Abstract
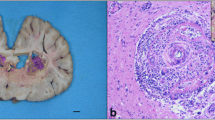
Halicephalobus gingivalis (H. gingivalis) causes a rare and fatal infection in horses and humans. Despite the zoonotic potential and severity of the disease, the epidemiology and pathogenesis of halicephalobiasis are still poorly understood. Several European cases of equine halicephalobiasis have been documented; however, in South-Eastern European countries, including Romania, equine neurohelminthiasis caused by H. gingivalis has not been previously described. Two Lipizzaner horses with a clinical history of progressive neurological signs were referred to the Pathology Department of the Cluj-Napoca (Romania) for necropsy. Both horses died with severe neurological signs. Gross examination and cytological, histological, and molecular analyses were performed. The stallions came from two different breeding farms. No history of traveling outside Romania was recorded. At necropsy, granulomatous and necrotizing lesions were observed in the kidneys, lymph nodes, brain, retroperitoneal adipose tissue, and lungs, indicating a systemic infection. Parasitological and histopathological analyses evidenced larval and adult forms of rhabditiform nematodes consistent with Halicephalobus species. Parasites were observed in both lymph and blood vessels of different organs and were also identified in urine samples. A subunit of the large-subunit ribosomal RNA gene (LSU rDNA) of H. gingivalis (673 bp) was amplified from lesions in both horses.
To the authors’ knowledge, this is the first report of equine systemic H. gingivalis infection in Romania and in South-Eastern Europe. Our findings provide new insights into the geographic distribution of specific genetic lineages of H. gingivalis, while also raising public health awareness, as the parasite is zoonotic.


Similar content being viewed by others
References
Adedeji AO, Borjesson DL, Kozikowski-Nicholas TA, Cartoceti AN, Prutton J, Aleman M (2015) What is your diagnosis? Cerebrospinal fluid from a horse. Vet Clin Pathol 44:171–172
Akagami M, Shibahara T, Yoshiga T, Tanaka N, Yaguchi Y, Onuki T, Kondo T, Yamanaka T, Kubo M (2007) Granulomatous nephritis and meningoencephalomyelitis caused by Halicephalobus gingivalis in a pony gelding. J Vet Med Sci 69:1187–1190
Anderson RC, Linder KE, Peregrine AS (1998) Halicephalobus gingivalis (Stefanski, 1954) from a fatal infection in a horse in Ontario, Canada with comments on the validity of H. deletrix and a review of the genus. Parasite 5:255–261
Andrássy I (1984) Klasse Nematoda. Gustav Fischer Verlag, Stuttgart, p 509
Anwar MA, Gokozan HN, Ball MK, Otero J, McGwire BS (2015) Fatal human eosinophilic meningo-encephalitis caused by CNS co-infection with Halicephalobus gingivalis and West Nile virus. Parasitol Int 64:417–420
Bröjer JT, Parsons DA, Linder KE, Peregrine AS, Dobson H (2000) Halicephalobus gingivalis encephalomyelitis in a horse. Can Vet J 41:559–561
Bryant UK, Lyons ET, Bain FT, Hong CB (2006) Halicephalobus gingivalis-associated meningoencephalitis in a Thoroughbred foal. J Vet Diagn Invest 18:612–615
Dame JB, Cutler TJ, Tanhauser S, Ellison S, Greiner EC, MacKay RJ (2000) Equine protozoal myeloencephalitis: mystery wrapped in enigma. Parasitol Res 86:940–943
Di Francesco G, Savini G, Maggi A, Cavaliere N, D’Angelo AR, Marruchella G (2012) Equine meningo-encephalitis caused by Halicephalobus gingivalis: a case report observed during West Nile disease surveillance activities. Vet Ital 48:437–442
Eydal M, Bambir SH, Sigurdarson S, Gunnarsson E, Svansson V, Fridriksson S, Benediktsson ET, Sigurdardóttir ÓG (2012) Fatal infection in two Icelandic stallions caused by Halicephalobus gingivalis (Nematoda: Rhabditida). Vet Parasitol 186:523–527
Ferguson R, van Dreumel T, Keystone JS, Manning A, Malatestinic A, Caswell JL, Peregrine AS (2008) Unsuccessful treatment of a horse with mandibular granulomatous osteomyelitis due to Halicephalobus gingivalis. Can Vet J 49:1099–1103
