Abstract
Anaphylaxis remains under-diagnosed and under-treated. A better knowledge of patterns and triggers of anaphylaxis might contribute to a better management. In this study we evaluated the demographic and clinical features of anaphylaxis in pediatric patients, as well as its triggers and therapeutic approach. From May 1st 2004 until April 30th 2006 we prospectively collected data on all patients referred for investigation of anaphylaxis to the pediatric department of the University Hospital Gasthuisberg Leuven and to two private pediatric practices. Data were stored in a MYSQL database by use of an online encrypted web form. Sixty-four cases of anaphylaxis occurred in 48 children, aged 6 months to 14.8 years. Twenty-seven episodes (42.2%) occurred at home. The symptoms were dermatologic in 62 (96.9%) episodes, respiratory in 57 (89.1%), gastrointestinal in 19 (29.7%), cardiovascular in 14 (21.8%), and neurological or behavioural in 19 (29.7%). Antihistamines were administered in 41/57 (71.9%) cases, corticosteroids in 26/57 (45.6%), beta-2-mimetics in 14/57 (24.6%), and adrenaline in 11/57 (19.3%). Out of nine cases where Epipen was available at the moment of anaphylaxis, it was administered in one case only. Food was the cause of anaphylaxis in 42/55 (76.4%) cases with identified trigger, while medication, insect stings, latex, and birch pollen triggered 5 (9.1%), 4 (7.3%), 3 (5.5%), and 1 (1.8%) case(s), respectively. Allergy to the trigger was known prior to anaphylaxis in 19/55 (34.5%) cases. In conclusion, anaphylaxis in pediatric patients generally presents with dermatologic and respiratory symptoms, while in 1/5 episodes cardiovascular symptoms occur. Food is by far the most frequent trigger. Allergy to the trigger is known in 1/3 cases only. Anaphylaxis is under-treated, even when appropriate medication is available.
Similar content being viewed by others
Introduction
Anaphylaxis is a “serious allergic reaction that is rapid in onset and may cause death” [27]. Although data on the incidence and prevalence of anaphylaxis are sparse and often imprecise, its frequency is estimated at a life-time prevalence of 0.05–0.2% [2, 10, 15]. The largest number of new cases occurs among children and adolescents [15]. Anaphylaxis often is under-diagnosed and under-treated [12, 15, 17], which in some cases may result in a fatal course [1, 26]. Recognition of anaphylactic patterns and knowledge of possible anaphylactic triggers may contribute to a more accurate treatment of anaphylactic episodes [29].
In this study we sought to investigate the frequency of anaphylaxis in a pediatric population seen at a tertiary or a secondary referral level, the demographic characteristics of the patients, the clinical course and triggers of anaphylaxis, its therapeutic approach and the co-existence of allergic symptoms and asthma.
Materials and methods
Definition of anaphylaxis and severity grading
At the moment this study started there was no unique internationally accepted definition of anaphylaxis. We define anaphylaxis here as “a serious allergic reaction with rapid onset of symptoms occurring on a site that is remote from the contact site of the trigger and/or in at least two organ systems” [4]. Applying this definition, we meet the clinical criteria for the diagnosis of anaphylaxis as proposed in the position paper of the European Academy for Allergology and Clinical Immunology [19]. According to the guidelines presented in this paper, we discerned mild, moderate, and severe anaphylaxis.
Collecting of data
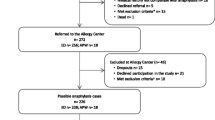
From May 1st 2004 until April 30th 2006 we prospectively collected data on all consecutive patients who were seen for investigation of anaphylaxis at the pediatric department’s outpatient Allergy Clinic of the University Hospital Gasthuisberg Leuven, in a private practice for pediatric allergy situated in Mechelen, or in a private pediatric practice in Hasselt; these facilities will be henceforth referred to as PedAllUH, PedAllPM, and PedPH, respectively. All patients were seen by a pediatrician trained in pediatric allergy (LDS, DB, and MR at PedAllUH; LDS and AD at PedAllPM; MR at PedPH) who handled history taking, clinical examination, and planning of further examinations. Data were stored in a MYSQL database by use of an online encrypted web form written in PHP, which was filled in for each episode of anaphylaxis. The form asked for (1) demographic data; (2) detailed information on the symptoms of anaphylaxis, with separate questions for dermatologic, respiratory, gastrointestinal, cardiovascular, and behavioural or neurological symptoms; (3) the trigger of anaphylaxis, investigations used to confirm the implication of the trigger and previously known allergy to the trigger; (4) the course of anaphylaxis: time lapse between contact with the trigger and onset of subsequent symptoms, total duration of symptoms, biphasic course or not; (5) the treatment of anaphylaxis and time lapse between onset of symptoms and administration of medication; (6) recurrence of anaphylaxis and presence of a management plan for it; and (7) coexistence of allergic and/or asthmatic symptoms.
