Abstract
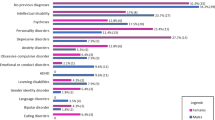
Fragile-X-syndrome (FXS) is caused by a mutation on the X chromosome (Xq27.3). Males with a full mutation have typical dysmorphic signs, moderate intellectual disability and psychological disorders. Twenty-five to fifty percent are affected by incontinence. The aim of the study was to assess subtypes of incontinence and psychological problems in children with FXS in their home environments. Twenty-two boys with FXS (mean age 11.0 years) and 22 healthy controls (mean age 11.1 years) were examined with sonography, uroflowmetry, 48-h bladder diary, physical examination, IQ test, parental psychiatric interview and questionnaires regarding incontinence and psychological symptoms in a home setting. Boys with FXS had higher rates of incontinence than controls (59.1 vs. 4.8 %). The most common subtypes in FXS boys were primary non-monosymptomatic nocturnal enuresis, urge incontinence and nonretentive faecal incontinence. 90.9 % boys with FXS had a psychological comorbidity. Incontinence and behavioural symptoms were not associated.
Conclusion: Boys with FXS have a higher risk for physical disabilities, psychological disorders and incontinence than healthy boys. Constipation is not a major problem in FXS. As effective treatment is available for children with ID, we recommend offering assessment and therapy to all children with FXS and incontinence.
What is Known: |
• Boys with fragile-X-syndrome (FXS) have higher rates of incontinence, psychological disorders and somatic conditions than typically developing boys. |
What is New: |
• Constipation is a rare condition in FXS in contrast to other genetic syndromes. |
• Although incontinence rates are higher, urological findings (uroflowmetry, sonography) are not more pathological per se in FXS. |
Similar content being viewed by others
Abbreviations
- DSM-5:
-
Fifth edition of the Diagnostic and Statistical Manual of Mental Disorders
- DUI:
-
Daytime urinary incontinence
- DV:
-
Dysfunctional voiding
- FI:
-
Faecal incontinence
- FI-C:
-
Faecal incontinence and constipation
- FI-NR:
-
Nonretentive faecal incontinence
- FXS:
-
Fragile-X-syndrome
- ICCS:
-
International Children’s Continence Society
- ID:
-
Intellectual disability
- LUTS:
-
Lower urinary tract symptoms
- NE:
-
Nocturnal enuresis
- OAB:
-
Overactive bladder
- UI:
-
Urge incontinence
- VP:
-
Voiding postponement
References
Achenbach TM (1991) Manual for the child behavior checklist/4–18 and 1991 profile. University of Vermont, Burlington, VT
American Psychiatric Association (APA) (2013) Diagnostic and statistical manual of mental disorders—fifth edition (DSM 5). APA, Washington, D.C.
Arbeitsgruppe Deutsche Child Behavior Checklist (1999) Deutsche Bearbeitung der Child Behavior Checklist (CBCL/4-18) – Einführung und Anleitung zur Handauswertung. Arbeitsgruppe Kinder-, Jugend- und Familiendiagnostik, Köln
Austin PF, Bauer SB, Bower W, Chase J, Franco I, Hoebeke P, Rittig S, Walle JV, von Gontard A, Wright A, Yang SS, Nevéus T (2015) The standardization of terminology of lower urinary tract function in children and adolescents: update report from the standardization Committee of the International Children’s Continence Society. Neurourol Urodyn. doi:10.1002/nau.22751
Backes M, Genç B, Schreck J, Doerfler W, Lehmkuhl G, Von Gontard A (2000) Cognitive and behavioral profile of fragile X boys: correlations to molecular data. Am J Med Genet 95:150–156
Bölte S, Poustka F (2006) FSK - Fragebogen zur Sozialen Kommunikation - Autismus Screening. Verlag Hans Huber, Bern
Brown T (2002) The molecular biology of the fragile X mutation. In: Hagerman RJ, Hagerman PJ (eds) Fragile X syndrome: diagnosis, treatment, and research. Johns Hopkins University Press, Baltimore
Brushini H, Faria N, Garcez E, Srougi M (2003) Development of bladder control in mentally handicapped children. International Braz J Urol 29:455–458
