Abstract
Background
We hypothesized that an esophageal nitinol stent that is mainly silicone-covered but partially uncovered may allow tissue ingrowth and decrease the migration rate seen with fully covered stents and still allow safe stent removal. The aim of this study was to evaluate the first human results of using partially covered stents for anastomotic complications of bariatric surgery.
Methods
This was a retrospective evaluation of all patients with staple-line complications after bariatric surgery who received a partly covered stent at a single tertiary-care bariatric center. The stents varied in length from 10 to 15 cm and in diameter from 18 to 23 mm.
Results
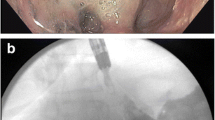
From April 2009 to April 2010, eight patients received partially covered stents on 14 separate occasions. The indications were gastrojejunal stricture in four, acute leak in two, acute leak followed by a later stricture in one, and a perforated anastomotic ulcer in one patient. Single stents were placed in 12 sessions and two overlapping stents in two sessions. At the time of stent deployment, one patient had the uncovered proximal end of the stent in the stomach, with all others in the distal esophagus. Immediate symptom improvement occurred in 12/14 stent placements. Oral nutrition was initiated for 10/14 stent treatments within 48 h. Stents were removed after 25 ± 10 days. Minor stent displacement occurred with 9/13 stents, with the proximal end of the stent moving into the stomach, though the site of pathology remained covered. The stents were difficult to remove when tissue ingrowth was present. One patient required laparoscopic removal and one required two endoscopy sessions for removal. At the time of removal of ten stents, where the proximal end was found in the stomach, four had gastric ulceration, three had gastric mucosa replaced by granulation tissue, and three had normal gastric mucosa. In four cases where the proximal portion of the stent stayed in the esophagus, the esophageal deployment zone had abnormalities: three with granulation tissue and one with denuding of the esophageal mucosa. The distal uncovered portion of the stent in the Roux limb never became embedded in the mucosa and caused minimal injury.
Conclusions
A partially covered stent was successful in keeping the site of the pathology covered and provided rapid symptom improvement and oral nutrition in most patients. The proximal end of the stent generally moved from the esophagus to the stomach, probably due to esophageal peristalsis. The proximal uncovered portion of the stent causes significant bowel mucosal injury and sometimes becomes embedded in the esophagus or the stomach, making removal difficult. We no longer use partially covered stents.



Similar content being viewed by others
References
DeMaria EJ, Sugarman HJ, Kellum JM, Meador JG, Wolf LG (2002) Results of 281 consecutive total laparoscopic Roux-en-Y gastric bypasses to treat morbid obesity. Ann Surg 235(5):640–645
Gonzalez RS, Smith CD, Baghai M, Kendrick M, Szomstein S, Rosenthal R, Murr MM (2007) Diagnosis and contemporary management of anastomotic leaks after gastric bypass for obesity. J Am Coll Surg 204(1):47–55
Fukumoto R, Orlina J, McGinty J, Teixeira J (2007) Use of polyflex stents in treatment of acute esophageal and gastric leaks after bariatric surgery. Surg Obes Relat Dis 3(1):68–72
Edwards C, Bui P, Astudillo JA, de la Torre R, Miedema B, Ramaswamy A, Fearing N, Ramshaw B, Thaler K, Scott JS (2008) Management of anastomotic leaks after Roux-en-Y bypass using self expanding polyester stents. Surg Obes Relat Dis 4(5):594–599
Eubanks WS, Edwards CA, de la Torre RA, Thaler K, Miedema BW, Scott JS (2008) Use of endoscopic stents to treat anastomotic complications after bariatric surgery. J Am Coll Surg 206:935–938
Efthimiou E, Stein L, Szego P, Court O, Christou N (2009) Stent migration causing alimentary limb obstruction necessitating laparotomy and surgical stent extraction. Surg Obes Relat Dis 5(3):375–377
Iqbal A, Miedema B, Ramaswamy A, Fearing N, de la Torre R, Pak Y, Stephen C, Thaler K (2011) Long-term outcome after endoscopic stent therapy for complications after bariatric surgery. Surg Endosc 25(2):515–520
Hirdes MM, Siersema PD, Houben MHMG, Weusten BLAM, Vleggaar FP (2011) Stent-in-stent technique for removal of embedded esophageal self-expanding mental stents. Am J Gastroenterol 106:286–293
Hirdes MM, Vleggaar FP, Van der Linde K, Willems M, Totté ER, Siersema PD (2011) Esophageal perforation due to removal of partially covered self-expanding metal stents placed for a benign perforation or leak. Endoscopy 43(2):156–159
Acknowledgments
The authors thank Stacy Turpin for her expertise in developing the illustrations.
Disclosure
Drs. Wei Wei, Archana Ramaswamy, Roger de la Torre, and Brent Miedema have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wei, W., Ramaswamy, A., de la Torre, R. et al. Partially covered esophageal stents cause bowel injury when used to treat complications of bariatric surgery. Surg Endosc 27, 56–60 (2013). https://doi.org/10.1007/s00464-012-2406-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2406-1