Identification of the trigger
The trigger of anaphylaxis could be scored as “identified” or “unknown or unclear”. This scoring was left to the interpretation of the individual investigator as a result of careful history taking, with confirmation by skin prick testing (SPT), measurement of allergen-specific IgE serum levels, or by means of provocation testing when this was judged to be appropriate and ethically acceptable [29].
SPT, specific IgE, provocation
Depending on each individual case, SPTs were performed with one or more of the following: (1) a commercial extract of cow’s milk, egg white, peanut, hazelnut, wheat, codfish, latex, and/or birch pollen (HAL, The Netherlands); (2) yellow jacket wasp or honey bee venom extract (ALK-Abellò, Hørsholm,Denmark) in a concentration up to 1.0 μg/ml; (3) self-prepared serial dilutions of methylprednisolon and amoxicillin; and (4) fresh food (apple, kiwi, scampi, lupine, walnut, pistachio, Brazil nut) by means of prick-to-prick testing [7]. SPTs were carried out on the back or on the volar side of the forearm by means of a microlance (HAL prick-lancette) and read after 15 min [22]. Histamine diphosphate 1 mg/ml (HAL) and Coca solution in 50% glycerol were used as positive and negative controls, respectively. Allergen-specific IgE levels were measured using the CAP-system (Phadia, Uppsala, Sweden).
In case food provocation testing was judged to be appropriate, open provocation testing was provided for children below the age of 3 and double-blind-placebo-controlled provocation for children 3 years and older [20].
Statistical analysis
Comparison between groups was done by chi-square, Fisher’s exact, and Mann-Whitney U tests, with two-tailed significance testing.
Results
Demographic data and place of occurrence
We registered 64 cases of anaphylaxis which occurred in 48 children: 31 boys and 17 girls (Table 1). In 58 cases the patient was referred to us after anaphylaxis for further investigation and management, while in only six cases we saw the patient at the moment of anaphylaxis. Twenty patients were seen at PedAllUH for a total of 25 episodes; 28 patients were seen in private practice, 25 of them at PedAllPM and 3 at PedPH, for a total of 36 and 3 episodes, respectively. These figures represent a frequency of 25:2000 ambulant visits at PedAllUH and of 36:2100 and 3:6000 at PedAllPM and at PEDPH, respectively. Age at anaphylaxis ranged from 6 months to 14.8 years, with a mean and median of 6.9 years (Fig. 1). Twenty-seven (42.2%) episodes of anaphylaxis occurred at home, ten episodes (15.6%) took place at the home of family, friends, or neighbours, while anaphylaxis occurring at school, outside, in a restaurant, or in a hospital accounted for 8 (12.5%), 12 (18.7%), 4 (6.2%), and 3 episodes (4.7%), respectively (Fig. 1). In children aged 0–11 years anaphylaxis occurred outside in 6 out of 51 episodes, compared to 6 out of 13 episodes in the adolescent group aged 12–14 years (p < 0.01).
Symptoms
The symptoms occurring during anaphylaxis were dermatologic in 62 episodes (96.9%), respiratory in 57 (89.1%), gastrointestinal in 19 (29.7%), and cardiovascular in 14 (21.8%), while neurological symptoms or changes in behaviour occurred in 19 (29.7%) cases (Table 2). Most patients showed a combination of symptoms. According to the above-mentioned severity grading, 9 (14.1%) of the anaphylactic episodes were classified as mild, 41 (64.1%) as moderate, and 14 (21.8%) as severe. In 57 cases the sequence of symptoms could be noticed, with dermatological and/or respiratory symptoms appearing first in 65% and 42% of cases, respectively.
