Abstract
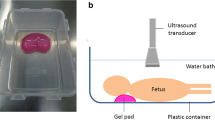
To determine the feasibility of percutaneous fetal organ biopsies in the context of a ‘minimally invasive’ perinatal autopsy after stillbirth and termination for abnormality is the aim of this study. We assessed successful biopsy rate and the proportion adequate for histological examination in 30 fetuses undergoing organ sampling before autopsy. The relationship between gestational age, body weight, death–biopsy interval, operator experience and successful biopsy rate was investigated. Significant findings from conventional block histology were compared with corresponding percutaneous biopsies. Of 210 organ biopsies attempted from seven target organs, 107 were obtained, of which 94 were adequate for pathological comment. The median delivery–autopsy interval was 4 (range 2–11) days. Adequate samples were obtained from the lung in 86% cases (95% CI 68, 96%), liver 76% (95% CI 56, 90%) and less frequently for the myocardium, kidney, adrenal, thymus and spleen. There was no relationship between biopsy success and time to biopsy, gestational age, body weight and user experience. No histological abnormalities found at autopsy were diagnosed from needle biopsies. Although targeted percutaneous biopsies appear feasible for some organs, fewer than 50% of all biopsies are adequate for histological examination. This technique cannot be considered to provide useful clinical information as part of a ‘minimally invasive’ perinatal autopsy.


Similar content being viewed by others
References
Alderliesten ME, Peringa J, van der Hulst VP, Blaauwgeers HL, van Lith JM (2003) Perinatal mortality: clinical value of postmortem magnetic resonance imaging compared with autopsy in routine obstetric practice. BJOG 110:378–382
Boyd PA, Tondi F, Hicks NR, Chamberlain PF (2004) Autopsy after termination of pregnancy for fetal anomaly: retrospective cohort study. BMJ 328:137
Breeze AC, Cross JJ, Hackett GA, Jessop FA, Joubert I, Lomas DJ, Set PA, Whitehead AL, Lees CC (2006) Use of a confidence scale in reporting postmortem fetal magnetic resonance imaging. Ultrasound Obstet Gynecol 28:918–924
Brookes JA, Hall-Craggs MA, Sams VR, Lees WR (1996) Non-invasive perinatal necropsy by magnetic resonance imaging. Lancet 348:1139–1141
Cox P, Scott R (2001) Perinatal pathology in 2001. Arch Dis Child 84:457–458
Farina J, Millana C, Fdez-Acenero MJ, Furio V, Aragoncillo P, Martin VG, Buencuerpo J (2002) Ultrasonographic autopsy (echopsy): a new autopsy technique. Virchows Arch 440:635–639
Foroudi F, Cheung K, Duflou J (1995) A comparison of the needle biopsy post mortem with the conventional autopsy. Pathology 27:79–82
Griffiths PD, Paley MN, Whitby EH (2005) Post-mortem MRI as an adjunct to fetal or neonatal autopsy. Lancet 365:1271–1273
Griffiths PD, Variend D, Evans M, Jones A, Wilkinson ID, Paley MN, Whitby E (2003) Postmortem MR imaging of the fetal and stillborn central nervous system. AJNR Am J Neuroradiol 24:22–27
Huisman TA, Wisser J, Stallmach T, Krestin GP, Huch R, Kubik-Huch RA (2002) MR autopsy in fetuses. Fetal Diagn Ther 17:58–64
Khong TY, Tanner AR (2006) Foetal and neonatal autopsy rates and use of tissue for research: The influence of ‘organ retention’ controversy and new consent process. J Paediatr Child Health 42:366–369
Nicholl RM, Balasubramaniam VP, Urquhart DS, Sellathurai N, Rutherford MA (2007) Postmortem brain MRI with selective tissue biopsy as an adjunct to autopsy following neonatal encephalopathy. Eur J Paediatr Neurol 11:167–174
Royal College of Obstetricians and Gynaecologists, Royal College of Pathologists. Fetal and perinatal pathology: report of a joint working party. London: RCOG Press, 2001
Rushton DI (1998) Perinatal pathology: centralise or perish. Br J Obstet Gynaecol 105:5–7
Sebire NJ (2006) Towards the minimally invasive autopsy. Ultrasound Obstet Gynecol 28:865–867
Silver RM (2007) Fetal death. Obstet Gynecol 109:153–167
Wellman KF (1969) The needle autopsy. A retrospective evaluation of 294 consecutive cases. Am J Clin Pathol 52:441–444
Woodward PJ, Sohaey R, Harris DP, Jackson GM, Klatt EC, Alexander AL, Kennedy A (1997) Postmortem fetal MR imaging: comparison with findings at autopsy. AJR Am J Roentgenol 168:41–46
Acknowledgements
Members of the Cambridge post mortem MRI study group also include: Dr Justin Cross, Professor David J Lomas, and Ms Ilse Joubert (of the Department of Radiology, University of Cambridge and Addenbrooke’s Hospital). We are indebted to the parents who agreed to take part in this study at a very difficult time.
We also acknowledge the assistance of Andrew F Dean (Department of Histopathology, Addenbrooke’s Hospital), and Dr Nicholas Coleman (Hutchison-MRC Centre, Cambridge), and the paediatric pathology service staff of Addenbrooke’s Hospital: Nicola Wood, Gillian Kenyon, Simon Brown, and Michelle Macer. We also wish to thank the midwives and medical staff of the Rosie Hospital, Cambridge for their support.
This study was supported by a grant from the Trustees of the Addenbrooke’s Charities, and ACGB’s salary was supported by Cambridge Fetal Care.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Breeze, A.C.G., Jessop, F.A., Whitehead, A.L. et al. Feasibility of percutaneous organ biopsy as part of a minimally invasive perinatal autopsy. Virchows Arch 452, 201–207 (2008). https://doi.org/10.1007/s00428-007-0548-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-007-0548-7