Abstract
Background
The quality of a total mesorectal excision (TME) is one of the most important prognostic factors for local recurrence of rectal carcinoma. The aim of this study was to clarify the manner in which lesser pelvis dimensions affect the quality of TME via the transabdominal approach, while simultaneously defining the criteria for selecting patients most likely to have Grade 3 TME outcomes for a transanal approach using the TaTME technique.
Methods
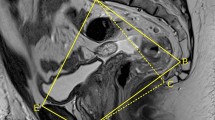
An analysis from the registry was conducted using 93 of total 198 patients with rectal cancer of the mid- and lower third of the rectum who underwent: (1) a low anterior resection, (2) an ultra-low resection with coloanal anastomosis, or (3) an intersphincteric rectal resection, all with total mesorectal excision. The procedures were carried out at the Department of Surgery at the University Hospital Hradec Králové between 2011 and 2014. Rectal specimens were histopathologically examined according to a standardized protocol. Pelvimetry data were obtained using anteroposterior, transverse, and sagittal CT or MRI scans.
Results
A correlation was found between the quality of the TME and pelvimetry parameter A5, i.e., the angle between the longitudinal axis of the symphysis, and the lines between the symphysis and the promontory (R 2 = −0.327, p < 0.001). The ordinal regression method was used to identify parameters of the model describing levels of probability for TME quality. These relationships were described by equations that provide probability of the achievement of each grade of TME.
Conclusion
The correlation described by obtained equations between pelvimetry parameters and the quality of TME represents a new tool for use in preoperative decision-making with regard to resection via the transanal approach (TaTME).


Similar content being viewed by others
References
Laurent C, Leblanc F, Wütrich P, Scheffler M, Rullier E (2009) Laparoscopic versus open surgery for rectal cancer: long-term oncologic results. Ann Surg 250:54–61. doi:10.1097/SLA.0b013e3181ad6511
Parfitt JR, Driman DK (2007) The total mesorectal excision specimen for rectal cancer: a review of its pathological assessment. J Clin Pathol 60:849–855. doi:10.1136/jcp.2006.043802
Lin H-H, Lin J-K, Lin C-C, Lan Y-T, Wang H-S, Yang S-H, Jiang J-K, Chen W-S, Lin T-C, Liang W-Y, Chang S-C (2013) Circumferential margin plays an independent impact on the outcome of rectal cancer patients receiving curative total mesorectal excision. Am J Surg 206:771–777. doi:10.1016/j.amjsurg.2013.03.009
Leonard D, Penninckx F, Fieuws S, Jouret-Mourin A, Sempoux C, Jehaes C, Van Eycken E (2010) Factors predicting the quality of total mesorectal excision for rectal cancer. Ann Surg 252:982–988. doi:10.1097/SLA.0b013e3181efc142
Jeyarajah S, Sutton CD, Miller AS, Hemingway D (2007) Factors that influence the adequacy of total mesorectal excision for rectal cancer. Colorectal Dis 9:808–815. doi:10.1111/j.1463-1318.2007.01256.x
Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, Ueno M, Miyata S, Yamaguchi T (2009) Factors affecting the difficulty of laparoscopic total mesorectal excision with double stapling technique anastomosis for low rectal cancer. Surgery 146:483–489. doi:10.1016/j.surg.2009.03.030
Ogiso S, Yamaguchi T, Hata H, Fukuda M, Ikai I, Yamato T, Sakai Y (2011) Evaluation of factors affecting the difficulty of laparoscopic anterior resection for rectal cancer: “narrow pelvis” is not a contraindication. Surg Endosc 25:1907–1912. doi:10.1007/s00464-010-1485-0
Veenhof AAFA, Engel AF, van der Peet DL, Sietses C, Meijerink WJHJ, de Lange-de Klerk ESM, Cuesta MA (2008) Technical difficulty grade score for the laparoscopic approach of rectal cancer: a single institution pilot study. Int J Colorectal Dis 23:469–475. doi:10.1007/s00384-007-0433-5
