Abstract
Pulmonary Langerhans cell histiocytosis (PLCH) is a rare, smoking-related histiocytic disorder with variable clinical symptoms. Like in other non-pulmonary Langerhans cell proliferations, PLCH has recently been shown to harbour BRAF V600E mutations in a significant subset of cases, thus challenging the concept of PLCH being a reactive disorder. Here, we analysed 38 formalin-fixed and paraffin-embedded PLCH nodules of nine patients for BRAF mutation using two different molecular methods. Using pyrosequencing and allele-specific quantitative PCR (AS-PCR), BRAF V600E mutations were found in 16/38 (42%) and 31/37 (84%) nodules, respectively. Analysing different nodules of the same patients with pyrosequencing 3/6 patients showed a concordant BRAF mutation status. When allele-specific quantitative PCR was used, condordant results were found in 5/6 patients. Our findings clearly indicate that (a) the sensitivity of the method used is crucial in analysing BRAF mutation status, (b) AS-PCR is more sensitive in detecting BRAF V600E mutations than pyrosequencing, (c) BRAF mutation is frequent and might play a key role in the pathogenesis of PLCH and (d) PLCH is a true neoplastic disease.
Similar content being viewed by others
Introduction
Langerhans cells represent a specific type of antigen presenting cells located in the skin and beneath the epithelium of the tracheobronchial tree [1]. Tumours with Langerhans cell differentiation can occur in multisystemic or localized forms [2, 3]. Pulmonary Langerhans cell histiocytosis (PLCH) belongs to the localized type and shows multiple pulmonary nodular infiltrations usually between 1 and 20 mm in size. It is a rare disorder and occurs predominantly in adult smokers [4–7]. In the lung, smoking induces Langerhans cell accumulation and activation, pointing to a reactive nature of PLCH [1]. Although early studies found evidence for a clonal proliferation of systemic Langerhans cell histiocytosis in children [8, 9], the vast majority of PLCH were found to be polyclonal thus supporting the concept of PLCH being a non-neoplastic lesion [10].
A member of Raf protein kinase family BRAF plays a key role in the regulation of the MAP Kinase/ERK signalling pathway and influences cell proliferation, cell differentiation and apoptosis [11–13]. BRAF gene mutations have been described in a number of malignant tumours such as melanoma, papillary thyroid carcinoma, colorectal and lung adenocarcinoma and hairy cell leukaemia. A number of different mutations have been reported. But more than 90% of mutations affect codon 600 leading to gene activation by substitution of valine by glutamate (V600E mutation) [14, 15]. Inhibition of BRAF by vemurafenib or dabrafenib is now an accepted therapeutic approach of selected malignant tumours with activating BRAF mutation [16].
BRAF V600E mutations have also been reported in up to 60% of patients with non-pulmonary Langerhans cell histiocytosis [17–20]. Treatment of some of these cases with BRAF inhibitor vemurafenib might be a promising therapeutic approach [18, 21, 22]. Finally, few studies reported also on BRAF mutations in adult cases of PLCH, giving new insight into the pathogenesis of the special entity and challenging the concept of PLCH being a reactive disorder [23–27].
To contribute to a better understanding of PLCH, we aimed to analyse the BRAF mutation status in our collection of cases using two different molecular methods. Furthermore, we aimed to analyse the possible concordance and discordance of BRAF mutations in different PLCH nodules of the same patient.
Material and methods
Tissue and antibodies
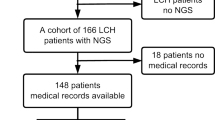
In the archive of our institute, tissue blocks of 11 lung resections from nine patients containing 38 nodules with PLCH were identified between the years 2006 and 2014. The size of the nodules ranged from 0.1 to 0.8 cm. The patients’ characteristics are summarized in Table 1.
Approval for the analysis conducted in this study was received from the ethics committee at the Albert-Ludwigs-University of Freiburg (approval no. 10005-16).
All formalin-fixed and paraffin-embedded PLCH specimens were histologically re-evaluated in H&E stained sections according to routine protocols.
