Abstract
Purpose
Breaking up prolonged sitting can attenuate the postprandial rise in glucose and insulin. Whether such effects are dependent of the glycaemic index (GI) of the consumed carbohydrate is unknown. This study examined the acute effects of breaking up prolonged sitting following a low GI and a high GI breakfast on postprandial glucose and insulin concentrations.
Procedures
Fourteen adult males aged 22.1 ± 1.2 years completed four, 4 h experimental conditions: high GI breakfast followed by uninterrupted sitting (HGI-SIT), low GI breakfast followed by uninterrupted sitting (LGI-SIT), high GI breakfast followed by 2 min activity breaks every 20 min (HGI-ACT), and low GI breakfast followed by 2 min activity breaks every 20 min (LGI-ACT). Positive incremental area under the curve (iAUC) for glucose and insulin (mean [95% CI]) for each 4 h experimental condition was calculated. Statistical analyses were completed using linear mixed models.
Results
The sitting × breakfast GI interaction was not significant for glucose positive iAUC (P = 0.119). Glucose positive iAUC (mmol/L 4 h−1) was significantly lower in the activity breaks conditions than the uninterrupted sitting conditions (2.07 [2.24, 2.89] vs. 2.56 [1.74, 2.40], respectively, P = 0.004) and significantly lower in the low GI conditions than the high GI conditions (2.13 [1.80, 2.45] vs. 2.51 [2.18, 2.84], respectively, P = 0.022). Insulin concentrations did not differ between conditions (P ≥ 0.203).
Conclusions
Breaking up prolonged sitting and lowering breakfast GI independently reduced postprandial glucose responses. This indicates that interrupting prolonged sitting and reducing dietary GI are beneficial approaches for reducing cardiometabolic disease risk.
Similar content being viewed by others
Introduction
Postprandial hyperglycaemia refers to an exaggerated elevation in blood glucose following the consumption of a meal. Elevated postprandial glucose is a significant risk factor for cardiometabolic disease (de Vegt et al. 2001); thus, interventions to reduce the rise in postprandial blood glucose may be important in disease prevention (Tuomilehto et al. 2001). In terms of dietary interventions, the glycaemic index (GI) quantifies the glycaemic response of carbohydrate-rich foods, with low GI foods resulting in a slow and steady release of glucose compared with HGI foods (Jenkins et al. 1981). Accordingly, acute experimental studies demonstrate a reduction in the postprandial glucose and insulin response to low GI compared with energy-matched high GI mixed meals (Galgani et al. 2006; Stevenson et al. 2009). Although low GI diets are commonly recommended to lower postprandial glycaemia (Buyken et al. 2010), adherence to this type of diet can be poor (Nisak et al. 2010). Furthermore, GI is not the single factor controlling postprandial glycaemia and there has been recent research interest in the potential impact of minimising prolonged periods of sitting during the postprandial period.
Independent of time spent in moderate-to-vigorous physical activity, spending a high amount of time sedentary is a significant risk factor for cardiometabolic disease (Wilmot et al. 2012). Acute experimental studies have observed reduced postprandial glucose and insulin concentrations when prolonged sitting is interrupted with 2 min bouts of light- or moderate-intensity activity every 20 min following the consumption of a standardised mixed liquid test drink (Bailey et al. 2016; Bailey and Locke 2015; Dunstan et al. 2012). However, an important limitation of these studies is that the liquid meals provided may not reflect habitual dietary patterns in free-living conditions. Furthermore, these studies have not considered or reported the GI of the meals provided. Indeed, it is possible that the attenuated rise in postprandial glucose and insulin concentrations from breaking up prolonged sitting depends on the degree of glycaemia induced by the meal. Specifically, there would be a greater ‘scope for improvement’ following meals inducing a greater glycaemic response. Thus, an understanding of whether breaking up prolonged sitting is effective in suppressing postprandial glucose responses to both low and high GI meals is required.
Evidence on the combined effects of breakfast GI and breaking up prolonged sitting on postprandial glycaemia would help inform combined activity and dietary approaches for preventing cardiometabolic disease. The primary aim of the present study was to examine the effect of breaking up prolonged sitting following the consumption of a high and a low GI breakfast on postprandial glucose and insulin responses in young adult males. It was hypothesised that breaking up prolonged sitting would reduce postprandial glucose concentrations, but that this reduction would be more pronounced following the consumption of a high GI breakfast compared with a low GI breakfast.
