Abstract
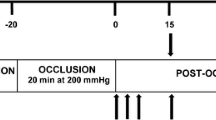
Vasodilatory mechanisms controlling post-exercise or post-ischemic hyperemia are thought to be under redundant control and remain incompletely understood. A maximal metabolic stimulus evoked by ischemic exercise (IE) might limit redundancy by full activation of multiple pathways. We tested whether nitric oxide (NO) and/or prostaglandins contribute to the hyperemic response to IE. 17 subjects were randomized into two groups and performed three trials of IE during control (saline), N G-monomethyl-l-arginine (l-NMMA; NOS inhibition) (protocol 1) or ketorolac (cyclooxygenase inhibition) infusion (protocol 2), and combined l-NMMA/ketorolac infusion via a brachial arterial catheter. Forearm blood flow (FBF) was measured with venous occlusion plethysmography following IE trials consisting of 5 min of ischemia and simultaneous rhythmic handgrip exercise (final 2 min). Peak and total (area under the curve) FBF and blood pressure (MAP) were measured for 3 min after each trial. Forearm vascular conductance (FVC) was calculated as FBF/MAP. Change (Δ) in peak FBF and FVC from baseline differed only between peak FBF for the saline and l-NMMA + ketorolac trials in protocol 1. Peak ΔFBF was 26.8 ± 2.5, 30.0 ± 2.8, and 33.9 ± 3.6 ml 100 ml−1 min−1 for saline, l-NMMA, and l-NMMA + ketorolac trials (P = 0.04). For protocol 1 (n = 8), total ΔFVC was 59.6 ± 4.3, 57.8 ± 6.0, and 59.9 ± 5.6 ml 100 ml−1 100 mmHg−1 for saline, l-NMMA, and l-NMMA + ketorolac trials, (P = 0.82). For protocol 2 (n = 9), total ΔFVC was 54.2 ± 5.0, 56.9 ± 4.5, and 56.5 ± 5.3 ml 100 ml−1 100 mmHg−1 for saline, ketorolac, and ketorolac + l-NMMA trials, (P = 0.69). These results suggest that NO and PGs are not obligatory for the hyperemic response to IE, and other vasodilator mechanisms predominate.



Similar content being viewed by others

References
Adkisson EJ, Casey DP, Beck DT, Gurovich AN, Martin JS, Braith RW (2010) Central, peripheral and resistance arterial reactivity: fluctuates during the phases of the menstrual cycle. Exp Biol Med (Maywood) 235(1):111–118
Boushel R, Langberg H, Gemmer C, Olesen J, Crameri R, Scheede C, Sander M, Kjaer M (2002) Combined inhibition of nitric oxide and prostaglandins reduces human skeletal muscle blood flow during exercise. J Physiol 543(Pt 2):691–698
Carlsson I, Sollevi A, Wennmalm A (1987) The role of myogenic relaxation, adenosine and prostaglandins in human forearm reactive hyperaemia. J Physiol 389:147–161
Casey DP, Joyner MJ (2009) NOS inhibition blunts and delays the compensatory dilation in hypoperfused contracting human muscles. J Appl Physiol 107(6):1685–1692
Casey DP, Joyner MJ (2011) Prostaglandins do not contribute to the nitric oxide-mediated compensatory vasodilation in hypoperfused exercising muscle. Am J Physiol Heart Circ Physiol 301(1):H261–H268
Casey DP, Madery BD, Curry TB, Eisenach JH, Wilkins BW, Joyner MJ (2010) Nitric oxide contributes to the augmented vasodilatation during hypoxic exercise. J Physiol 588(Pt 2):373–385
Dietz NM, Rivera JM, Eggener SE, Fix RT, Warner DO, Joyner MJ (1994) Nitric oxide contributes to the rise in forearm blood flow during mental stress in humans. J Physiol 480(Pt 2):361–368
Dinenno FA, Joyner MJ (2004) Combined NO and PG inhibition augments alpha-adrenergic vasoconstriction in contracting human skeletal muscle. Am J Physiol Heart Circ Physiol 287(6):H2576–H2584
Duffy SJ, New G, Tran BT, Harper RW, Meredith IT (1999) Relative contribution of vasodilator prostanoids and NO to metabolic vasodilation in the human forearm. Am J Physiol 276(2 Pt 2):H663–H670
Duncker DJ, Bache RJ (2008) Regulation of coronary blood flow during exercise. Physiol Rev 88:1009–1086
Engelke KA, Halliwill JR, Proctor DN, Dietz NM, Joyner MJ (1996) Contribution of nitric oxide and prostaglandins to reactive hyperemia in human forearm. J Appl Physiol 81(4):1807–1814
Joyner MJ, Dietz NM, Shepherd JT (2001) From Belfast to Mayo and beyond: the use and future of plethysmography to study blood flow in human limbs. J Appl Physiol 91(6):2431–2441