Additional immunohistochemistry was performed using antibodies against protein S-100 (diluted 1:250, DCS, Germany) and CD1a (diluted 1:20, Novocastra, UK) to proof Langerhans cell differentiation. For CD1a, antigen retrieval sections were incubated for 30 min in a heat steamer with citrate buffer pH 6.0. No antigen retrieval protocol was used for S-100 detection. After applying primary antibodies, S100 and CD1a biotinylated secondary goat antibodies (Polylink DetectionLine, DCS, Hamburg, Germany) were added. Colour was developed using DAB (DCS, Hamburg, Germany). Immunostaining was carried out by an OptiMax 2.0 Immunostainer (Biogenex, CA). Non-tumour tissue on the slide was used as internal control.
Pyrosequencing
Tumour areas marked by an experienced pathologist on haematoxylin-eosin stained slides were microdissected on corresponding deparaffinized and hydrated slide samples and tumour tissue was collected in a microtube. After adding 180 μl Higuchi buffer and 20 μl proteinase K, samples were incubated overnight at 56 °C and finally denatured at 94 °C for 10 min.
BRAF mutation analysis by pyrosequencing was performed as previously described [28]. Briefly, for BRAF exon15 analysis, 5 μl of tissue lysate was added to PCR mixture containing dNTPs (each 200 μM), 1.5 mM MgCl2, 50 mM KCl, 30 mM Tris-HCl, 0.2% Igepal®-CA630, Taq polymerase (1.25 units; 5Prime, Hamburg, Germany), forward and reverse primers (400 nM each, see Table 2) and water to a final volume of 50 μl. PCR was conducted using following temperatures: 4 min at 95 °C, 35 cycles 30 s at 95 °C, 30 s at 60 °C and 30 s at 72 °C followed by 7 min at 72 °C. BRAF amplicon size was 92 bp. Six to twenty microliters of PCR products was purified and denatured in vacuum preparation procedure using streptavidin-coupled sepharose beads as described in manufacturer’s protocol for Pyromark Q24 (Qiagen, Hilden, Germany). Pyrosequencing was performed using corresponding sequencing primers (500 nM each) and dispensation order (see Table 2). The accuracy of the applied pyrosequencing method was externally validated and proofed by repeated and successful participation in the respective round robin test performed by the German Society of Pathology. For our pyrosequencing assay, limit of blank (LoB) was calculated from blank measurements according to a standard method recently published by Clinical and Laboratory Standards Institute (CLSI document EP17) [29] as LoB = mean wild type + 1.645 × standard deviation of wild type (SDwild type) = 5.64%. As recommended by manufacturer of pyrosequencing instrument, limit of detection (LoD) was set to LoD = LoB +3 × SDwild type = 10.74%, leading to confidence interval of 99.7% in discrimination between wild type and mutated samples.
Allele-specific quantitative PCR
BRAF exon15 V600E mutation analysis was performed using allele-specific quantitative PCR as previously published [30]. In brief, two quantitative PCR reactions were necessary to calculate allele frequencies. At first reference, PCR was performed in a 25 μl reaction volume containing 1× PCR Master Mix (Peqlab, Erlangen, Germany), 6 mM MgCl2, 900 nM each BRAF mutation-unspecific forward and reverse primer, 100 nM BRAF probe, 112.5 nM each internal control forward and reverse primer, 25 nM internal control probe (see Table 3) and 5 μl of DNA lysate prepared as described above. Subsequently, V600E allele-specific PCR was performed according to the same protocol but using a concentration of 450 nM allele-specific primer. All reactions were performed on LightCycler Nano Real-Time PCR System (Roche Diagnostics, Vienna, Austria) with this temperature profile: 95 °C for 10 min, followed by 50 cycles of 90 °C for 15 s and 60 °C for 1 min. All reactions were performed in duplicate and only samples with two detectable Ct values were regarded as true positives. Cycle threshold (Ct) values were recorded for reference PCR and for AS-PCR and calculation of their differences provided corresponding ΔCt values. Standard curves to calculate allele frequencies of samples were generated by dilution series of DNA with known allele frequencies and detection limit was defined at the previously published threshold ΔCt of 9 resulting in sensitivity limit of 0.1% allele frequency.