Davis JP, Judd FK, Herrman H (1997) Depression in adults with intellectual disability. Part 1: A review. Aust N Z J Psychiatry 31:232–242
De Gennaro M, Niero M, Capitanucci ML, Von Gontard A, Woodward M, Tubaro A, Abrams P (2010) Validity of the international consultation on incontinence questionnaire-pediatric lower urinary tract symptoms: a screening questionnaire for children. J Urol 184:1662–1667
Duker PC, Dekkers M (1992) Development of diurnal bladder control in severely and profoundly mentally handicapped residents. J Intellect Disabil Res 36:177–181
Einfeld S, Tonge B (1995) Manual for the developmental behaviour checklist—primary carer version (DBC-P) & teacher version (DBC-T). Monash University Centre for Developmental Psychiatry and Psychology, Clayton, Melbourne
Equit M, Piro-Hussong A, Niemczyk J, Curfs L, Von Gontard A (2013) Elimination disorders in persons with Prader-Willi and fragile-X syndromes. Neurourol Urodyn 32:986–992
Equit M, Sambach H, Von Gontard A (2011) Fragile X syndrome and elimination disorders in a 6-year-old girl. Klin Padiatr 223:430–433
Gabis LV, Baruch YK, Jokel A, Raz R (2011) Psychiatric and autistic comorbidity in fragile X syndrome across ages. J Child Neurol 26:940–948
Gallagher A, Hallahan B (2012) Fragile X-associated disorders: a clinical overview. J Neurol 259:401–413
Hagerman RJ, Jackson III AW, Levitas A, Rimland B, Braden M (1986) An analysis of autism in fifty males with the fragile X syndrome. Am J Med Genet 23:359–374
Jarvelin MR, Vikevainen-Tervonen L, Moilanen I, Huttunen N (1988) Enuresis in seven-year-old children. Acta Paediatr Scand 77:148–153
Joinson C, Heron J, Emond A, Butler R (2007) Psychological problems in children with bedwetting and combined (day and night) wetting: a UK population-based study. J Pediatr Psychol 32:605–616
Joinson C, Heron J, Butler U, Von Gontard A (2006) Psychological differences between children with and without soiling problems. Pediatrics 117:1575–1584
Joinson C, Heron J, Von Gontard A (2006) Psychological problems in children with daytime wetting. Pediatrics 118:1985–1993
Kidd SA, Lachiewicz A, Barbouth D, Blitz RK, Delahunty C, McBrien D, Visootsak J, Berry-Kravis E (2014) Fragile X syndrome: a review of associated medical problems. Pediatrics 134:995–1005
Koskentausta T, Iivanainen M, Almqvist F (2004) CBCL in the assessment of psychopathology in Finnish children with intellectual disability. Res Dev Disabil 25:341–354
Kuczmarski R, Ogden CL, Grummer-Strawn LM (2000) CDC growth charts: United States. National Center for Health Statistics, Hyattsville, MD
Kuhn S, Natale N, Siemer S, Stoeckle M, Von Gontard A (2009) Clinical differences in daytime wetting subtypes: urge incontinence and postponed voiding. J Urol 182:1967–1972
Moeschler JB, Shevell M, Schaefer GB, Bull MJ, Enns GM, Gruen JR, Hersh JH, Mendelsohn NJ, Saal HM, Goldberg JD, Hanson JW, Lloyd-Puryear MA, Rasmussen SA, Spire P (2006) Clinical genetic evaluation of the child with mental retardation or developmental delays. Pediatrics 117:2304–2316
Moore SW (2008) Down syndrome and the enteric nervous system. Pediatr Surg Int 24:873–883
Morris CA, Demsey SA, Leonard CO, Dilts C, Blackburn BL (1988) Natural history of Williams syndrome: physical characteristics. J Pediatr 113:318–326
Nevéus T, von Gontard A, Hoebeke P, Hjälmås K, Bauer S, Bower W, Jørgensen TM, Rittig S, Walle JV, Yeung C, Djurhuus JC (2006) The standardization of terminology of lower urinary tract function in children and adolescents: report from the standardisation committee of the International Children’s Continence Society. J Urol 176:314–324
Radstaake M, Didden R, Giesbers S, Korzilius H, Peters-Scheffer N, Lang R, von Gontard A, Curfs LMG (2013) Incontinence in individuals with Angelman syndrome: a comparative study. Res Dev Disabil 34:4184–4193
Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, Walker LS (2006) Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology 130:1527–1537