Trigger
The anaphylactic trigger could be identified in 55 cases (86%), whereas it was unknown or unclear in 9 cases (14%) (Table 1). Out of the nine cases with an unidentified trigger, six had an onset of symptoms within minutes after the ingestion of food, but the ingredients of the ingested food could not be fully identified. Those six cases were considered to be caused by an unidentified food trigger. Taking together the 55 cases with an identified trigger and the six cases with an unidentified food trigger, food was the cause of anaphylaxis in 48 cases (75%), whereas medication, insect stings, latex, and birch pollen were responsible for 5 (9.1%), 4 (7.3%), 3 (5.5%), and 1 (1.8%) case(s), respectively (Fig. 2a). Out of a total of 48 food-induced cases, peanut was the trigger in 12, egg and nuts in seven cases each, cow’s milk in four, kiwi in three, apple in two, and wheat, lupine, fish, and shellfish in one case each. Food additives triggered three cases, and in six cases the food trigger could not be identified (Fig. 2b).
In 5 out of 48 food-induced cases, exercise most likely contributed to the occurrence of anaphylaxis. This was the case in four episodes in the same patient, three of them being caused by peanut and one by an unidentified food trigger; the fifth case occurred in another patient after the ingestion of an additive containing sweets. Furthermore, exercise was a possible contribution to an episode of anaphylaxis caused by exposure to birch pollen.
Episodes of anaphylaxis triggered by medication were due to oral acetylsalicylic acid in two cases, methylprednisolon + amoxicilline–clavulanic acid intravenously in one, methylprednisolon intravenously in one, and benzoic acid in a syrup in one case. The two cases of anaphylaxis due to methylprednisolon and to methylprednisolon + amoxicilline–clavulanic acid intravenously occurred in the same patient while hospitalized in a peripheral pediatric service (methylprednisolon was administered for the purpose of protecting against allergic reaction to antibiotics in this child known to have a complex food allergy and having already experienced two anaphylactic episodes due to food). Benzoic acid was identified as the anaphylactic trigger in a patient previously known to have urticaria due to benzoic acid, but not having previously experienced anaphylaxis to it.
Tests used to confirm the involvement of a specific trigger are shown in Table 3. In two cases a food provocation test was performed, because the food that triggered anaphylaxis contained two different allergens that both tested positive in SPT and CAP.
Previously known allergy to the trigger
Out of 55 cases with an identified trigger, allergy to the anaphylactic trigger had been documented prior to the moment of anaphylaxis in 19 (34.5%) cases (Table 4). This concerned a food allergen in 17 cases. In 14/17 (82%) food-induced cases, the subject and/or parents were unaware of the presence of the causal allergen in the ingested food; the other three cases were triggered by ingestion of raw egg in a subject previously known with egg allergy but having become tolerant to cooked egg in the meantime in one case, by skin contact with raw egg in another case, while the third one was triggered by apple in a patient formerly known with oral allergy syndrome to apple, but not having experienced anaphylactic symptoms to apple before.
On the other hand, out of 36 cases caused by a previously unknown trigger, a food allergen was implicated in 25 (69%) cases: nuts and peanuts in seven and six cases, respectively, kiwi in three, additives in three, and egg, cow’s milk, apple, lupine, fish, and scampi in one case each, respectively.
Course of anaphylaxis
The course of anaphylaxis could be seen in a detailed manner in 54 cases. Time lapse between contact with the trigger and onset of symptoms ranged from a few seconds to 240 min (median 10 min; mean 21 min) (Table 1). In case number 48, which occurred after 2 doses of a benzoic acid containing syrup, time lapse was 240 minutes from the first dose and 25 minutes from the second dose. In 17 children younger than 3 years, time lapse ranged from a few seconds to 90 min (median 2 min; mean 13.2 min), compared to a range from a few seconds to 240 min (median 15 min; mean 25) in 37 children older than 3 years (not significant). The total duration from onset of symptoms until complete recovery ranged from 20 min to 120 hours.
A biphasic course was noticed in two cases, with a symptom-free interval of 4 h and 30 min, respectively.