Results
All nodules of PLCH showed typical morphology and were positive for S100 and CD1a. The proportion of Langerhans cells in each nodule ranged between 20 and 70%. A typical example is shown in Fig. 1.
Using pyrosequencing and the cut-off values as described above BRAF V600E mutations were found in 16/38 (42%) nodules. 22/38 (58%) nodules were BRAF V600E wild type. A typical molecular result (pyrogram) is shown in Fig. 2. In all 13 nodules of 3 patients, no BRAF V600E mutation was detected at all, whereas all 7 nodules of 3 patients were BRAF V600E mutated. The remaining 3 patients showed mutated and non-mutated nodules simultaneously: one had a predominance of mutated nodules (7 mutated vs. 2 non-mutated), one had a predominance of unmutated nodules (6 unmutated vs. 1 mutated) and one patient had equal number of mutated and non-mutated nodules (one each). Histologically, mutated and unmutated nodules showed no significant difference. These results are summarized in Table 1.
Using AS-PCR remarkable differences in the mutation status could be found: In AS-PCR, BRAF V600E mutations were found in 31/37 (84%) nodules whereas 6/37 (16%) nodules were BRAF V600E wild type. A typical amplification plot is shown in Fig. 3.
With AS-PCR in all but one of eight patients with valid results only mutated (23 nodules of six patients) or non-mutated nodules (five of one patient) were detected. Only one patient had discordant results with one unmutated and eight mutated nodules. Due to significant DNA degradation and non-representative residual tissue one nodule (patient-ID 3) could not be investigated by AS-PCR. These results are summarized in Table 1.
Allele frequencies were comparable between both analysis methods. The correlation between the two methods is shown in Fig. 4. BRAF mutations detected in AS-PCR and not by pyrosequencing had an allele frequency below 7%. Differences in percentage between both methods could be assumed to partly degraded samples with low DNA content and prolonged storage.
Histologically, mutated and unmutated nodules showed no significant difference.
Discussion
Pulmonary Langerhans cell histiocytosis is a rare, smoking-related disorder with uncertain pathogenesis. Although earlier studies pointed to a reactive, inflammatory or immunological disorder, recent results on recurrent BRAF V600E mutations indicate a clonal and neoplastic disorder at least in a subset of cases [1, 25].
In this study, we analysed the frequency of BRAF V600E mutation in our cohort of pulmonary Langerhans cell histiocytosis using two different molecular methods, namely pyrosequencing and AS- PCR. Furthermore, we investigated various nodules of PLCH in the same patient to get more insight into the pathogenesis of the disease in two aspects, possible clonality and natural course.
Pyrosequencing and AS-PCR provided molecular results with remarkable differences. Depending on method of detection, BRAF V600E mutations were found in 42 and 84%, respectively.
However, the range of these frequencies is in agreement with the results of other studies. Using molecular methods, the BRAF V600E mutation rate in PLCH was found between 28 and 67% of cases [23, 25, 26, 31]. Using immunohistochemistry, Chilosi et al. found BRAF expression indicating BRAF mutations in 61% of their collection of patients [27].
According to our results, the detection rate of BRAF mutations in PLCH depends on the method used. With pyrosequencing, we found a cut-off value and sensitivity of 10%. Using the more sensitive method of AS-PCR, the cut-off value was 0.1%. These figures correspond well with the recent data of Mourah et al. who also investigated BRAF mutations with two different molecular approaches. The cut-off values for pyrosequencing and ICE-COLD-PCR in their study was 7 and 0.1%, respectively. This explains the fact that in our study and in the paper by Mourah et al. PLCH nodules thought to be BRAF unmutated according to pyrosequencing turn to mutated when more sensitive methods are used [23].
So far, only two studies focused on BRAF mutation status in different PLCH nodules of in the same patient. In the five patients studied by Youssem et al., all 22 nodules showed concordant mutation status. That means if one nodule in a patient was mutated all other nodules of the same patient were also mutated and vice versa. Recently, Kamionek also reported on 18 nodules of seven patients showing concordant BRAF mutation status [25, 31]. This concordance was taken as a sign of clonality of all foci. Furthermore, it was concluded that some cases of PLCH nodules do not need BRAF mutation to proliferate [25].
