Abstract
Background
Transoral incisionless fundoplication (TIF) treats gastroesophageal reflux disease (GERD) by creating a full-thickness esophagogastric plication using transmural fasteners. If unsuccessful, revision laparoscopic anti-reflux surgery (rLARS) may be performed. This study evaluated operative findings and clinical outcomes of rLARS in 28 patients with prior primary TIF.
Methods
Intraoperative findings, complications, and symptomatic outcomes with GERD health-related quality of life (GERD-HRQL) were evaluated prospectively in patients having rLARS after TIF. Results are median with interquartile range (IQR).
Results
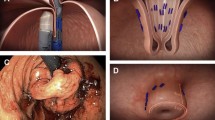
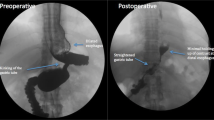
Between 03/2009 and 08/2013, 28 patients underwent rLARS at 14 (13–50) months post-TIF for recurrent symptoms after initial improvement. Pre-rLARS endoscopies found hiatal hernia (9) and wrap disruption (12). All revisions were completed laparoscopically in 88 (70–90) min. Eight patients underwent partial fundoplication, the rest Nissen. No intraoperative or postoperative complications occurred. Operative findings included: No axial hernia in 65 %; Dense adhesions in 14 %; Fasteners incorporating the lateral crus in 95 %; Traction diverticuli from esophagus to crura in 21 %. Residual plication was noted anteriorly in 75 %, posteriorly in 0 %. Operative approaches: (1) Areas where the TIF fundoplication remained were left intact. This necessitated rolling the fundoplication over the fused area to prevent an endoscopic appearance of ‘fold’. (2) Fasteners were cut and left to migrate into the lumen, rather than being pulled out. (3) In 8 patients with fusion of the lateral crus to TIF fundoplication and no axial hernia, revision fundoplication was performed without mediastinal mobilization but with posterior hernia repair. One patient required subsequent surgery for small paraesophageal hernia, one for refractory gas-bloat after rLARS. Dysphagia in 2 patients resolved with dilation. GERD-HRQL improved from a median of 20 (8–27) pre-TIF and 10 (1–20) pre-rLARS to 3 (0–4) at 28 months (12–40) post-rLARS (p = 0.020 for pre-rLARS to post-rLARS).
Conclusion
rLARS after TIF can be performed safely with excellent clinical outcomes.





Similar content being viewed by others
References
Wendling MR, Melvin WS, Perry KA (2013) Impact of transoral incisionless fundoplication (TIF) on subjective and objective GERD indices: a systematic review of the published literature. Surg Endosc 27:3754–3761
Witteman BP, Kessing BF, Snijders G, Koek GH, Conchillo JM, Bouvy ND (2013) Revisional laparoscopic antireflux surgery after unsuccessful endoscopic fundoplication. Surg Endosc 27:2231–2236
Furnee EJ, Broeders JA, Draaisma WA, Schwartz MP, Hazebroek EJ, Smout AJ, van Rijn PJ, Broeders IA (2010) Laparoscopic Nissen fundoplication after failed EsophyX fundoplication. Br J Surg 97:1051–1055
Bell RC, Cadiere GB (2011) Transoral rotational esophagogastric fundoplication: technical, anatomical, and safety considerations. Surg Endosc 25:2387–2399
Bell RC, Hanna P, Powers B, Sabel J, Hruza D (1996) Clinical and manometric results of laparoscopic partial (Toupet) and complete (Rosetti–Nissen) fundoplication. Surg Endosc 10:724–728
Bell RC, Hanna P, Mills MR, Bowrey D (1999) Patterns of success and failure with laparoscopic Toupet fundoplication. Surg Endosc 13:1189–1194
Bell RC, Fearon J, Freeman KD (2013) Allograft dermal matrix hiatoplasty during laparoscopic primary fundoplication, paraesophageal hernia repair, and reoperation for failed hiatal hernia repair. Surg Endosc 27:1997–2004
Oelschlager BK, Pellegrini CA, Hunter J, Soper N, Brunt M, Sheppard B, Jobe B, Polissar N, Mitsumori L, Nelson J, Swanstrom L (2006) Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg 244:481–490
Frantzides CT, Madan AK, Carlson MA, Stavropoulos GP (2002) A prospective, randomized trial of laparoscopic polytetrafluoroethylene (PTFE) patch repair vs. simple cruroplasty for large hiatal hernia. Arch Surg 137:649–652
Granderath FA, Schweiger UM, Kamolz T, Asche KU, Pointner R (2005) Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: preliminary results of a prospective randomized functional and clinical study. Arch Surg 140:40–48
Velanovich V (1998) Comparison of generic (SF-36) vs. disease-specific (GERD-HRQL) quality-of-life scales for gastroesophageal reflux disease. J Gastrointest Surg 2:141–145
Galmiche JP, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, Langstrom G, Lind T, Lundell L, Collaborators LT (2011) Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA 305:1969–1977
Bell RC, Mavrelis PG, Barnes WE, Dargis D, Carter BJ, Hoddinott KM, Sewell RW, Trad KS, Da Costa Gill B, Ihde GM (2012) A prospective multicenter registry of patients with chronic gastroesophageal reflux disease receiving transoral incisionless fundoplication. J Am Coll Surg 215:794–809
Wilson EB, Barnes WE, Mavrelis PG, Carter BJ, Bell RC, Sewell RW, Ihde GM, Dargis D, Hoddinott KM, Shughoury AB, Gill BD, Fox MA, Turgeon DG, Freeman KD, Gunsberger T, Hausmann MG, Leblanc KA, Deljkich E, Trad KS (2014) The effects of transoral incisionless fundoplication on chronic GERD patients: 12-month prospective multicenter experience. Surg Laparosc Endosc Percutan Tech 24:36–46
Hoppo T, Immanuel A, Schuchert M, Dubrava Z, Smith A, Nottle P, Watson DI, Jobe BA (2010) Transoral incisionless fundoplication 2.0 procedure using EsophyX for gastroesophageal reflux disease. J Gastrointest Surg 14:1895–1901
Bell RC, Freeman KD (2011) Clinical and pH-metric outcomes of transoral esophagogastric fundoplication for the treatment of gastroesophageal reflux disease. Surg Endosc 25:1975–1984
Perry KA, Linn JG, Eakin JL, Onders RP, Velanovich V, Melvin WS (2013) Transoral incisionless fundoplication does not significantly increase morbidity of subsequent laparoscopic Nissen fundoplication. J Laparoendosc Adv Surg Tech A 23:456–458
Disclosures
Dr. Reginald CW Bell, Dr. Ashwin A Kurian, and Ms. Katherine Freeman NP have no conflicts of interest or financial ties to disclose.
Funding
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bell, R.C.W., Kurian, A.A. & Freeman, K.D. Laparoscopic anti-reflux revision surgery after transoral incisionless fundoplication is safe and effective. Surg Endosc 29, 1746–1752 (2015). https://doi.org/10.1007/s00464-014-3897-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3897-8