Treatment
Medication
The medication used to treat anaphylaxis could be identified in 57/64 cases. It concerned antihistamines in 41 (72%), corticosteroids in 26 (46%), beta-2-mimetics in 14 (25%), adrenaline in 11 cases (19%), and paracetamol in one case, while in three cases no medication was used (Fig. 3a). In most cases several medications were used and in several cases one compound was administered in different ways (Fig. 3b). The first medication administered was an antihistamine in 27 (47.4%), cortisone in 14 (24.6%), beta-2-mimetics in 6 (10.5%), adrenaline in 6 (10.5%), and paracetamol in 1 case(s). Adrenaline was administered in 7 out of 14 (50%) severe cases of anaphylaxis and in 4 out of 41 (9.8%) moderately severe cases. In 4 of 11 cases where adrenaline was used, two or more doses were administered.
Other treatment
In 57 out of 64 (89%) episodes of anaphylaxis, the subject was treated in an ambulant way or kept under monitoring for less than 24 hours. In 4 of 64 (6.3%) cases the subject was hospitalised for treatment and monitoring for more than 24 hours; of these cases, one subject needed intubation and assisted ventilation for 4 days. Finally, three cases of anaphylaxis (4.7%) occurred in an already hospitalized subject.
Time lapse between onset of symptoms and administration of medication
Time lapse between onset of symptoms and first administration of medication was recorded in 38 out of 64 episodes, which ranged from 1 to 210 min (mean 30, median 7.5). In 13 of 14 cases with severe anaphylaxis this time lapse ranged from 1 to 30 min (mean 9.69, median 5), while in 24 of 41 cases with moderately severe anaphylaxis it ranged from 1 to 210 min (mean 52, median 30; p < 0.05).
Recurrence of anaphylaxis and presence of a management plan
Eight out of 48 patients (16.6%) experienced two or more episodes of anaphylaxis for a total number of 24 episodes in those eight patients. The total number of episodes per patient and the anaphylactic triggers are given in Table 5. In those patients anaphylaxis was caused by a formerly unknown trigger in 12 cases, by accidental contact with a known trigger in seven cases, and by an unidentified trigger in five cases.
Out of 19 cases caused by a previously known trigger, a management plan for treatment of anaphylaxis–including Epipen–had been handed out prior to the actual episode in 12 cases (Table 4). In 9 of 12 cases Epipen was available at the moment of anaphylaxis, while it was used during the actual anaphylactic episode in one case only; in two other cases Epipen was not administered at the location where anaphylaxis occurred, but the patient received adrenaline subsequently after arrival in the hospital.
Coexisting allergy and/or asthma
Out of 48 patients 32 (66.7%) had a history of atopic disease, 29 of whom having a previously documented sensitization to one or more allergens. The trigger of anaphylaxis in patients with known atopy as compared to patients not known with atopy is depicted in Table 6. Out of 48 patients, 22 (45.8%) were known to have asthma, in whom 33 episodes of anaphylaxis occurred, compared to 31 episodes in 26 patients without asthma. The frequency of moderate and severe anaphylaxis in subjects with asthma was 19/33 (57.6%) and 9/33 (27.3%), respectively, compared to 21/31 (67.7%) and 5/31 (16.1%) in subjects without asthma (not significant). At the moment of anaphylaxis the subjects’ asthma was considered to be well controlled in 18/33 cases (54.5%) and as not controlled in 6/33 (18.2%), whereas the level of control of asthma was not clear in the remaining 9/33 (27.3%) cases.
Discussion
This is the first prospective study on anaphylaxis in children in Belgium. As far as we know, this is also the first survey on anaphylaxis that has been completed using an online database. Doing so allowed us to store detailed information on each individual episode of anaphylaxis at any moment and at any location where the patient was seen.
The number of anaphylactic episodes was highest in the age group 0–3 years, which is comparable with the findings of other authors [3, 6, 9]. This is also concordant with food allergy being the most prevalent in young children and food being the most frequent trigger of anaphylaxis in children [15, 17, 21, 31]. The latter might also explain the gradually lowering figures in subsequent age classes in our patient group. The relatively higher frequency of anaphylaxis in the age group 12–15 years is concordant with the findings of other authors [15] and might at least be partly explained by adolescents being less adherent to preventive measures [1].
Comparable with the findings of other authors, the children’s home was the most frequent location of occurrence of anaphylaxis [17, 21]. However, in the age group 3–6 years a comparable number of episodes occurred at home, school, home of family, friends or neighbours, and outside. This probably reflects the daily schedule of children of this age in the population studied. Fifty percent of anaphylactic episodes in the adolescent group occurring outside compares to data from other authors [1] and can be partly explained by food associated exercise induced anaphylaxis occurring more frequently in this age group. Indeed, out of five cases of food associated exercise induced anaphylaxis, four of them occurred at age 13–14 years, while the fifth occurred at age 4 years. This also stresses the importance of having the management plan and rescue medication available for anaphylaxis at any place and during any activity.