Fonderie P, Bert W, Hendrickx F, Houthoofd W, Moens T (2012) Anthelmintic tolerance in free-living and facultative parasitic isolates of Halicephalobus (Panagrolaimidae). Parasitology 139:1301–1308
George LW (1990) Diseases of the nervous system. In: Smith BP (ed) Large animal internal medicine. Mosby Co. St. Louis, MO, pp 901–1045
Henneke C, Jespersen A, Jacobsen S, Nielsen MK, McEvoy F, Jensen HE (2014) The distribution pattern of Halicephalobus gingivalis in a horse is suggestive of a haematogenous spread of the nematode. Acta Vet Scand 19:56
Hermosilla C, Coumbe KM, Habershon-Butcher J, Schöniger S (2011) Fatal equine meningoencephalitis in the United Kingdom caused by the panagrolaimid nematode Halicephalobus gingivalis: case report and review of the literature. Equine Vet J 43:759–763
Isaza R, Schiller CA, Stover J, Smith PJ, Greiner EC (2000) Halicephalobus gingivalis (Nematoda) infection in a Grevy’s zebra (Equus grevyi). J Zoo Wildl Med 31:77–81
Jung JY, Lee KH, Rhyoo MY, Byun JW, Bae YC, Choi E, Kim C, Jean YH, Lee MH, Yoon SS (2014) Meningoencephalitis caused by Halicephalobus gingivalis in a thoroughbred gelding. J Vet Med Sci 76:281–284
Kinde H, Mathews M, Ash L, St Leger J (2000) Halicephalobus gingivalis (H. deletrix) infection in two horses in southern California. J Vet Diagn Invest 12:162–165
Kuzmina TA (2012) Contamination of the environment by strongylid (Nematoda: Strongylidae) infective larvae at horse farms of various types in Ukraine. Parasitol Res 110:1665–1674
Lim CK, Crawford A, Moore CV, Gasser RB, Nelson R, Koehler AV, Bradbury RS, Speare R, Dhatrak D, Weldhagen GF (2015) First human case of fatal Halicephalobus gingivalis meningoencephalitis in Australia. J Clin Microbiol 53:1768–1774
Lyons ET, Tolliver SC (2014) Prevalence of patent Strongyloides westeri infections in Thoroughbred foals in 2014. Parasitol Res 113:4163–4164
Monoranu CM, Müllges W, Keppler M, Brehm K, Ondrejka SL, Muntau B, Tannich E, Müller-Hermelink HK, Tappe D (2015) Fatal human meningoencephalitis due to Halicephalobus nematodes. Open Forum Infect Dis 2, Germany, ofv061
Montgomery D, O’Toole D (2006) Neurological disease in a cow in Big Horn Basin due to a free-living nematode. Wyoming State Veterinary Laboratory Newsletter 7(1):3–4
Muller S, Grzybowski M, Sager H, Bornand V, Brehm W (2008) A nodular granulomatous posthitis caused by Halicephalobus sp. in a horse. Vet Dermatol 19:44–48
Nadler SA, Carreno RA, Adams BJ, Kinde H, Baldwin JG, Mundo-Ocampo M (2003) Molecular phylogenetics and diagnosis of soil and clinical isolates of Halicephalobus gingivalis (Nematoda: Cephalobina: Panagrolaimoidea), an opportunistic pathogen of horses. Int J Parasitol 33:1115–1125
Papadi B, Boudreaux C, Tucker JA, Mathison B, Bishop H, Eberhard ME (2013) Halicephalobus gingivalis: a rare cause of fatal meningoencephalomyelitis in humans. Am J Trop Med Hyg 88:1062–1064
Pearce SG, Bouré LP, Taylor JA, Peregrine AS (2001) Treatment of a granuloma caused by Halicephalobus gingivalis in a horse. J Am Vet Med Assoc 219:1735–1738
Schmitz DG, Chaffin MK (2004) What is your diagnosis? J Am Vet Med Assoc 225:1667–1668
Spalding MG, Greiner EC, Green SL (1990) Halicephalobus (Micronema) deletrix infection in 2 half sibling foals. J Am Vet Med Assoc 196:1127–1129
Acknowledgments
This paper was published under the frame of European Social Fund, Human Resources Development Operational Program 2007–2013, project no. POSDRU/159/1.5/S/136893.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Taulescu, M.A., Ionicã, A.M., Diugan, E. et al. First report of fatal systemic Halicephalobus gingivalis infection in two Lipizzaner horses from Romania: clinical, pathological, and molecular characterization. Parasitol Res 115, 1097–1103 (2016). https://doi.org/10.1007/s00436-015-4839-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-015-4839-7