Abstract
Purpose
To assess the safety and efficacy of ultrasound coagulation of the ciliary body in refractory glaucoma.
Methods
This prospective multicenter interventional study was conducted in two Italian university-affiliated glaucoma centers: St. Orsola-Malpighi Teaching Hospital (Bologna, Italy) and University Eye Clinic of Genoa (Genoa, Italy). The main inclusion criterion was the diagnosis of glaucoma with a baseline intraocular pressure (IOP) ≥ 21 mmHg while on maximum topical and systemic medical hypotensive treatment. The EyeOP1 device (Eye Tech Care, Rillieux-la-Pape, France), which was employed in the study, uses miniaturized transducers to produce high-intensity focused ultrasound (HIFU). Treatment consisted of the sequential activation of each transducer lasting 4 s (group 1), 6 s (group 2) or 8 s (group 3). Hypotensive medications were interrupted after surgery and then prescribed only if postoperative IOP was ≥ 21 mmHg during follow-up visits. Patients were assessed before and 1, 7, 14, 30, 90 and 180 days after the procedure. Primary outcomes were the mean IOP reduction in the overall population and in groups 1, 2 and 3, and the rates of complete success, qualified success and failure.
Results
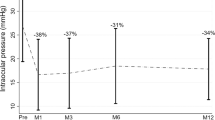
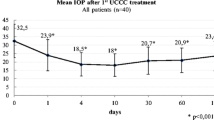
Thirty eyes (16 open-angle, 10 angle-closure and 4 neovascular glaucoma) of 30 patients were included. The mean preoperative IOP was 30.1 ± 10.5 mmHg. Twenty-nine patients completed the entire study follow-up; one patient exited from the study 3 months after HIFU and underwent trabeculectomy. At days 1 and 180, the mean IOP was significantly reduced (18.4 ± 7.2 and 20.2 ± 6.2 mmHg, respectively; all p < 0.0001). Group 3 patients (8-s ultrasound exposure time) showed a greater IOP reduction than the other two groups (−16.2 ± 8.3 for group 3 vs. −8.8 ± 6.6 for group 2 and −3.7 ± 6.5 for group 1; p = 0.02 and p < 0.001, respectively). Qualified and complete success was achieved in 23.3 and 46.7% of patients, respectively; treatment failure was recorded in 6.6%.
Conclusions
Ultrasonic coagulation of the ciliary body is a safe and effective procedure for reducing IOP in refractory glaucoma. The increase in ultrasound exposure time appears to improve the response rate and the global efficacy of the procedure, with no detrimental effect on safety.



Similar content being viewed by others
References
Traverso CE, Walt JG, Kelly SP, Hommer AH, Bron AM, Denis P et al (2005) Direct costs of glaucoma and severity of the disease: a multinational long term study of resource utilisation in Europe. Br J Ophthalmol 89:1245–1249
European Glaucoma Society (2014) Terminology and guidelines for glaucoma. In: EGS Guidelines, 4th edn. Dogma Srl, Savona Italy, pp 139–169
De Roetth A Jr (1965) Cryosurgery for the treatment of glaucoma. Trans Am Ophthalmol Soc 63:189–204
Maus M, Katz LJ (1990) Choroidal detachment, flat anterior chamber, and hypotony as complications of neodymium: YAG laser cyclophotocoagulation. Ophthalmology 97:69–72
Uram M (1992) Ophthalmic laser microendoscope ciliary process ablation in the management of neovascular glaucoma. Ophthalmology 99:1823–1828
Al-Ghamdi S, Al-Obeidan S, Tomey KF, Al-Jadaan I (1993) Transscleral neodymium:YAG laser cyclophotocoagulation for end-stage glaucoma, refractory glaucoma, and painful blind eyes. Ophthalmic Surg 24:526–529
Kosoko O, Gaasterland DE, Pollack IP, Enger CL (1996) Long-term outcome of initial ciliary ablation with contact diode laser transscleral cyclophotocoagulation for severe glaucoma. The Diode Laser Ciliary Ablation Study Group. Ophthalmology 103:1294–1302
Hamard P, Gayraud JM, Kopel J, Valtot F, Quesnot S, Hamard H (1997) Treatment of refractory glaucomas by transscleral cyclophotocoagulation using semiconductor diode laser. Analysis of 50 patients followed-up over 19 months. J Fr Ophthalmol 20:125–133
Sabri K, Vernon SA (1999) Scleral perforation following trans-scleral cyclodiode. Br J Ophthalmol 83:502–503
Vernon SA, Koppens JM, Menon GJ, Negi AK (2006) Diode laser cycloablation in adult glaucoma: long-term results of a standard protocol and review of current literature. Clin Experiment Ophthalmol 34:411–420
Aptel F, Charrel T, Palazzi X, Chapelon JY, Denis P, Lafon C (2010) Histologic effects of a new device for high-intensity focused ultrasound cyclocoagulation. Invest Ophthalmol Vis Sci 51:5092–5098. doi:10.1167/iovs.09-5135
Aptel F, Charrel T, Lafon C, Romano F, Chapelon JY, Blumen-Ohana E et al (2011) Miniaturized high-intensity focused ultrasound device in patients with glaucoma: a clinical pilot study. Invest Ophthalmol Vis Sci 52:8747–8753. doi:10.1167/iovs.11-8137
Aptel F, Dupuy C, Rouland JF (2014) Treatment of refractory open-angle glaucoma using ultrasonic circular cyclocoagulation: a prospective case series. Curr Med Res Opin 30:1599–1605. doi:10.1185/03007995.2014.910509