Our study could mainly confirm these observations described. Six of our patients had more than one nodule studied and five of them showed concordant mutation status in all nodules when the more sensitive AS-PCR was used. However, in one patient with nine nodules eight where mutated and one was unmutated. This discordance could be a matter of method sensitivity as discussed above. Another explanation for the discrepant results might be the low numbers of cases included in these analyses. But studies analysing a higher number of patients did not investigate various nodules in the same patients [26, 27]. Finally, it is also possible that PLCH is not an entire clonal lesion. Mourah et al. provided experimental evidence that in a single lesion various subclones exist which can be both BRAF, mutated and unmutated [23]. Furthermore it is of interest that in a paper published in the year 2001 by Youssem clonal and non-clonal nodules of PLCH were found in the same patient which is contradictory to the more recent results of the same research group [10, 25].
Interestingly, Roden et al. reported that BRAF mutation was associated with higher cumulative tobacco exposure [26]. This could mean that BRAF mutation occurs not as an early but as a later event in the pathogenesis of PCLH. Therefore, it would be of no wonder that mutated and unmutated Langerhans cells and PLCH nodules can occur in the same patient. Our results could support this concept but it still has to be confirmed in future studies.
BRAF V600E is not the only mutation found in PLCH. Recently, gene mutations in other factors in the ERK signalling pathway like MAP2KI, MAP3KI and N-RAS were reported. These results indicate that LCH cells can harbour additional genetic alterations in the RAS-RAF-MEK pathway. In particular, MAP2K1 mutations may be responsible for ERK activation even in a BRAF wild-type setting [23, 31–33]. But these genes were not in the focus of our study.
In summary, we found BRAF V600E mutations in a significant number of PLCH. The detection rate of BRAF mutations clearly depends on the molecular method used. Using sensitive molecular methods, we found a clear predominance of concordant BRAF mutations in multiple nodules of the same patient. Whether the single observation of a discordant BRAF mutation status is pathogenetically relevant needs to be addressed in further studies on this topic with higher numbers of patients and/or nodules. Furthermore, additional studies with an expanded number of genes involved are needed to provide a better understanding of the pathogenesis of this rare disorder.
References
Suri HS, Yi ES, Nowakowski GS, Vassallo R (2012) Pulmonary Langerhans cell histiocytosis. Orphanet J Rare Dis 7:16
El Demellawy D, Young JL, de Nanassy J, Chernetsova E, Nasr A (2015) Langerhans cell histiocytosis: a comprehensive review. Pathology 47:294–301
Grana N (2014) Langerhans cell histiocytosis. Cancer Control 21:328–334
Travis WD, Borok Z, Roum JH, Zhang J, Feuerstein I, Ferrans VJ, Crystal RG (1993) Pulmonary Langerhans cell granulomatosis (histiocytosis X). A clinicopathologic study of 48 cases. Am J Surg Pathol 17:971–986
Tazi A (2006) Adult pulmonary Langerhansʼ cell histiocytosis. Eur Respir J 27:1272–1285
Allen TC (2008) Pulmonary Langerhans cell histiocytosis and other pulmonary histiocytic diseases: a review. Arch Pathol Lab Med 132:1171–1181
Vassallo R, Ryu JH (2004) Pulmonary Langerhansʼ cell histiocytosis. Clin Chest Med 25:561–571 vii