Methods
Study overview
This randomised four-way crossover design study was approved by the University of Bedfordshire School of Sport Science and Physical Activity Ethics Review Committee and conformed to the principles set out in the Declaration of Helsinki. All testing took place at the University of Bedfordshire Sport and Exercise Science Laboratories. After preliminary measures, participants completed four experimental conditions: (1) high GI breakfast + uninterrupted sitting, (2) low GI breakfast + uninterrupted sitting, (3) high GI breakfast + activity breaks, and (4) low GI breakfast + activity breaks. Each condition was separated by a 6–14 day washout period. The conditions were conducted in an incomplete counterbalanced order pre-determined using the Latin square method.
Participants
Fourteen adult males aged 21–25 years gave informed consent to participate in the study following a written and verbal explanation of the nature and risks involved. Exclusion criteria were any blood borne disease, clinically diagnosed diabetes, taking glucose-lowering and/or lipid-lowering medication, known physical activity contraindications, major illness/injury (acute or chronic), or other health issues that may limit the ability to perform the necessary activity bouts.
Sample size calculations
The primary outcome was postprandial glucose positive incremental area under the curve (iAUC). Our previous research reported a 16% reduction (effect size, F = 0.61) in 5 h postprandial glucose total area under the curve (AUC) when breaking up prolonged sitting with 2 min walking every 20 min versus uninterrupted sitting (Bailey and Locke 2015). Allowing for an intervention effect of 16% change in glucose positive iAUC, 10% within-group error variance, a within-person correlation of 0.6, 80% power, and an α of 0.05, it was estimated that 12 participants would be required for this complete four-treatment crossover design. Fourteen participants were recruited to allow for potential dropout.
Preliminary measures
Stature was measured to the nearest 0.01 m using a stadiometer (Holtain Ltd., Crymych, Wales). Body mass was measured to the nearest 0.1 kg and body fat estimated to the nearest 0.1% using the Tanita BC-418 Segmental Body Composition Analyzer (Tanita Corp., Tokyo, Japan). Participants were then familiarised with use of the Borg Rating of Perceived Exertion (RPE) scale (Borg 1982) and completed a test to determine a moderate-intensity speed on a motorised treadmill (Woodway PPS55 Med-i, GmbH, Germany). In line with previous research (Bailey et al. 2016; Dunstan et al. 2012), the test began at a speed of 5 km h−1 and increased by 0.5 km h−1 every 2 min until an RPE of 12–14 (somewhat hard) was reached. Subsequently, the speed that elicited an RPE of 12–14 for each individual was used for the experimental conditions; the treadmill speeds ranged between 6.5 and 8.0 km h−1.
Experimental protocol
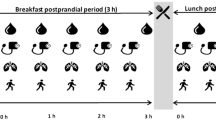
Figure 1 shows the experimental protocol. The 4 h experimental conditions were based on previous research that demonstrated suppressed postprandial glucose and insulin responses when breaking up prolonged sitting with 2 min activity every 20 min (Bailey and Locke 2015; Dunstan et al. 2012) and were as follows:
-
1.
High GI breakfast + uninterrupted sitting (HGI-SIT): participants consumed a high GI breakfast followed by uninterrupted sitting at a desk, rising only to void.
-
2.
Low GI breakfast + uninterrupted sitting (LGI-SIT): as HGI-SIT, but participants consumed a low GI breakfast.
-
3.
High GI breakfast + activity breaks (HGI-ACT): participants consumed a high GI breakfast and then rose from the seated position every 20 min to complete 2 min bouts of moderate-intensity activity on a motorised treadmill, providing a total of 22 min activity (11 activity breaks). Participants returned to a seated position at a desk between activity breaks.
-
4.
Low GI breakfast + activity breaks (LGI-ACT): as HGI-ACT, but participants consumed a low GI breakfast.
Participants were asked to refrain from exercise, alcohol, and caffeine in the 24 h before each experimental condition. Participants were asked to weigh and record all food and liquid intake in a food diary for 24 h before the first experimental condition and to replicate their diet (quantity and timings) prior to each subsequent experimental condition (Bailey et al. 2016). All participants attended the laboratory at ~0800 h after an overnight fast and were instructed to minimise activity during their commute. Upon arrival, participants rested for 30 min before a fasting blood sample was taken. A standardised high or low GI breakfast meal was then consumed within 15 min and the 4 h experimental condition commenced following the last mouthful of food. Participants were asked to void immediately prior to consumption of the breakfast meal and were then permitted to void when needed during the remainder of the conditions. The toilets were located ~30 m from the laboratory. Participants were supervised throughout the conditions to ensure adherence to the protocols and were permitted to watch DVDs, read books, magazines, or newspapers, talk, or work on a laptop computer. During sitting periods, participants were instructed to minimise excessive movement.