Frequencies of dermatologic, respiratory, gastrointestinal, and cardiovascular symptoms found in this study are comparable with the findings of another referral centre for pediatric allergy [21]. Similarly, we also found dermatologic and respiratory symptoms appearing most frequently as a first symptom. Twenty-two percent of anaphylactic reactions presenting with cardiovascular symptoms is comparable with the findings of a German questionnaire-based study [17]. The only near-fatal case in our survey was triggered by the ingestion of two hazelnuts. As our study concerned patients referred for investigation of anaphylaxis and as in only six cases the patient was seen at the moment of anaphylaxis, our survey clearly cannot be used for calculation of the frequency of fatal cases.
Food was by far the most frequent anaphylactic trigger in the total group, as was also true in all different age classes. In the age group 12–14 years food was even the only trigger. Peanut is the most important trigger, accounting for more than 20% of the cases with an identified trigger and for 25% of those triggered by food, followed by nuts and egg, each accounting for 12.5% of cases with identified triggers. This is in accordance with other investigations in children [17]. As in an earlier although retrospective study in our own pediatric population, cow’s milk was the cause of anaphylaxis in 11/39 cases compared to 6/39 for peanut, this might suggest that the relative importance of cow’s milk and peanut as an anaphylactic trigger has changed in recent years [5]. In contrast to the findings of an Italian survey [21], in our survey only two cases were triggered by fish/shellfish. This distribution of food triggers might reflect different eating habits in different countries [25, 31]. In contrast to other surveys [17, 21], there were no cases triggered by immunotherapy, although immunotherapy currently is prescribed at PedAllUH as well as at PedAllPM and PedPH. Anaphylaxis triggered by insect stings only appearing in the age groups 3–6 and 6–9 years and not in the older age groups probably reflects a local referral policy. Indeed, as in our university hospital rush immunotherapy for severe insect venom allergy is carried out at the department of internal medicine [11], older children and adolescents with insect venom anaphylaxis currently are directly referred to that department.
Anaphylaxis caused by a previously identified trigger occurred most frequently in connection with peanut and egg. In 14 out of 17 (82%) episodes caused by an already known food trigger, the patients/parents were unaware of its presence in the ingested food. This stresses the importance of clear food labelling and of extensive dietetic information [30]. On the other hand, for 6/12 patients with peanut anaphylaxis and for all seven patients with nut anaphylaxis, the actual episode was the first manifestation of peanut/nut allergy. Moreover, four of seven patients with nut anaphylaxis weren’t even aware of any allergy at all. However, by means of careful history taking it was revealed that some of these patients had shown mild, but so far unnoticed signs that might have been preliminary symptoms of the actual food allergy (data not shown). The three episodes of anaphylaxis caused by ingestion of kiwi were also the first manifestation of kiwi allergy in the respective three patients. Thus, although features predictive of a serious allergic reaction to food have been identified, such features are lacking in a substantial proportion of cases [24, 29]. It will be a task for future studies and for pediatric allergists to further disclose the early signs of allergy that are predictive of a potentially serious reaction to the most frequent causal allergens of anaphylaxis.
As expected, an IgE-dependent mechanism could be confirmed in the majority of cases with identified trigger [28]. However, an IgE-independent, so-called pseudoallergic mechanism presumably was involved in two and one case(s) triggered by acetylsalicylic acid and by benzoic acid, respectively [23], while for three cases caused by food additives the underlying mechanism could not be documented.
Time lapse between contact with the trigger and onset of symptoms is comparable with other data on anaphylaxis in children and adolescents [2, 21]. In contrast to the findings of another referral centre for pediatric allergy [21], we found the latency period in children aged 0–3 years shorter than in older ones. The same applied to children aged 0–2 years as compared to older ones (data not shown). The only two biphasic reactions in our study were triggered by peanut and bee venom respectively. The low frequency of biphasic reactions we noticed is in contrast to the findings of other studies [8, 14], but comparable with the findings of one pediatric study [13]. As other surveys on anaphylaxis in children currently do not mention biphasic anaphylaxis [6, 17, 21], this might suggest that biphasic anaphylaxis is less frequent in children than in adults. On the other hand, one can speculate that the administration of corticosteroids might have protected some patients from a biphasic course, although clear-cut documentation for such a protection is not available [14, 16].