Willman CL, Busque L, Griffith BB, Favara BE, McClain KL, Duncan MH, Gilliland DG (1994) Langerhansʼ-cell histiocytosis (histiocytosis X)—a clonal proliferative disease. N Engl J Med 331:154–160
Yu RC, Chu C, Buluwela L, Chu AC (1994) Clonal proliferation of Langerhans cells in Langerhans cell histiocytosis. Lancet 343:767–768
Yousem SA, Colby TV, Chen YY, Chen WG, Weiss LM (2001) Pulmonary Langerhansʼ cell histiocytosis: molecular analysis of clonality. Am J Surg Pathol 25:630–636
Daum G, Eisenmann-Tappe I, Fries HW, Troppmair J, Rapp UR (1994) The ins and outs of Raf kinases. Trends Biochem Sci 19:474–480
Robinson MJ, Cobb MH (1997) Mitogen-activated protein kinase pathways. Curr Opin Cell Biol 9:180–186
Chong H, Vikis HG, Guan KL (2003) Mechanisms of regulating the Raf kinase family. Cell Signal 15:463–469
Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, Davis N, Dicks E, Ewing R, Floyd Y, Gray K, Hall S, Hawes R, Hughes J, Kosmidou V, Menzies A, Mould C, Parker A, Stevens C, Watt S, Hooper S, Wilson R, Jayatilake H, Gusterson BA, Cooper C, Shipley J, Hargrave D, Pritchard-Jones K, Maitland N, Chenevix-Trench G, Riggins GJ, Bigner DD, Palmieri G, Cossu A, Flanagan A, Nicholson A, Ho JW, Leung SY, Yuen ST, Weber BL, Seigler HF, Darrow TL, Paterson H, Marais R, Marshall CJ, Wooster R, Stratton MR, Futreal PA (2002) Mutations of the BRAF gene in human cancer. Nature 417:949–954
Hall RD, Kudchadkar RR (2014) BRAF mutations: signaling, epidemiology, and clinical experience in multiple malignancies. Cancer Control 21:221–230
Zhang W (2015) BRAF inhibitors: the current and the future. Curr Opin Pharmacol 23:68–73
Badalian-Very G, Vergilio JA, Degar BA, Rodriguez-Galindo C, Rollins BJ (2012) Recent advances in the understanding of Langerhans cell histiocytosis. Br J Haematol 156:163–172
Haroche J, Charlotte F, Arnaud L, von Deimling A, Helias-Rodzewicz Z, Hervier B, Cohen-Aubart F, Launay D, Lesot A, Mokhtari K, Canioni D, Galmiche L, Rose C, Schmalzing M, Croockewit S, Kambouchner M, Copin MC, Fraitag S, Sahm F, Brousse N, Amoura Z, Donadieu J, Emile JF (2012) High prevalence of BRAF V600E mutations in Erdheim-Chester disease but not in other non-Langerhans cell histiocytoses. Blood 120:2700–2703
Sahm F, Capper D, Preusser M, Meyer J, Stenzinger A, Lasitschka F, Berghoff AS, Habel A, Schneider M, Kulozik A, Anagnostopoulos I, Mullauer L, Mechtersheimer G, von Deimling A (2012) BRAFV600E mutant protein is expressed in cells of variable maturation in Langerhans cell histiocytosis. Blood 120:e28–e34
Satoh T, Smith A, Sarde A, Lu HC, Mian S, Trouillet C, Mufti G, Emile JF, Fraternali F, Donadieu J, Geissmann F (2012) B-RAF mutant alleles associated with Langerhans cell histiocytosis, a granulomatous pediatric disease. PLoS One 7:e33891
Haroche J, Cohen-Aubart F, Emile JF, Arnaud L, Maksud P, Charlotte F, Cluzel P, Drier A, Hervier B, Benameur N, Besnard S, Donadieu J, Amoura Z (2013) Dramatic efficacy of vemurafenib in both multisystemic and refractory Erdheim-Chester disease and Langerhans cell histiocytosis harboring the BRAF V600E mutation. Blood 121:1495–1500
Haroche J, Cohen-Aubart F, Emile JF, Donadieu J, Amoura Z (2015) Vemurafenib as first line therapy in BRAF-mutated Langerhans cell histiocytosis. J Am Acad Dermatol 73:e29–e30
Mourah S, How-Kit A, Meignin V, Gossot D, Lorillon G, Bugnet E, Mauger F, Lebbe C, Chevret S, Tost J, Tazi A (2016) Recurrent NRAS mutations in pulmonary Langerhans cell histiocytosis. Eur Respir J 47:1785–1796