Breakfast meal and water consumption
The high and low GI breakfast meals provided 1 g carbohydrate kg body mass−1 for each participant. The meals were matched for macronutrient content (70% carbohydrate, 16% fat and 14% protein), energy and fluid, but the high GI breakfast contained 40% less fibre than the low GI breakfast. The high GI breakfast consisted of cornflakes, skimmed milk, white bread and strawberry jam. The low GI breakfast consisted of muesli, semi-skimmed milk, apple and peaches. The GI values for each food item were obtained from the International Tables of Glycaemic Index and Glycaemic Load Values 2008 (Atkinson et al. 2008) and breakfast GI was calculated using weighted means of the GI values for the component foods (Wolever and Jenkins 1986). The calculated GI values of the high and low GI breakfasts were 78 and 47, respectively. During the first experimental conditions, consumption time was recorded and participants were asked to replicate this consumption time as closely as possible in each subsequent condition. Water was provided ad libitum during the first condition and the volume consumed was replicated during each subsequent condition.
Blood collection and biochemistry
During each experimental condition, capillary blood samples were collected by finger prick (Haemolance Plus Lancet, Prospect Diagnostics, Dronfield, UK). Capillary rather than venous blood sampling is preferred for reliable GI testing (Wolever et al. 2003). The first sample was taken in a fasted state at −15 min and followed by subsequent samples at 15, 30, 45, 60, 90, 120, 180 and 240 min during the 4 h postprandial period. Hourly blood samples were obtained immediately prior to the activity breaks (i.e., for 60, 120, 180 and 240 min). At each time point, ~600 μL of whole blood was collected into two EDTA-containing microvettes (Microvette CB300 EDTA, Sarstedt Ltd, Leicester, UK). Blood glucose was analysed immediately using the YSI 2300 STAT plus glucose and lactate analyzer (YSI Inc., Yellow Springs, OH, USA) using 30 μL of whole blood from one microvette. The YSI uses a steady state measurement methodology, where membrane based glucose oxidase catalyses the oxidation of glucose to gluconic acid and hydrogen peroxide. The difference between the sample generated plateau current and the initial baseline current is proportional to the glucose concentration. The YSI was calibrated at the start of every experimental condition and every 45 min thereafter. The remaining whole blood (~570 μL) was centrifuged at 2500×g for 5 min (Heraeus Pico 17, Thermo Scientific, Loughborough, UK). Subsequently, the plasma was extracted and stored at −80 °C for later batch analysis of insulin. Plasma insulin concentration was measured in duplicate using an enzyme-linked immunosorbent assay (Mercodia, Uppsala, Sweden). To eliminate inter-assay variation, samples from each participant were analysed in the same run. The intra-assay coefficient of variation was 9.2%.
Calculation of outcome variables
Positive iAUC and total AUC were calculated for glucose and insulin for each 4 h condition using the trapezoidal method. For the positive iAUC calculation, any value below baseline (fasting) was treated as a baseline value; it has been suggested that this method more accurately describes glycaemic responses to food compared with total AUC (Le Floch et al. 1990). Use of this method also permits direct comparisons with previous research (Bailey et al. 2016).
Statistical analyses
Statistical analyses were completed using SPSS version 22.0 (SPSS Inc., Armonk, N.Y., USA). Quantile–Quantile plots were used to check the normality assumption of the results obtained for each of the conditions. This method was preferred over null hypothesis significance testing to check statistical assumptions (Grafen and Hails 2002). Linear mixed models were used to evaluate the main effect of sitting (uninterrupted sitting vs. activity breaks) and breakfast GI (high GI vs. low GI) and the sitting × breakfast GI interaction for the dependent variables. Condition and covariates (age, fasting glucose/insulin concentrations, and body fat%) were fixed factors and subjects were random factors within the models. When there was a significant sitting × breakfast GI interaction, post hoc comparisons examined differences between the four individual conditions using Sidak correction for multiple comparisons. Cohens’ d effect sizes were calculated if P ≤ 0.200 to examine whether the magnitude of differences between conditions was potentially meaningful; 0.2, 0.5 and 0.8 indicated a small, medium or large effect, respectively (Cohen 1988). Data are presented as mean (95% confidence interval [CI]) unless stated otherwise. The two-tailed alpha level for significance testing was set as P ≤ 0.05.
