Abstract
Background
We have prospectively collected information concerning the costs incurred during the management of patients allocated to either forceful dilatation or to an immediate laparoscopic operation because of newly diagnosed achalasia.
Methods
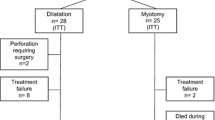
Fifty-one patients with newly diagnosed achalasia were randomized to either pneumatic dilatation to a diameter of 30–40 mm or to a laparoscopic myotomy to which was added a posterior partial fundoplication. Follow-ups were scheduled at 1, 3, 6, and 12 months after inclusion. At each follow-up visit a study nurse interviewed the patients regarding symptoms and their quality of life (QoL) and a health economic questionnaire was completed. In the latter questionnaire, patients were asked to report the presence and character of contacts with the healthcare system since the last visit.
Results
In the dilatation group six patients (23%), including the patient who was operated on because of perforation, were classified as failures during the first 12 months of follow-up compared to one (4%) in the myotomy group (p = 0.047). Five of those classified as failures in the dilatation group subsequently had a surgical myotomy and the sixth patient was treated with repeated dilatations. The patient classified as failure in the myotomy group was treated with endoscopic dilatation. The initial treatment cost and the total costs were significantly higher for laparoscopic myotomy compared to a pneumatic dilatation-based strategy (p = 0.0002 and p = 0.0019, respectively) When the total costs were subdivided into the different resources used, we found that the single largest cost item for pneumatic dilatation was that for hospital stay and that for laparoscopic myotomy was the actual operative treatment (operating room time) The cost-effectiveness analysis, relating to the actual treatment failures, revealed that the cost to avoid one treatment failure (incremental cost-effectiveness ratio) amounted to €9239.
Conclusion
The current prospective, controlled clinical trial shows that despite a higher level of clinical efficacy of laparoscopic myotomy to prevent treatment failure in newly diagnosed achalasia, the cost effectiveness of pneumatic dilatation is superior, at least when a reasonable time horizon is applied.

Similar content being viewed by others
References
Sonnenberg A, Massey BT, McCarty DJ, Jacobsen SJ (1993) Epidemiology of hospitalisation for achalasia in the United States. Dig Dis Sci 38:233–244
Mayberry JF, Atkinson M (1987) Variations in the prevalence of achalasia in Great Britain and Ireland: an epidemiological study based on hospital admissions. Q J Med 62:67–74
Howard PJ, Maher L, Pryde A, Cameron EW, Heading RC (1992) Five years prospective study of the incidence, clinical features, and diagnosis of achalasia in Edinburgh. Gut 33:1011–1015
Ben-Meir A, Urbach DR, Khajanchee YS, Hansen PD, Swanstrom LL (2001) Quality of life before and after laparoscopic Heller myotomy for achalasia. Am J Surg 181:471–474
Urbach DR, Tomlinson GA, Harnish JL, Martino R, Diamant NE (2005) A measure of disease-specific health related quality of life for achalasia. Am J Gastroenterol 100:1668–1676
Spiess AE, Kahrilas PJ (1998) Treating achalasia: from whalebone to laparoscope. JAMA 280:638–642
Abir F, Modlin I, Kidd M, Bell R (2004) Surgical treatment of achalasia: current status and controversies. Dig Surg 21:165–176
Vantrappen G, Hellemans J, Deloof W, Valembois P, Vandenbroucke J (1971) Treatment of achalasia with pneumatic dilatations. Gut 121:268–275
Bonavina L, Nosadini A, Bardini R, Baessato M, Peracchia A (1992) Primary treatment of esophageal achalasia. Long-term results of myotomy and Dor fundoplication. Arch Surg 127:222–226
Patti MG, Fisichella PM, Perretta S, Galvani C, Gorodner MV, Robinson T, Way LW (2003) Impact of minimally invasive surgery on the treatment of esophageal achalasia: a decade of change. J Am Coll Surg 196:698–703