The most frequently used medication to treat anaphylaxis was antihistamines, which is comparable with the findings of other surveys [15, 17]. As adrenaline was administered in only 50% of cases with cardiovascular symptoms and in only 10.5% of moderately severe cases, it must be stressed that anaphylaxis clearly was under-treated. This is concordant with previous appraisals on the management of anaphylaxis [12, 15, 17]. Moreover, although nine patients had Epipen available at the actual episode, this was used in only one case, while—according to the severity of the episode—its use was indicated in seven cases. Nevertheless, all parents had been extensively instructed on how to use Epipen. This suggests that parents and patients follow the instructions as to carry a management plan and Epipen with them, but are reluctant to use the pen when necessary. It also indicates that repeated training of parents and patients in the management of anaphylaxis is necessary.
The frequency of recurrence of anaphylaxis is in accordance with other investigations [18]. However, it must be stressed that two patients having experienced four and five cases of anaphylaxis, respectively, had not received preventive measures before, nor an adrenaline based management plan. Follow-up of our patients has to show if such measures are successful in decreasing the frequency of recurrence.
Although severe anaphylaxis was more frequent in patients with asthma as compared to patients without asthma, this difference was not statistically significant.
Conclusion
Anaphylaxis in children occurs most frequently at home, except in adolescents who experience 50% of their anaphylactic episodes outside. Food is the trigger of anaphylaxis in 75% of cases, with peanut counting for 25% of all food induced episodes and egg and nuts each for 12.5%. Most patients have dermatological and respiratory symptoms, while gastrointestinal and cardiovascular symptoms occur in 30% and 22%, respectively. Anaphylaxis clearly is under-treated, even when appropriate medication is available. In only one of three cases, allergy to the trigger is known prior to anaphylaxis.
Abbreviations
- SPT:
-
skin prick test
References
Bock SA, Munoz-Furlong A, Sampson HA (2001) Fatalities due to anaphylactic reactions to foods. J Allergy Clin Immunol 107:191–193
Bohlke K, Davis RL, DeStefano F, Marcy SM, Braun MM, Thompson RS (2004) Epidemiology and anaphylaxis among children and adolescents enrolled in a health maintenance organisation. J Allergy Clin Immunol 113:536–542
Boros CA, Kay D, Gold MS (2000) Parent reported allergy and anaphylaxis in 4173 South Australian children. J Paediatric Child Health 36:36–40
Ceuppens JL (2005) Anafylaxie en veralgemeende vormen van acute allergische reacties: een overzicht. Tijdschr voor Geneeskunde 61:1142–1149
De Swert LF (2005) Anafylaxie bij kinderen. Tijdschr voor Geneeskunde 61:1150–1154
Dibs SD, Baker MD (1997) Anaphylaxis in children: a 5-year experience. Pediatrics 99(1):E7
Dreborg S, Foucard T (1983) Allergy to apple, carrot and potato in children with birch pollen allergy. Allergy 38:167–172
Ellis AK, Day JH (2007) Incidence and characteristics of biphasic anaphylaxis: a prospective evaluation of 103 patients. Ann Allergy Asthma Immunol 98:64–69
Gupta R, Sheikh A, Strachan P, Anderson HR (2004) Burden of allergic disease in the UK: secondary analyses of national databases. Clin Exp Allergy 34:520–526
Hebling A, Hurni T, Mueller UR, Pichler WJ (2004) Incidence of anaphylaxis with circulatory symptoms: a study over a 3-year period comprising 940,000 inhabitants of the Swiss Canton Bern. Clin Exp Allergy 34:285–290
Kochuyt AM, Van Hoeyveld EM, Stevens EA (2005) Prevalence and clinical relevance of specific immunoglobulin E to pollen caused by sting-induced specific immunoglobulin E to cross-reacting carbohydrate determinants in Hymenoptera venoms. Clin Exp Allergy 35:441–447