Results
Descriptive characteristics of the participants are reported in Table 1. Eight participants had a body mass index (BMI) ≥ 25 kg/m2 and six had a BMI < 25 kg/m2. Thirteen participants had a low body fat level (i.e. <25%) (Shah and Braverman 2012). Although one participant had a high body fat level (≥25%), their fasting glucose concentration was normal (<6.1 mmol/L) (World Health Organization 2006) and their postprandial glucose response was lower than ten of the other participants. Therefore, this participant was not excluded from the analyses.
Table 2 shows fasting and AUC values for glucose and insulin concentrations for each condition. Fasting glucose concentrations did not differ significantly between conditions and the sitting × breakfast GI interaction was not significant. All participants had a fasting glucose concentration of ≤4.77 mmol/L, which is within the normal range (World Health Organization 2006). Although the sitting × breakfast GI interaction for postprandial glucose iAUC did not reach significance, there was a large effect size for the difference between HGI-SIT and HGI-ACT (d = 0.97), HGI-SIT and LGI-ACT (d = 1.14), and HGI-SIT and LGI-SIT (d = 0.83). There was a small effect size for the difference between LGI-SIT and LGI-ACT (d = 0.31), LGI-SIT and HGI-ACT (d = 0.14), and LGI-ACT and HGI-ACT (d = 0.17). There was a significant main effect of sitting for glucose positive iAUC, with concentrations in the activity breaks conditions being 21% lower than the uninterrupted sitting conditions (2.07 mmol/L 4 h [1.74, 2.40] vs. 2.56 mmol/L 4 h [2.24, 2.89], respectively). The effect size for this difference was large (d = 0.76). The main effect of breakfast GI was also significant, with glucose positive iAUC concentrations 16% lower in the low GI breakfast conditions than the high GI breakfast conditions (2.13 mmol/L 4 h [1.80, 2.45] vs. 2.51 mmol/L 4 h [2.18, 2.84], respectively). There was a medium effect size for this difference (d = 0.59).
Analysis of glucose total AUC also revealed that the sitting × breakfast GI interaction was not significant (Table 2). There was a main effect for sitting and for breakfast GI, with glucose total AUC being significantly lower in the activity breaks conditions than the uninterrupted sitting conditions (19.15 mmol/L 4 h [18.79, 19.52] vs. 19.77 mmol/L 4 h [19.40, 20.13], respectively; d = 0.86) and significantly lower in the low GI breakfast conditions than the high GI breakfast conditions (19.04 mmol/L 4 h [18.67, 19.40] vs. 19.88 mmol/L 4 h [19.52, 20.24], respectively; d = 1.17). Glucose concentrations over time for each trial are shown in Fig. 2.
Changes in blood glucose (a) and plasma insulin (b) concentrations during the low glycaemic index (GI) breakfast + activity breaks (LGI-ACT), low GI breakfast + uninterrupted sitting (LGI-SIT), high GI breakfast + activity breaks (HGI-ACT), and high GI breakfast + uninterrupted sitting (HGI-SIT) conditions. Data are mean and 95% confidence interval. Some error bars have been omitted for clarity
The sitting × breakfast GI interaction for fasting insulin concentration was significant (Table 2). Fasting insulin concentration was higher in LGI-SIT than LGI-ACT (P = 0.037), but there were no significant differences between any of the other conditions (P ≥ 0.059). The sitting × breakfast GI interaction and the main effects of sitting and breakfast GI for postprandial insulin positive iAUC and total AUC were all non-significant (Table 2). Insulin concentrations over time for each trial are shown in Fig. 2.
Conclusions
This is the first study to assess the acute postprandial glucose and insulin response to breaking up prolonged sitting following meals differing in GI. The present study found that breaking up prolonged sitting with moderate-intensity activity acutely lowers the postprandial glucose response following a low or high GI breakfast. Similarly, lowering the GI of breakfast acutely lowered the postprandial glucose response regardless of whether postprandial sitting was interrupted with activity breaks or not. There was minimal evidence that combining these two interventions had a cumulative added impact on lowering postprandial glycaemia.
