrecord&rid=1&page=1&id=L70470575
Tanabe M, Kawachi S, Itano O, Shinoda M, Kitago M, Wada N, Kitagawa Y (2012) Needle-assisted single-incision laparoscopic (naslap) liver surgery. Surg Endosc 26:S350. http://www.embase.com.libproxy.tulane.edu:2048/search/results?subaction=viewrecord&rid=1&page=1&id=L71482526
Tanabe M, Abe Y, Hibi T, Itano O, Shinoda M, Kitago M, Yagi H, Wada N, Kitagawa Y (2013) New paradigm in laparoscopic liver resection: the ‘‘pouch-in-a-pouch’’ technique. Surg Endosc 27:S407. http://www.embase.com.libproxy.tulane.edu:2048/search/results?subaction=viewrecord&rid=1&page=1&id=L71044987
Weiss HG, Schirnhofer J, Bunner W, Biebl M, Pimpl K, Mittermair C, Obrist C, Hell T (2013) Wound complications in 1127 consecutive transumbilical laparoscopic single incision procedures. Surg Endosc 27:S14. http://www.embase.com.libproxy.tulane.edu:2048/search/results?subaction=viewrecord&rid=1&page=1&id=L71045940
Schirnhofer J, Brunner W, Mittermair C, Pimpl K, Kronberger IK, Laimer E, Klaus A, Weiss H (2011) The learning curve in single incision laparoscopic surgery. Surg Endosc 25:S51. http://www.embase.com.libproxy.tulane.edu:2048/search/results?subaction=viewrecord&rid=8&page=1&id=L70470845
Antoniou SA, Morales-Conde S, Antoniou GA, Granderath FA, Berrevoet F, Muysoms FE, Bonham Group (2016) Single-incision laparoscopic surgery through the umbilicus is associated with a higher incidence of trocar-site hernia than conventional laparoscopy: a meta-analysis of randomized controlled trials. Hernia 20(1):1–10. doi:10.1007/s10029-015-1371-8 (Epub 2015 Apr 7)
Acknowledgments
We thank Jin Xia and Jian-Ying Zhang for assistance in statistical analysis. We also thank Professor Jian-Ping Gong and Co-chief superintendent nurse Xiao-Mei Wang for modifying our initial manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Yun-Bing Wang, Jin Xia, Jian-Ying Zhang, Jian-Ping Gong, and Xiao-Mei Wang have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Wang, YB., Xia, J., Zhang, JY. et al. Effectiveness and safety of single-port versus multi-port laparoscopic surgery for treating liver diseases: a meta-analysis. Surg Endosc 31, 1524–1537 (2017). https://doi.org/10.1007/s00464-016-5199-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5199-9