Aptel F, Béglé A, Razavi A, Romano F, Charrel T, Chapelon JY et al (2014) Short- and long-term effects on the ciliary body and the aqueous outflow pathways of high-intensity focused ultrasound cyclocoagulation. Ultrasound Med Biol 40:2096–2106. doi:10.1016/j.ultrasmedbio.2014.04.017
Charrel T, Aptel F, Birer A, Chavrier F, Romano F, Chapelon JY et al (2011) Development of a miniaturized HIFU device for glaucoma treatment with conformal coagulation of the ciliary bodies. Ultrasound Med Biol 37:742–754. doi:10.1016/j.ultrasmedbio.2011.01.017
Aptel F, Lafon C (2012) Therapeutic applications of ultrasound in ophthalmology. Int J Hyperthermia 28:405–418. doi:10.3109/02656736.2012.665566
Denis P, Aptel F, Rouland J-F, Nordmann J-P, Lachkar Y, Renard J-P et al (2015) Cyclocoagulation of the ciliary bodies by high-intensity focused ultrasound: a 12-month multicenter study. Invest Ophthalmol Vis Sci 56:1089–1096. doi:10.1167/iovs.14-14973
Mastropasqua R, Agnifili L, Fasanella V, Toto L, Brescia L, Di Staso S et al (2016) Uveo-scleral outflow pathways after ultrasonic cyclocoagulation in refractory glaucoma: an anterior segment optical coherence tomography and in vivo confocal study. Br J Ophthalmol. doi:10.1136/bjophthalmol-2015-308069
Melamed S, Goldenfeld M, Cotlear D, Skaat A, Moroz I (2015) High-intensity focused ultrasound treatment in refractory glaucoma patients: results at 1 year of prospective clinical study. Eur J Ophthalmol 25:483–489. doi:10.5301/ejo.5000620
Aptel F, Denis P, Rouland JF, Renard JP, Bron A (2016) Multicenter clinical trial of high-intensity focused ultrasound treatment in glaucoma patients without previous filtering surgery. Acta Ophthalmol 94:e268–277. doi:10.1111/aos.12913
Coleman DJ, Lizzi FL, Driller J, Rosado AL, Burgess SE, Torpey JH et al (1985) Therapeutic ultrasound in the treatment of glaucoma. II. Clinical applications. Ophthalmology 92:347–353
Valtot F, Kopel J, Haut J (1989) Treatment of glaucoma with high intensity focused ultrasound. Int Ophthalmol 13:167–170
Burgess SE, Silverman RH, Coleman DJ, Yablonski ME, Lizzi FL, Driller J et al (1986) Treatment of glaucoma with high-intensity focused ultrasound. Ophthalmology 93:831–838
Yip LW, Yong SO, Earnest A, Ji J, Lim BA (2009) Endoscopic cyclophotocoagulation for the treatment of glaucoma: an Asian experience. Clin Experiment Ophthalmol 37:692–697
Lima FE, Beniz Neto J, Toscano D, Carvalho DM, Avila MP (2009) Endoscopic cyclophotocoagulation in refractory glaucomas: a long term study. Rev Bras Oftalmol 68:146–151
Murthy GJ, Murthy PR, Murthy KR, Kulkarni VV, Murthy KR (2009) A study of the efficacy of endoscopic cyclophotocoagulation for the treatment of refractory glaucomas. Indian J Ophthalmol 57:127–132
Chen J, Cohn RA, Lin SC, Cortes AE, Alvarado JA (1997) Endoscopic photocoagulation of the ciliary body for treatment of refractory glaucomas. Am J Ophthalmol 124:787–796
Egbert PR, Fiadoyor S, Budenz DL, Dadzie P, Byrd S (2001) Diode laser transscleral cyclophotocoagulation as a primary surgical treatment for primary open-angle glaucoma. Arch Ophthalmol 119:345–350
Gupta V, Agarwal HC (2000) Contact trans-scleral diode laser cyclophotocoagulation treatment for refractory glaucomas in the Indian population. Indian J Ophthalmol 48:295–300
Nabili S, Kirkness CN (2004) Trans-scleral diode laser cyclophoto-coagulation in the treatment of diabetic neovascular glaucoma. Eye 18:352–356
Iliev ME, Gerber S (2007) Long-term outcome of trans-scleral diode laser cyclo-photocoagulation in refractory glaucoma. Br J Ophthalmol 91:1631–1635
Tan AM, Chockalingam M, Aquino MC, Lim ZI, See JL, Chew PT (2010) Micropulse transscleral diode laser cyclophotocoagulation in the treatment of refractory glaucoma. Clin Experiment Ophthalmol 38:266–272
Kuchar S, Moster MR, Reamer CB, Waisbourd M (2016) Treatment outcomes of micropulse transscleral cyclophotocoagulation in advanced glaucoma. Lasers Med Sci 31:393–396
Supuran CT (2010) Carbonic anhydrase inhibitors. Bioorg Med Chem Lett 20:3467–3474. doi:10.1016/j.bmcl.2010.05.009
Fraunfelder FT, Bagby GC (2000) Monitoring patients taking oral carbonic anhydrase inhibitors. Am J Ophthalmol 130:221–223
Gilmour KM (2010) Perspectives on carbonic anhydrase. Comp Biochem Physiol A Mol Integr Physiol 157:193–197. doi:10.1016/j.cbpa.2010.06.161
Acknowledgements
The authors wish to thank Dr. Ada Dormi, Math.ST, Statistical Service, DIMEC, University of Bologna, for her skillful assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Giannaccare, G., Vagge, A., Gizzi, C. et al. High-intensity focused ultrasound treatment in patients with refractory glaucoma. Graefes Arch Clin Exp Ophthalmol 255, 599–605 (2017). https://doi.org/10.1007/s00417-016-3563-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3563-z