The finding that postprandial glucose responses are lowered when sitting is interrupted with moderate-intensity activity is synonymous with previous experimental research (Bailey et al. 2016; Dunstan et al. 2012; Peddie et al. 2013). These studies have observed benefits in postprandial glucose despite differences in the age, weight status, and metabolic status of the participants, and methodological differences in the duration of the experimental conditions, duration and frequency of interruptions to sitting time, and the test meal frequency, timing, and calorie content. The present study contributes to current knowledge by demonstrating that the benefits of breaking up prolonged sitting are observable following consumption of meals differing in GI.
In contrast to previous research in normal weight, overweight and obese adults (Dunstan et al. 2012; Peddie et al. 2013), the present study did not observe reductions in postprandial insulin responses to breaking up sitting time. Dunstan et al. (2012) studied older (45–65 years) males and females and it is possible that the younger male participants in the present study were able to increase their glucose disposal in response to the activity breaks via insulin-independent pathways, such as increased translocation of the intracellular glucose transporter protein GLUT-4 (Latouche et al. 2013), increased permeability of muscles cells to glucose (Wallberg-Henriksson et al. 1988), and increased carbohydrate oxidation (Peddie et al. 2013) that may occur in response to muscular contractions. However, Peddie et al. (2013) studied males and females of a similar age to the present study. It is possible that the longer observation period, more frequent test meal consumption and differences in test meal composition could explain the lowered insulin response with interruptions to sitting time in the study by Peddie et al. (2013), which was not observed in the present study.
In line with previous research using similar mixed breakfast meals (Stevenson et al. 2009; Zakrzewski et al. 2012), the high GI breakfast induced a larger glucose response compared with the low GI breakfast. Somewhat unexpectedly, the postprandial peak in glucose and insulin concentrations was higher in the low GI compared with the high GI breakfast conditions. Thus, the reduced glucose iAUC with low GI breakfast consumption was due to lower glucose concentrations that occurred after the postprandial peak (i.e., from 15 to 240 min). Although there is evidence that GI predicts the peak in blood glucose for individual food items (Brand-Miller et al. 2009), GI values are defined by glucose iAUC rather than the peak blood glucose concentration after food consumption. Our data suggests that predicted GI values for mixed meals may not necessarily reflect expected differences in peak glucose concentrations. Thus, further research is required to confirm the applicability of GI values from single food items to mixed meals when considering peak glucose concentrations. Despite the higher glucose response to the high GI breakfast, the postprandial insulin iAUC was not different between the breakfast meals. Thus, reduced insulin-stimulated disposal of glucose may have contributed to the higher overall glycaemic response to the high GI breakfast. Although the breakfasts in the present study were matched for carbohydrate, fat and protein, it should be noted that the higher fibre content in the low GI breakfast may have contributed to the lower glycaemic response by acting as a physical barrier and delaying access of digestive enzymes to breakdown carbohydrate (Jenkins et al. 1981; Nuttall 1993). With this in mind, it may be more appropriate to recommend low GI high-fibre breakfasts (rather than LGI breakfasts per se) for reducing postprandial glycaemia, but not necessarily for reducing peak glucose concentrations.
The non-significant sitting by breakfast GI interaction indicates that these interventions have independent effects on lowering postprandial glycaemia. Nevertheless, it should be highlighted that breaking up sitting lowered the glucose response by 30% following high GI breakfast consumption, but only by 11% following low GI breakfast consumption. The larger effect size for breaking up sitting following the high GI breakfast compared with the low GI breakfast could potentially be clinically meaningful, suggesting that breaking up sitting could have more pronounced benefits following higher GI breakfasts. With this in mind, the sitting by breakfast GI interaction may not have been significant due to a lack of statistical power in the present study. The relatively high glucose response to the high GI breakfast could explain why breaking up sitting resulted in a more pronounced reduction in postprandial glucose compared with a low GI breakfast. This could suggest that dietary GI may be important in determining the magnitude of response to interventions involving breaking up prolonged sitting. Thus, future research on the metabolic effects of breaking up prolonged sitting should consider and report the GI content of the meals provided to participants.