Raven J, Raven JC, Court JH (2006) Raven’s progressive matrices und vocabulary scales. Harcourt Test Services, Frankfurt
Raven JC (1998) Standard progressive matrices. Beltz-Test, Göttingen
Schneider S, Margraf J, Unnewehr S (1995) Kinder-DIPS: Diagnostisches Interview bei psychischen Störungen von Kindern und Jugendlichen. Springer, Berlin
Smith L, Smith P, Lee SKY (2000) Behavioural treatment of urinary incontinence and encopresis in children with learning disabilities: transfer of stimulus control. Dev Med Child Neurol 42:276–279
Tranfaglia MR (2011) The psychiatric presentation of fragile X: evolution of the diagnosis and treatment of the psychiatric comorbidities of fragile X syndrome. Dev Neurosci 33:337–348
Turner G, Webb T, Wake S, Robinson H (1996) Prevalence of fragile X syndrome. Am J Med Genet 64:196–197
van Laecke E, Raes A, Vande Walle J, Hoebeke P (2009) Adequate fluid intake, urinary incontinence, and physical and/or intellectual disability. J Urol 182:2079–2084
von Gontard A (2013) Urinary incontinence in children with special needs. Nature Reviews Urology 10:667–674
von Gontard A (2012) Enuresis. In: Rey JM (ed) IACAPAP e-textbook of child and adolescent mental health. International Association for Child and Adolescent Psychiatry and Allied Professions, Geneva
von Gontard A (2012) Encopresis. In: Rey JM (ed) IACAPAP e-Textbook of Child and Adolescent Mental Health. International Association for Child and Adolescent Psychiatry and Allied Professions, Geneva
von Wendt L, Simila S, Niskanen P, Jarvelin M (1990) Development of bowel and bladder control in the mentally retarded. Dev Med Child Neurol 32:515–518
Yang PY, Meng NH, Chou ECL (2010) Voiding dysfunctions in children with mental retardation. Neurourol Urodyn 29:1272–1275
Yeung CK, Sreedhar B, Leung VT, Metreweli C (2004) Ultrasound bladder measurements in patients with primary nocturnal enuresis: a urodynamic and treatment outcome correlation. J Urol 171:2589–2594
Yeung C, Sreedhar B, Leung Y-V, Sit K-F (2007) Correlation between ultrasonographic bladder measurements and urodynamic findings in children with recurrent urinary tract infection. BJU Int 99:651–655
Zink S, Freitag CM, von Gontard A (2008) Behavioral comorbidity differs in subtypes of enuresis and urinary incontinence. J Urol 179:295–298
Acknowledgments
We would like to thank the German support group ‘Interessengemeinschaft Fragiles-X e. V.’ and their chairman Dr. Jörg Richstein for giving us the opportunity to cooperate and conduct this study with the help of the members of the support group.
Authors’ individual contribution to the paper
Niemczyk, Justine: Protocol and project development, data management and data analysis, manuscript writing and editing
von Gontard, Alexander: Protocol and project development, data management, manuscript writing and editing
Equit, Monika: Protocol and project development, data analysis, manuscript editing
Bauer, Katharina: Data collection and management
Naumann, Teresa: Data collection and management
Wagner, Catharina: Protocol and project development, data management
Curfs, Leopold: Protocol and project development, manuscript editing
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The Department of Child and Adolescent Psychiatry, Saarland University Hospital, received financial support from Novartis AG to conduct this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the present study have been approved by the local ethics committee and were in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Communicated by Jaan Toelen
Rights and permissions
About this article
Cite this article
Niemczyk, J., von Gontard, A., Equit, M. et al. Detailed assessment of incontinence in boys with fragile-X-syndrome in a home setting. Eur J Pediatr 175, 1325–1334 (2016). https://doi.org/10.1007/s00431-016-2767-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-016-2767-x