Abstract
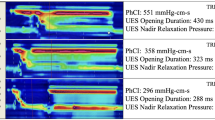
The motility of the pharynx, upper esophageal sphincter (UES), and proximal esophagus in patients with oropharyngeal dysphagia is still not entirely understood. High-resolution manometry (HRM) was recently added to the armamentarium for the study of this area. This study aims to describe HRM findings in patients with vagal paralysis. Sixteen patients (mean age 54 years, 69% females) with oropharyngeal dysphagia due to unilateral vagal paralysis were prospectively studied. All patients underwent HRM. Motility of the UES and at the topography of the velopharynx and epiglottis were recorded. (1) UES relaxation is compromised in a minority of patients, (2) epiglottis pressure does not follow a specific pattern, (3) vellum is hypotonic in half of the patients, (4) dysphagia is related to a low pharyngeal pressure, not to a flow obstruction at the level of the UES, and (5) aspiration is related to low pressures at the level of the UES and epiglottis and higher pressures at the level of the vellum. Pharyngeal motility is significantly impaired in patients with oropharyngeal dysphagia and unilateral vagal paralysis. In half of the cases, UES resting pressure is preserved due to unilateral innervation and relaxation is normal in most patients. Dysphagia therapy in these patients must be directed toward improvement in the oropharyngeal motility not at the UES.



Similar content being viewed by others
References
Shaw SM, Martino R. The normal swallow: muscular and neurophysiological control. Otolaryngol Clin N Am. 2013;46(6):937–56.
Heitmiller R, Tseng E, Jones B. Prevalence of aspiration and laryngeal penetration in patients with unilateral vocal fold motion impairment. Dysphagia. 2000;15:184–7.
Tabaee A, Murry T, Zschommler A, Desloge RB. Flexible endoscopic evaluation of swallowing with sensory testing in patients with unilateral vocal fold immobility: incidence and pathophysiology of aspiration. Laryngoscope. 2005;115(4):565–9.
Leder S, Suiter D, Duffey D, Judson B. Vocal fold immobility and aspiration status: a direct replication study. Dysphagia. 2012;27(2):265–70.
Leder SB, Ross DA. Incidence of vocal fold immobility in patients with dysphagia. Dysphagia 2005;20(2):163–7; discussion 168–9.
Kupfer R, Meyer K. Evaluation of unilateral vocal fold immobility. Curr Otorhinolaryngol Rep. 2014;2:105–13.
Silva LC, Herbella FA, Neves LR, Vicentine FP, Neto SP, Patti MG. Anatomophysiology of the pharyngo-upper esophageal area in light of high-resolution manometry. J Gastrointest Surg. 2013;17(12):2033–8.
Wilson JA, Pryde A, White A, Maher L, Maran AG. Swallowing performance in patients with vocal fold motion impairment. Dysphagia. 1995;10(3):149–54.
Castell JA, Castell DO, Duranceau CA, Topart P. Manometric characteristics of the pharynx, upper esophageal sphincter, esophagus, and lower esophageal sphincter in patients with oculopharyngeal muscular dystrophy. Dysphagia. 1995;10(1):22–6.
Henderson RD, Boszko A, VanNostrand AW, Pearson FG. Pharyngoesophageal dysphagia and recurrent laryngeal nerve palsy. J Thorac Cardiovasc Surg. 1974;68(4):507–12.
Herbella FA, Patti MG. Can high resolution manometry parameters for achalasia be obtained by conventional manometry? World J Gastrointest Pathophysiol. 2015;6(3):58–61.
Takasaki K, Umeki H, Enatsu K, Kumagami H, Takahashi H. Evaluation of swallowing pressure in a patient with amyotrophic lateral sclerosis before and after cricopharyngeal myotomy using high-resolution manometry system. Auris Nasus Larynx. 2010;37(5):644–7.
Nativ-Zeltzer N, Logemann JA, Zecker SG, Kahrilas PJ. Pressure topography metrics for high resolution pharyngeal esophageal manofluorography—a normative study of younger and older adults. Neurogastroenterol Motil. 2016;28(5):721–31.
Hila A, Castell JA, Castell DO. Pharyngeal and upper esophageal sphincter manometry in the evaluation of dysphagia. J Clin Gastroenterol. 2001;33(5):355–61.
Mu L, Sanders I. Neuromuscular organization of the human upper esophageal sphincter. Ann Otol Rhinol Laryngol. 1998;107(5 Pt 1):370–7.
Mu L, Sanders I. The innervation of the human upper esophageal sphincter. Dysphagia. 1996;11(4):234–8.
Lang IM, Shaker R. Anatomy and physiology of the upper esophageal sphincter. Am J Med. 1997;103(5A):50S–5S.
Omari TI, Dejaeger E, van Beckevoort D, Goeleven A, Davidson GP, Dent J, Tack J, Rommel N. A method to objectively assess swallow function in adults with suspected aspiration. Gastroenterology. 2011;140(5):1454–63. doi:10.1053/j.gastro.2011.02.051.
Acknowledgements
We are indebted to Ms. Vanessa Tuxen for her invaluable assistance with the esophageal tests.
Author’s contribution
BRP: conception and design, acquisition of data, analysis and interpretation of data, drafting the article, final approval of the version to be published. FAMH: conception and design, acquisition of data, analysis and interpretation of data, drafting the article, final approval of the version to be published. NB: conception and design, review for intellectual content, final approval of the version to be published. TCGV: review for intellectual content, final approval of the version to be published. MGP: review for intellectual content, final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Pinna, B.R., Herbella, F.A.M., de Biase, N. et al. High-Resolution Manometry Evaluation of Pressures at the Pharyngo-upper Esophageal Area in Patients with Oropharyngeal Dysphagia Due to Vagal Paralysis. Dysphagia 32, 657–662 (2017). https://doi.org/10.1007/s00455-017-9811-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9811-5