It is unknown whether the magnitude of the observed reductions in postprandial glucose in response to breaking up prolonged sitting in this study equates to clinical significance in a young adult population. Nevertheless, postprandial excursions in glucose are a cardiometabolic disease risk factor in healthy, nondiabetic individuals (Levitan et al. 2004), suggesting that the findings of this study have meaningful implications. Furthermore, reductions in dietary GI remain an important public health target for the prevention of cardiometabolic disease (Buyken et al. 2010). However, it should be emphasised that the findings reported here are based on young, healthy males and may not apply directly to treat clinical populations.
This study has several potential limitations. The sample included young adult males and the generalisability of the findings to other population groups is uncertain. This study compared the effects of consuming different GI meals and breaking up prolonged sitting over a period of 4 h following a single meal. Responses to multiple meals consumed across the course of the day thus cannot be inferred, nor can the long term responses to the consumption of a low GI diet or breaking up prolonged sitting. Participants were asked to refrain from exercise 24 h prior to experimental conditions. However, an acute bout of exercise may enhance insulin sensitivity for up to 48 h (Mikines et al. 1988); therefore, future studies should consider asking participants to refrain from exercise for a minimum of 48 h prior to experimental conditions. Fasting insulin concentrations were higher in the low GI + uninterrupted sitting condition than the low GI + activity breaks condition. However, this difference was small and the positive iAUC calculations account for differences in baseline (fasting) values between conditions (Le Floch et al. 1990). In addition, all analyses were adjusted for fasting glucose and insulin concentrations. Another potential limitation of the study is that the GI values of the breakfast meals used were predicted, and there is evidence that the predicted GI of mixed meals does not always reflect the GI of individual food items (Flint et al. 2005). Nevertheless, the low GI breakfast induced significantly lower glucose positive iAUC compared with the high GI breakfast, as predicted. Finally, it is unknown whether the peak in postprandial glucose observed at 15 min in the low GI conditions could be attenuated by breaking up prolonged sitting as the first interruption in sitting time in the present study did not occur until 20 min.
In conclusion, breaking up prolonged sitting with moderate-intensity activity acutely lowers the postprandial glucose response following consumption of a low and high GI breakfast in young adult males. Similarly, lowering the GI of breakfast reduced the postprandial glucose response independent of whether the postprandial period was interrupted with activity breaks or not. These findings emphasise the importance of avoiding prolonged periods of sitting and high GI breakfasts to reduce cardiometabolic disease risk.
Abbreviations
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- GI:
-
Glycaemic index
- HGI-ACT:
-
High glycaemic index breakfast + activity breaks
- HGI-SIT:
-
High glycaemic index breakfast + uninterrupted sitting
- iAUC:
-
Incremental area under the curve
- LGI-ACT:
-
Low glycaemic index breakfast + activity breaks
- LGI-SIT:
-
Low glycaemic index breakfast + uninterrupted sitting
- RPE:
-
Rating of perceived exertion
References
Atkinson FS, Foster-Powell K, Brand-Miller JC (2008) International tables of glycemic index and glycemic load values: 2008. Diabetes Care 31:2281–2283. doi:10.2337/dc08-1239
Bailey DP, Locke CD (2015) Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. J Sci Med Sport 18:294–298. doi:10.1016/j.jsams.2014.03.008
Bailey DP, Broom DR, Chrismas BC, Taylor L, Flynn E, Hough J (2016) Breaking up prolonged sitting time with walking does not affect appetite or gut hormone concentrations but does induce an energy deficit and suppresses postprandial glycaemia in sedentary adults. Appl Physiol Nutr Metab 41:324–331. doi:10.1139/apnm-2015-0462
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14:377–381
Brand-Miller JC, Stockmann K, Atkinson F, Petocz P, Denyer G (2009) Glycemic index, postprandial glycemia, and the shape of the curve in healthy subjects: analysis of a database of more than 1000 foods. Am J Clin Nutr 89:97–105. doi:10.3945/ajcn.2008.26354