Badalian-Very G, Vergilio JA, Degar BA, MacConaill LE, Brandner B, Calicchio ML, Kuo FC, Ligon AH, Stevenson KE, Kehoe SM, Garraway LA, Hahn WC, Meyerson M, Fleming MD, Rollins BJ (2010) Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood 116:1919–1923
Yousem SA, Dacic S, Nikiforov YE, Nikiforova M (2013) Pulmonary Langerhans cell histiocytosis: profiling of multifocal tumors using next-generation sequencing identifies concordant occurrence of BRAF V600E mutations. Chest 143:1679–1684
Roden AC, Hu X, Kip S, Parrilla Castellar ER, Rumilla KM, Vrana JA, Vassallo R, Ryu JH, Yi ES (2014) BRAF V600E expression in Langerhans cell histiocytosis: clinical and immunohistochemical study on 25 pulmonary and 54 extrapulmonary cases. Am J Surg Pathol 38:548–551
Chilosi M, Facchetti F, Calio A, Zamo A, Brunelli M, Martignoni G, Rossi A, Montagna L, Piccoli P, Dubini A, Tironi A, Tomassetti S, Poletti V, Doglioni C (2014) Oncogene-induced senescence distinguishes indolent from aggressive forms of pulmonary and non-pulmonary Langerhans cell histiocytosis. Leuk Lymphoma 55:2620–2626
Dimmler A, Geddert H, Faller G (2014) EGFR, KRAS, BRAF-mutations and microsatellite instability are absent in goblet cell carcinoids of the appendix. Pathol Res Pract 210:274–278
Tholen DW, Linnet K, Kondratovich M, Armbruster DA, Garrett PE, Jones RL, Kroll MH, Lequin RM, Pankratz TJ, Scassellati G (2004) Protocols for determination of limits of detection and limits of quantitation; approved guidelines
Lang AH, Drexel H, Geller-Rhomberg S, Stark N, Winder T, Geiger K, Muendlein A (2011) Optimized allele-specific real-time PCR assays for the detection of common mutations in KRAS and BRAF. J Mol Diagn 13:23–28
Kamionek M, Ahmadi Moghaddam P, Sakhdari A, Kovach AE, Welch M, Meng X, Dresser K, Tomaszewicz K, Dresser K, Cosar EF, Mark EJ, Fraire AE, Hutchinson L (2016) Mutually exclusive ERK pathway mutations are present in different stages of multifocal pulmonary Langerhans cell histiocytosis supporting clonal nature of the disease. Histopathology 69:499–509
Chakraborty R, Hampton OA, Shen X, Simko SJ, Shih A, Abhyankar H, Lim KP, Covington KR, Trevino L, Dewal N, Muzny DM, Doddapaneni H, Hu J, Wang L, Lupo PJ, Hicks MJ, Bonilla DL, Dwyer KC, Berres ML, Poulikakos PI, Merad M, McClain KL, Wheeler DA, Allen CE, Parsons DW (2014) Mutually exclusive recurrent somatic mutations in MAP2K1 and BRAF support a central role for ERK activation in LCH pathogenesis. Blood 124:3007–3015
Nelson DS, van Halteren A, Quispel WT, van den Bos C, Bovee JV, Patel B, Badalian-Very G, van Hummelen P, Ducar M, Lin L, MacConaill LE, Egeler RM, Rollins BJ (2015) MAP2K1 and MAP3K1 mutations in Langerhans cell histiocytosis. Genes Chromosomes Cancer 54:361–368
Acknowledgments
The authors wish to thank Ines Obreiter and Stephanie Lechner for expert technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest. Approval for the analysis conducted in this study was received from the ethics committee at the Albert-Ludwigs-University of Freiburg (approval no. 10005/16).
Rights and permissions
About this article
Cite this article
Dimmler, A., Geddert, H., Werner, M. et al. Molecular analysis of BRAF V600E mutation in multiple nodules of pulmonary Langerhans cell histiocytosis. Virchows Arch 470, 429–435 (2017). https://doi.org/10.1007/s00428-017-2092-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-017-2092-4