Seki Y, Ohue M, Sekimoto M, Takiguchi S, Takemasa I, Ikeda M, Yamamoto H, Monden M (2007) Evaluation of the technical difficulty performing laparoscopic resection of a rectosigmoid carcinoma: visceral fat reflects technical difficulty more accurately than body mass index. Surg Endosc 21:929–934. doi:10.1007/s00464-006-9084-9
Akiyoshi T, Watanabe T, Ueno M (2011) Pelvic dimensions as a predictor of difficulty in laparoscopic surgery for rectal cancer. Surg Endosc 25:3122–3123. doi:10.1007/s00464-011-1649-6
Brannigan AE, De Buck S, Suetens P, Penninckx F, D’Hoore A (2006) Intracorporeal rectal stapling following laparoscopic total mesorectal excision: overcoming a challenge. Surg Endosc 20:952–955. doi:10.1007/s00464-005-0536-4
Targarona EM, Balague C, Pernas JC, Martinez C, Berindoague R, Gich I, Trias M (2008) Can we predict immediate outcome after laparoscopic rectal surgery? Multivariate analysis of clinical, anatomic, and pathologic features after 3-dimensional reconstruction of the pelvic anatomy. Ann Surg 247:642–649. doi:10.1097/SLA.0b013e3181612c6a
Atallah S, Albert M, Larach S (2010) Transanal minimally invasive surgery: a giant leap forward. Surg Endosc 24:2200–2205. doi:10.1007/s00464-010-0927-z
Atallah S, Albert M, Debeche-Adams T, Larach S (2013) Transanal minimally invasive surgery (TAMIS): applications beyond local excision. Tech Coloproctol 17:239–243. doi:10.1007/s10151-012-0945-z
Atallah S, Albert M, DeBeche-Adams T, Nassif G, Polavarapu H, Larach S (2013) Transanal minimally invasive surgery for total mesorectal excision (TAMIS-TME): a stepwise description of the surgical technique with video demonstration. Tech Coloproctol 17:321–325. doi:10.1007/s10151-012-0971-x
McLemore EC, Coker AM, Devaraj B, Chakedis J, Maawy A, Inui T, Talamini MA, Horgan S, Peterson MR, Sylla P, Ramamoorthy S (2013) TAMIS-assisted laparoscopic low anterior resection with total mesorectal excision in a cadaveric series. Surg Endosc 27:3478–3484. doi:10.1007/s00464-013-2889-4
Lim S-B, Seo S-I, Lee JL, Kwak JY, Jang TY, Kim CW, Yoon YS, Yu CS, Kim JC (2012) Feasibility of transanal minimally invasive surgery for mid-rectal lesions. Surg Endosc 26:3127–3132. doi:10.1007/s00464-012-2303-7
Killeen T, Banerjee S, Vijay V, Al-Dabbagh Z, Francis D, Warren S (2010) Magnetic resonance (MR) pelvimetry as a predictor of difficulty in laparoscopic operations for rectal cancer. Surg Endosc 24:2974–2979. doi:10.1007/s00464-010-1075-1
Wang C, Xiao Y, Qiu H, Yao J, Pan W (2014) Factors affecting operating time in laparoscopic anterior resection of rectal cancer. World J Surg Oncol 12:44. doi:10.1186/1477-7819-12-44
Boyle KM, Petty D, Chalmers AG, Quirke P, Cairns A, Finan PJ, Sagar PM, Burke D (2005) MRI assessment of the bony pelvis may help predict resectability of rectal cancer. Colorectal Dis 7:232–240. doi:10.1111/j.1463-1318.2005.00819.x
Salerno G, Daniels IR, Brown G, Norman AR, Moran BJ, Heald RJ (2007) Variations in pelvic dimensions do not predict the risk of circumferential resection margin (CRM) involvement in rectal cancer. World J Surg 31:1313–1320. doi:10.1007/s00268-007-9007-5
Salerno G, Daniels IR, Brown G, Heald RJ, Moran BJ (2006) Magnetic resonance imaging pelvimetry in 186 patients with rectal cancer confirms an overlap in pelvic size between males and females. Colorectal Dis 8:772–776. doi:10.1111/j.1463-1318.2006.01090.x
Acknowledgments
Supported by MH CZ-DRO (UHHK, 00179906).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Prof. Alexander Ferko and Drs. Ondřej Malý, Július Örhalmi and Josef Dolejš have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Ferko, A., Malý, O., Örhalmi, J. et al. CT/MRI pelvimetry as a useful tool when selecting patients with rectal cancer for transanal total mesorectal excision. Surg Endosc 30, 1164–1171 (2016). https://doi.org/10.1007/s00464-015-4324-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4324-5