Dimenäs E, Carlsson G, Glise H, Israelsson B, Wiklund I (1996) Relevance of norm values as part of the documentation of quality of life instruments for use in upper gastrointestinal disease. Scand J Gastroenterol Suppl 221:8–13
Dimenas E (1993) Methological aspects of evaluation of quality of life in upper gastrointestinal diseases. Scan J Gastroenterol Suppl 199:18–21
Patrick DL, Deyo RA (1989) Generic and disease-specific measures in assessing health status and quality of life. Med Care 27(Suppl):217–232
Dupuy HJ (1984) The Psychological General Well-Being (PGWB) index. In: Wenger NK, Mattson ME, Furberg CF (eds) Assessment of Quality of Life in Clinical Trials of Cardiovascular Therapies. LeJacq Publishing Inc., New York, pp 170–183
Svedlund J, Sjödin I, Dotevall G (1988) GSRS: a clinical rating scale for gastrointestinal symtoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig Dis Sci 33:129–134
Svedlund J, Sullivan M, Sjodin I, Liedman B, Lundell L (1996) Quality of life in gastric cancer prior to gastrectomy. Qual Life Res 5:255–264
Korolija D, Sauerland S, Wood-Dauphinee S, Abbou CC, Eypasch E, Gareia Caballero M, Lumsden MA, Millat B, Monson JRT, Nilsson G, Pointer R, Schwenk W, Shamiyeh A, Szold A, Targarona E, Ure B, Neugebauer E (2004) Surg Endosc 18:879–897
Parkman HP, Reynolds JC, Ouyang A, Rosato EF, Eisenberg JM, Cohen S (1993) Pneumatic dilatation or esophagomyotomy treatment for idiopathic achalasia: clinical outcomes and cost analysis. Dig Dis Sci 38:75–85
O’Connor JB, Singer ME, Imperiale TF, Vaezi MF, Richter JE (2002) The cost-effectiveness of treatment strategies for achalasia. Dig Dis Sci 47:1516–1525
Imperiale TF, O’Connor JB, Vaezi MF, Richter JE (2000) A cost-minimization analysis of alternative treatment strategies for achalasia. Am J Gastroenterol 95:2737–2745
Draaisma WA, Buskens E, Bais JE, Simmermacher RK, Rijnhart-de Jong HG, Broeders IA, Gooszen HG (2006) Randomized clinical trial and follow-up study of cost-effectiveness of laparoscopic versus conventional Nissen fundoplication. Br J Surg 93:690–697
Myrvold HE, Lundell L, Miettinen P, Pedersen SA, Liedman B, Hatlebakk J, Julkunen R, Levander K, Lamm M, Mattson C, Carlsson J, Stahlhammar NO (2001) The cost of long term therapy for gastro-oesophageal reflux disease: a randomised trial comparing omeprazole and open antireflux surgery. Gut 49:488–494
van Hout BA, Al MJ, Gordon GS, Rutten FF (1994) Costs, effects and C/E-ratios alongside a clinical trial. Health Econ 3:309–319
Weinstein MC, Stason WB (1977) Foundations of cost-effectiveness analysis for health and medical practices. N Engl J Med 296:716–721
Brauer CA, Rosen AB, Greenberg D, Neumann PJ (2006) Trends in the measurement of health utilities in published cost-utility analyses. Value Health 4:213–218
Richards KF, Fisher KS, Flores JH, Christensen BJ (1996) Laparoscopic Nissen fundoplication: cost, morbidity, and outcome compared with open surgery. Surg Laparosc Endosc 6:140–143
Romagnuolo J, Meier MA, Sadowski DC (2002) Medical or surgical therapy for erosive reflux esophagitis: cost-utility analysis using a Markov model. Ann Surg 236:191–202
Van Den Boom G, Go PM, Hameeteman W, Dallemagne B, Ament AJ (1996) Cost effectiveness of medical versus surgical treatment in patients with severe or refractory gastroesophageal reflux disease in the Netherlands. Scand J Gastroenterol 31:1–9
Csendes A, Braghetto I, Burdiles P, Korn O, Csendes P, Henriquez A (2006) Very late results of esophagomyotomy for patients with achalasia. Ann Surg 243:196–203
Csendes A, Braghetto I, Henriquez A, Cortes C (1989) Late results of a prospective randomised study comparing forceful dilatation and esophagomyotomy in patients with achalasia of the esophagus. Gut 30:299–300
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kostic, S., Johnsson, E., Kjellin, A. et al. Health economic evaluation of therapeutic strategies in patients with idiopathic achalasia: results of a randomized trial comparing pneumatic dilatation with laparoscopic cardiomyotomy. Surg Endosc 21, 1184–1189 (2007). https://doi.org/10.1007/s00464-007-9310-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9310-0