Krugman SD, Chiaramonte DR, Matsui EC (2006) Diagnosis and management of food-induced anaphylaxis: a national survey of pediatricians. Pediatrics 118:e554–e560
Lee JM, Greenes DS (2000) Biphasic anaphylactic reactions in pediatrics. Pediatrics 106:762–766
Lieberman P (2005) Biphasic anaphylactic reactions. Ann Allergy Asthma Immunol 95:217–226
Lieberman P, Camargo CA, Bohlke K, Jick H, Miller RL, Sheikh A, Simons FE (2006) Epidemiology of anaphylaxis: findings of the American College of Allergy, Asthma and Immunology Epidemiology of anaphylaxis working group. Ann Allergy Asthma Immunol 97:596–602
Lieberman P, Decker W, Camargo CA, O’Connor R, Oppenheimer J, Simons FE (2007) SAFE: a multidisciplinary approach to anaphylaxis education in the emergency department. Ann Allergy Asthma Immunol 98:519–523
Mehl A, Wahn U, Niggeman B (2005) Anaphylactic reactions in children—a questionnaire-based survey in Germany. Allergy 60:1440–1445
Mullins RJ (2003) Anaphylaxis: risk factors for recurrence. Clin Exp Allergy 33:1033–1040
Muraro A, Roberts G, Clark A, Eigenmann PA, Halken S, Lack G, Moneret-Vautrin M, Niggeman B, Rancé F; EAACI task force on anaphylaxis in children (2007) The management of anaphylaxis in childhood: position paper of the European academy of allergology and clinical immunology. Allergy 62:857–871
Muraro MA (2001) Diagnosis of food allergy: the oral provocation test. Pediatr Allergy Immunol 12(suppl 14):31–36
Novembre E, Cianferoni A, Bernardini R, Mugnaini L, Caffarelli C, Cavagni G, Giovane A, Vierucci A (1998) Anaphylaxis in children: clinical and allergologic features. Pediatrics Apr 101(4):E8
Osterballe O, Weeke B (1979) A new lancet for skin prick testing. Acta Paediatrica Scandinavica 34:209–212
Pichler WJ (2007) Drug hypersensitivity reactions: classification and relationship to T-cell activation. In: Pichler WJ (ed) Drug hypersensitivity. Karger, Basel pp169–189
Pumphrey R (2004) Anaphylaxis: can we tell who is at risk of a fatal reaction? Curr Opin Allergy Clin Immunol 4:285–290
Sampson HA (2004) Update on food allergy. J Allergy Clin Immunol 113:805–819
Sampson HA, Mendelson L, Rosen JP (1992) Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Eng J Med 327:380–384
Sampson HA, Munoz-Furlong A, Campbell RL, Adkinson F Jr, Bock A, Branum A, Brown SG, Camargo CA Jr, Cydulka R, Galli SJ, Gidudu J, Gruchalla RS, Harlor AD Jr, Hepner DL, Lewis LM, Lieberman PL, Metcalfe DD, O’Connor R, Muraro A, Rudman A, Schmitt C, Scherrer D, Simons FE, Thomas S, Wood JP, Decker WW (2006) Second symposium on the definition and management of anaphylaxis: summary report. J Allergy Clin Immunol 117:391–397
Simons FE (2006) Anaphylaxis, killer allergy: long-term management in the community. J Allergy Clin Immunol 367–377
Simons FE, Frew AJ, Ansotegui IJ, Bochner BS, Golden DB, Finkelman FD, Leung DY, Lotvall J, Marone G, Metcalfe DD, Müller U, Rosenwasser LJ, Sampson HA, Schwartz LB, van Hage M, Walls AF (2007) Risk assessment in anaphylaxis: current and future approaches. J Allergy Clin Immunol 120:S2–S24
Taylor SL, Hefle SL (2006) Food allergen labelling in the USA and Europe. Curr Opin Allergy Clin Immunol 6:186–190
Wood RA (2003) The natural history of food allergy. Pediatrics 111:1631–1633
Acknowledgements
We would like to thank Johannes Daniels for statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work has been partially sponsored by an unrestricted grant from UCB, Belgium.
Rights and permissions
About this article
Cite this article
De Swert, L.F.A., Bullens, D., Raes, M. et al. Anaphylaxis in referred pediatric patients: demographic and clinical features, triggers, and therapeutic approach. Eur J Pediatr 167, 1251–1261 (2008). https://doi.org/10.1007/s00431-007-0661-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-007-0661-2