Abstract
Purpose
To study morphological and functional characteristics of myopic lamellar macular hole (LMH) with posterior staphyloma.
Methods
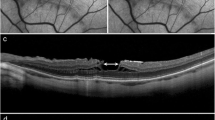
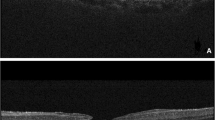
Retrospective observational longitudinal study. Forty myopic eyes affected by LMH and posterior staphyloma have been examined. Pathological myopia was defined as axial length equal or superior to 26.5 mm. LMH was defined on the basis of the following characteristics: irregular foveal contour, inner retinal defect with or without intraretinal splitting and absence of full thickness retinal defect. Demographic and functional parameters were: age, sex, status of lens and best corrected visual acuity (BCVA). Tomographic parameters were: type of LMH, macular retinoschisis (MRS), posterior vitreous detachment (PVD), type of epiretinal membrane (ERM), integrity of ellipsoid zone (EZ) and external limiting membrane (ELM), residual foveal thickness (RFT) and maximal diameter of intraretinal splitting (MDIRS).
Results
The statistical analysis showed a significant prevalence of posterior vitreous adherence in the atypical ERM subgroup (P = 0.001). EZ (P = 0.006) and ELM (P = 0.007) damages were significantly associated with the atypical ERM subgroup. RFT was statistically lower in the atypical ERM subgroup compared to the conventional ERM subgroup (P = 0.015). During the follow-up, the statistical analysis showed a significant reduction of RFT in the atypical ERM subgroup (P = 0.041).
Conclusions
Myopic lamellar macular hole (LMH) associated with atypical ERM is a more severe clinical entity than myopic LMH associated with conventional ERM.






Similar content being viewed by others
References
Witkin AJ, Ko TH, Fujimoto JG, Schuman JS, Baumal CR, Rogers AH, Reichel E, Duker J (2006) Redefining lamellar holes and the vitreomacular interface: an ultrahigh-resolution optical coherence tomography study. Ophthalmology 113(3):388–397
Reibaldi M, Parravano M, Varano M, Longo A, Avitabile T, Uva MG, Zagari M, Toro M, Boscia F, Boccassini B, Chiaravalloti A, Mariotti C, Reibaldi A (2012) Foveal microstructure and functional parameters in lamellar macular hole. Am J Ophthalmol 154(6):974–980.e1
Bottoni F, Deiro AP, Giani A et al (2013) The natural history of lamellar macular holes: a spectral domain optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol 251:467–475
Pang CE, Spaide RF, Freund KB (2015) Comparing functional and morphologic characteristics of lamellar macular holes with and without lamellar hole-associated epiretinal proliferation. Retina 35(4):720–726
Parolini B, Schumann RG, Cereda MG, Haritoglou C, Pertile G (2011) Lamellar macular hole: a clinicopathologic correlation of surgically excised epiretinal membranes. Invest Ophthalmol Vis Sci 52(12):9074–9083
Pang CE, Spaide RF, Freund KB (2014) Epiretinal proliferation seen in association with lamellar macular holes: a distinct clinical entity. Retina 34(8):1513–1523
Schumann RG, Compera D, Schaumberger MM, Wolf A, Fazekas C, Mayer WJ, Kamppik A, Haritoglou C (2105) Epiretinal membrane characteristics correlate with photoreceptor layer defects in lamellar macular holes and macular pseudoholes. Retina 35:727–735
Compera D, Entchev E, Haritoglou C, Scheler R, Mayer WJ, Wolf A, Kampik A, Schumann RG (2015) Lamellar hole-associated epiretinal proliferation in comparison to epiretinal membranes of macular pseudoholes. Am J Ophthalmol 160(2):373–384
Duker JS, Waheed NK, Goldman DR (2014) Myopic macular schisis in: handbook of retinal OCT: optical coherence tomography. Saunders Elsevier Inc, Philadelphia, pp 50–51
Tanaka Y, Shimada N, Moriyama M, Hayashi K, Yoshida T, Tokoro T, Ohno-Matsui K (2011) Natural history of lamellar macular holes in highly myopic eyes. Am J Ophthalmol 152(1):96–99
Morgan I, Rose K (2005) How genetic is school myopia? Prog Retin Eye Res 24:1–38
Pan CW, Ramamurthy D, Saw SM (2012) Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt 32:3–16
Spaide RF, Ohno-Matsui K, Yannuzzi LA (2013) Pathologic myopia. Springer, New York, pp 177–185
Panozzo G, Mercanti A (2004) Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol 122(10):1455–1460
Takano M, Kishi S (1999) Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthalmol 128(4):472–476
Baba T, Ohno Matsui K, Futagami S, Yoshida T, Yasuzumi K, Kojima A, Tokoro T, Mochizuki M (2003) Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol 135(3):338–342
Ikuno Y, Sayanagi K, Ohji M, Kamei M, Gomi F, Harino S, Fujikado T, Tano Y (2004) Vitrectomy and internal limiting membrane peeling for myopic foveoschisis. Am J Ophthalmol 137(4):719–724
Gaucher D, Haouchine B, Tadayoni R, Massin P, Erginay A, Benhamou N, Gaudric A (2007) Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol 143(3):455–462
Benhamou N, Massin P, Haouchine B, Erginary A, Gaudric A (2002) Macular retinoschisis in highly myopic eyes. Am J Ophthalmol 133(6):794–800
Shimada N, Ohno-Matsui K, Baba T, Futagami S, Tokoro T, Mochizuki M (2006) Natural course of macular retinoschisis in highly myopic eyes without macular hole or retinal detachment. Am J Ophthalmol 142(3):497–500
Sun CB, Liu Z, Xue AQ, Yao K (2010) Natural evolution from macular retinoschisis to full-thickness macular hole in highly myopic eyes. Eye (Lond) 24(12):1787–1791
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
For this type of study, formal consent is not required.
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00417-016-3383-1.
Rights and permissions
About this article
Cite this article
Rino, F., Elena, Z., Ivan, M. et al. Lamellar macular hole in high myopic eyes with posterior staphyloma: morphological and functional characteristics. Graefes Arch Clin Exp Ophthalmol 254, 2141–2150 (2016). https://doi.org/10.1007/s00417-016-3371-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3371-5