Abstract
Background
Endoscopic forceps biopsy is insufficient for a definitive diagnosis of dysplastic lesions. It is difficult to decide clinical management of gastric indefinite neoplasia diagnosed by endoscopic forceps biopsy when early gastric cancer (EGC) is macroscopically suspected. The aim of this study was to discuss the final results of gastric indefinite neoplasia and associated clinical factors predictive of early gastric cancer.
Methods
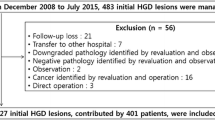
The medical records of 119 patients who were diagnosed with gastric indefinite neoplasia by index forceps biopsy were retrospectively reviewed. The initial endoscopic findings were analyzed, and predictive factors of EGC were evaluated.
Results
The final pathologic diagnoses of 119 patients included early gastric cancer (n = 26, 21.8 %), adenoma (n = 6, 5.0 %) and non-neoplasm (n = 87, 73.1 %). Univariate analysis showed that lesion size greater than 10 mm, surface nodularity and surface redness were associated risk factors. In the multivariate analysis, lesions diameter (p = 0.021, OR 11.401, 95 % CI 1.432–90.759) and surface redness (p = 0.014, OR 3.777, 95 % CI 1.306–10.923) were significant risk factors.
Conclusions
Patients with gastric indefinite neoplasia with larger size (≥10 mm) and surface redness might need further diagnostic investigation rather than simple follow-up endoscopy.



Similar content being viewed by others
References
Hull MJ, Mino-Kenudson M, Nishioka NS, Ban S, Sepehr A, Puricelli W, Nakatsuka L, Ota S, Shimizu M, Brugge WR, Lauwers GY (2006) Endoscopic mucosal resection: an improved diagnostic procedure for early gastroesophageal epithelial neoplasms. Am J Surg Pathol 30:114–118
Yoshida S, Kozu T, Gotoda T, Saito D (2006) Detection and treatment of early cancer in high-risk populations. Best Pract Res Clin Gastroenterol 20:745–765
Dixon MF (2002) Gastrointestinal epithelial neoplasia: Vienna revisited. Gut 51:130–131
Choi CW, Kim HW, Shin DH, Kang DH, Hong YM, Park JH, Park SB, Cho M, Lee JH (2014) The risk factors for discrepancy after endoscopic submucosal dissection of gastric category 3 lesion (low grade dysplasia). Dig Dis Sci 59:421–427
Participants in the Paris Workshop (2003) The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointestinal endoscopy 58:S3–S43
Shimada H, Okazumi S, Koyama M, Murakami K (2011) Japanese Gastric Cancer Association Task Force for Research Promotion: clinical utility of (1)(8)F-fluoro-2-deoxyglucose positron emission tomography in gastric cancer. A systematic review of the literature. Gastric Cancer 14:13–21
Kato M, Nishida T, Tsutsui S, Komori M, Michida T, Yamamoto K, Kawai N, Kitamura S, Zushi S, Nishihara A, Nakanishi F, Kinoshita K, Yamada T, Iijima H, Tsujii M, Hayashi N (2011) Endoscopic submucosal dissection as a treatment for gastric noninvasive neoplasia: a multicenter study by Osaka University ESD Study Group. J Gastroenterol 46:325–331
Szaloki T, Toth V, Tiszlavicz L, Czako L (2006) Flat gastric polyps: results of forceps biopsy, endoscopic mucosal resection, and long-term follow-up. Scand J Gastroenterol 41:1105–1109
Rugge M, Farinati F, Baffa R, Sonego F, Di Mario F, Leandro G, Valiante F (1994) Gastric epithelial dysplasia in the natural history of gastric cancer: a multicenter prospective follow-up study. Interdisciplinary Group on Gastric Epithelial Dysplasia. Gastroenterology 107:1288–1296
de Vries AC, van Grieken NC, Looman CW, Casparie MK, de Vries E, Meijer GA, Kuipers EJ (2008) Gastric cancer risk in patients with premalignant gastric lesions: a nationwide ohort study in the Netherlands. Gastroenterology 134:945–952
Gotoda T, Yamamoto H, Soetikno RM (2006) Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol 41:929–942
Choi CW, Kim HW, Kang DH, Hong YM, Kim SJ, Park SB, Cho M, Kim DJ, Hong JB (2014) Clinical outcomes of second-look endoscopy after gastric endoscopic submucosal dissection: predictive factors with high risks of bleeding. Surg Endosc 28:2213–2220
Chung IK, Lee JH, Lee SH, Kim SJ, Cho JY, Cho WY, Hwangbo Y, Keum BR, Park JJ, Chun HJ, Kim HJ, Kim JJ, Ji SR, Seol SY (2009) Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc 69:1228–1235
Cho SJ, Choi IJ, Kim CG, Lee JY, Kook MC, Park S, Ryu KW, Lee JH, Kim YW (2011) Risk of high-grade dysplasia or carcinoma in gastric biopsy-proven low-grade dysplasia: an analysis using the Vienna classification. Endoscopy 43:465–471
Park DI, Rhee PL, Kim JE, Hyun JG, Kim YH, Son HJ, Kim JJ, Paik SW, Rhee JC, Choi KW, Oh YL (2001) Risk factors suggesting malignant transformation of gastric adenoma: univariate and multivariate analysis. Endoscopy 33:501–506
Goldstein NS, Lewin KJ (1997) Gastric epithelial dysplasia and adenoma: historical review and histological criteria for grading. Hum Pathol 28:127–133
Nakayoshi T, Tajiri H, Matsuda K, Kaise M, Ikegami M, Sasaki H (2004) Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video). Endoscopy 36:1080–1084
Tahara T, Shibata T, Nakamura M, Yoshioka D, Okubo M, Arisawa T, Hirata I (2009) Gastric mucosal pattern by using magnifying narrow-band imaging endoscopy clearly distinguishes histological and serological severity of chronic gastritis. Gastrointest Endosc 70:246–253
Disclosures
Goo Ja Jun, Cheol Woong Choi, Dae Hwan Kang, Hyung Wook Kim, Su Bum Park, Mong Cho, Sun Hwi Hwang and Si Hak Lee have no conflicts of interest or financial ties to disclose.
Acknowledgments
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by Ministry for Health & Welfare, Republic of Korea (grant number: HI12C1845).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goo, J.J., Choi, C.W., Kang, D.H. et al. Risk factors associated with diagnostic discrepancy of gastric indefinite neoplasia: Who need en bloc resection?. Surg Endosc 29, 3761–3767 (2015). https://doi.org/10.1007/s00464-015-4151-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4151-8