Kilbom A, Wennmalm A (1976) Endogenous prostaglandins as local regulators of blood flow in man: effect of indomethacin on reactive and functional hyperaemia. J Physiol 257(1):109–121
Kirby BS, Carlson RE, Markwald RR, Voyles WF, Dinenno FA (2007) Mechanical influences on skeletal muscle vascular tone in humans: insight into contraction-induced rapid vasodilatation. J Physiol 583(Pt 3):861–874
Lopez MG, Silva BM, Joyner MJ, Casey DP (2012) Ischemic exercise hyperemia in the human forearm: reproducibility and roles of adenosine and nitric oxide. Eur J Appl Physiol 112(6):2065–2072
Markwald RR, Kirby BS, Crecelius AR, Carlson RE, Voyles WF, Dinenno FA (2011) Combined inhibition of nitric oxide and vasodilating prostaglandins abolishes forearm vasodilatation to systemic hypoxia in healthy humans. J Physiol 589(Pt 8):1979–1990
Minson CT, Halliwill JR, Young TM, Joyner MJ (2000) Influence of the menstrual cycle on sympathetic activity, baroreflex sensitivity, and vascular transduction in young women. Circulation 101(8):862–868
Mortensen SP, Gonzalez-Alonso J, Damsgaard R, Saltin B, Hellsten Y (2007) Inhibition of nitric oxide and prostaglandins, but not endothelial-derived hyperpolarizing factors, reduces blood flow and aerobic energy turnover in the exercising human leg. J Physiol 581(Pt 2):853–861
Mortensen SP, Nyberg M, Thaning P, Saltin B, Hellsten Y (2009) Adenosine contributes to blood flow regulation in the exercising human leg by increasing prostaglandin and nitric oxide formation. Hypertension 53(6):993–999
Naylor HL, Shoemaker JK, Brock RW, Hughson RL (1999) Prostaglandin inhibition causes an increase in reactive hyperaemia after ischaemic exercise in human forearm. Clin Physiol 19(3):211–220
Nyberg M, Mortensen SP, Thaning P, Saltin B, Hellsten Y (2010) Interstitial and plasma adenosine stimulate nitric oxide and prostacyclin formation in human skeletal muscle. Hypertension 56(6):1102–1108
Patterson GC, Whelan RF (1955) Reactive hyperaemia in the human forearm. Clin Sci (Lond) 14(2):197–211
Schrage WG, Joyner MJ, Dinenno FA (2004) Local inhibition of nitric oxide and prostaglandins independently reduces forearm exercise hyperaemia in humans. J Physiol 557(Pt 2):599–611
Schrage WG, Dietz NM, Joyner MJ (2006) Effects of combined inhibition of ATP-sensitive potassium channels, nitric oxide, and prostaglandins on hyperemia during moderate exercise. J Appl Physiol 100(5):1506–1512
Schrage WG, Eisenach JH, Joyner MJ (2007) Ageing reduces nitric-oxide- and prostaglandin-mediated vasodilatation in exercising humans. J Physiol 579(Pt 1):227–236
Sinoway LI, Musch TI, Minotti JR, Zelis R (1986) Enhanced maximal metabolic vasodilatation in the dominant forearms of tennis players. J Appl Physiol 61(2):673–678
Wendelhag I, Fagerberg B, Wikstrand J (1999) Adding ischaemic hand exercise during occlusion of the brachial artery increases the flow-mediated vasodilation in ultrasound studies of endothelial function. Clin Physiol 19(4):279–283
Wilson JR, Kapoor S (1993) Contribution of endothelium-derived relaxing factor to exercise-induced vasodilation in humans. J Appl Physiol 75(6):2740–2744
Acknowledgments
We would like to acknowledge Drs. Tim Curry and John Eisenach for their instrumental role in making these experiments possible. Also, we would like to thank Branton Walker, Chris Johnson, Alex Allen, John Roger Shepherd, and Alex White for technical assistance, and Pamela Engrav for her aid in recruiting research participants. This publication was made possible by National Institutes of Health grants HL46493 (M.J.J.), AR-55819 (D.P.C.) and CTSA RR-024150. The Caywood Professorship via the Mayo Foundation also supported this research. We also acknowledge stipend support from Brazil’s Coordination for the Improvement of Higher Education Personnel (CAPES).
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Keith Phillip George.
Rights and permissions
About this article
Cite this article
Lopez, M.G., Silva, B.M., Joyner, M.J. et al. Roles of nitric oxide and prostaglandins in the hyperemic response to a maximal metabolic stimulus: redundancy prevails. Eur J Appl Physiol 113, 1449–1456 (2013). https://doi.org/10.1007/s00421-012-2570-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-012-2570-y