Buyken AE, Mitchell P, Ceriello A, Brand-Miller J (2010) Optimal dietary approaches for prevention of type 2 diabetes: a life-course perspective. Diabetologia 53:406–418. doi:10.1007/s00125-009-1629-8
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Erlbaum, Hillsdale, NJ
de Vegt F et al (2001) Relation of impaired fasting and postload glucose with incident type 2 diabetes in a Dutch population: the Hoorn Study. JAMA 285:2109–2113
Dunstan DW et al (2012) Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care 35:976–983. doi:10.2337/dc11-1931
Flint A, Moller BK, Raben A, Tetens I, Holst JJ, Astrup A (2005) The use of glycaemic index tables to predict glycaemic index of breakfast meals. Br J Nutr 94:135–136
Galgani J, Aguirre C, Diaz E (2006) Acute effect of meal glycemic index and glycemic load on blood glucose and insulin responses in humans. Nutr J 5:22. doi:10.1186/1475-2891-5-22
Grafen G, Hails R (2002) Modern statistics for the life sciences, 1st edn. Oxford University Press, New York
Jenkins DJ et al (1981) Glycemic index of foods: a physiological basis for carbohydrate exchange. Am J Clin Nutr 34:362–366
Latouche C, Jowett JB, Carey AL, Bertovic DA, Owen N, Dunstan DW, Kingwell BA (2013) Effects of breaking up prolonged sitting on skeletal muscle gene expression. J Appl Physiol (1985) 114:453–460. doi:10.1152/japplphysiol.00978.2012
Le Floch JP, Escuyer P, Baudin E, Baudon D, Perlemuter L (1990) Blood glucose area under the curve. Methodological aspects. Diabetes Care 13:172–175
Levitan EB, Song Y, Ford ES, Liu S (2004) Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta-analysis of prospective studies. Arch Intern Med 164:2147–2155. doi:10.1001/archinte.164.19.2147
Mikines KJ, Sonne B, Farrell PA, Tronier B, Galbo H (1988) Effect of physical exercise on sensitivity and responsiveness to insulin in humans. Am J Physiol 254:E248–E259
Nisak MYB, Abd Talib R, Norimah AK, Gilbertson H, Azmi KN (2010) Improvement of dietary quality with the aid of a low glycemic index diet in Asian patients with type 2 diabetes mellitus. J Am Coll Nutr 29:161–170
Nuttall FQ (1993) Dietary fiber in the management of diabetes. Diabetes 42:503–508
Peddie MC, Bone JL, Rehrer NJ, Skeaff CM, Gray AR, Perry TL (2013) Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. Am J Clin Nutr 98:358–366. doi:10.3945/ajcn.112.051763
Shah NR, Braverman ER (2012) Measuring adiposity in patients: the utility of body mass index (BMI), percent body fat, and leptin. PLoS One 7:e33308. doi:10.1371/journal.pone.0033308
Stevenson EJ, Astbury NM, Simpson EJ, Taylor MA, Macdonald IA (2009) Fat oxidation during exercise and satiety during recovery are increased following a low-glycemic index breakfast in sedentary women. J Nutr 139:890–897. doi:10.3945/jn.108.101956
Tuomilehto J et al (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344:1343–1350. doi:10.1056/NEJM200105033441801
Wallberg-Henriksson H, Constable SH, Young DA, Holloszy JO (1988) Glucose transport into rat skeletal muscle: interaction between exercise and insulin. J Appl Physiol (1985) 65:909–913
Wilmot EG et al (2012) Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia 55:2895–2905. doi:10.1007/s00125-012-2677-z
Wolever TM, Jenkins DJ (1986) The use of the glycemic index in predicting the blood glucose response to mixed meals. Am J Clin Nutr 43:167–172
Wolever TM et al (2003) Determination of the glycaemic index of foods: interlaboratory study. Eur J Clin Nutr 57:475–482. doi:10.1038/sj.ejcn.1601551
World Health Organization (2006) Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia (Available at: http://www.who.int/diabetes/publications/Definition%20and%20diagnosis%20of%20diabetes_new.pdf, Accessed 22 Dec 2014)
Zakrzewski JK, Stevenson EJ, Tolfrey K (2012) Effect of breakfast glycemic index on metabolic responses during rest and exercise in overweight and non-overweight adolescent girls. Eur J Clin Nutr 66:436–442. doi:10.1038/ejcn.2011.175
Acknowledgements
The authors would like to thank the participants for their involvement in this study. The authors would also like to thank Sarita Govender and Joseph Swithenby for assisting in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Guido Ferretti.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bailey, D.P., Maylor, B.D., Orton, C.J. et al. Effects of breaking up prolonged sitting following low and high glycaemic index breakfast consumption on glucose and insulin concentrations. Eur J Appl Physiol 117, 1299–1307 (2017). https://doi.org/10.1007/s00421-017-3610-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-017-3610-4