Abstract
Purpose
To investigate whether a new macular hole closure index (MHCI) could predict anatomic outcome of macular hole surgery.
Methods
A vitrectomy with internal limiting membrane peeling, air-fluid exchange, and gas tamponade were performed on all patients. The postoperative anatomic status of the macular hole was defined by spectral-domain OCT.
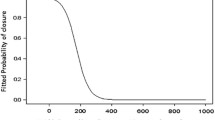
MHCI was calculated as (M+N)/BASE based on the preoperative OCT status. M and N were the curve lengths of the detached photoreceptor arms, and BASE was the length of the retinal pigment epithelial layer (RPE layer) detaching from the photoreceptors. Postoperative anatomical outcomes were divided into three grades: A (bridge-like closure), B (good closure), and C (poor closure or no closure). Correlation analysis was performed between anatomical outcomes and MHCI. Receiver operating characteristic (ROC) curves were derived for MHCI, indicating good model discrimination. ROC curves were also assessed by the area under the curve, and cut-offs were calculated. Other predictive parameters reported previously, which included the MH minimum, the MH height, the macular hole index (MHI), the diameter hole index (DHI), and the tractional hole index (THI) had been compared as well.
Results
MHCI correlated significantly with postoperative anatomical outcomes (r = 0.543, p = 0.000), but other predictive parameters did not. The areas under the curves indicated that MHCI could be used as an effective predictor of anatomical outcome. Cut-off values of 0.7 and 1.0 were obtained for MHCI from ROC curve analysis. MHCI demonstrated a better predictive effect than other parameters, both in the correlation analysis and ROC analysis.
Conclusions
MHCI could be an easily measured and accurate predictive index for postoperative anatomical outcomes.




Similar content being viewed by others
References
Noyes HD (1871) Detachment of the retina, with laceration at the macula lutea. Trans Am Ophthalmol Soc 1:128–129
Kelly NE, Wendel RT (1991) Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol 109(5):654–659
Bainbridge J, Herbert E, Gregor Z (2008) Macular holes: vitreoretinal relationships and surgical approaches. Eye (Lond) 22(10):1301–1309
Park DW, Lee JH, Min WK (1998) The use of internal limiting membrane maculorrhexis in treatment of idiopathic macular holes. Korean J Ophthalmol 12(2):92–97
Margherio RR, Margherio AR, Williams GA et al (2000) Effect of perifoveal tissue dissection in the management of acute idiopathic full-thickness macular holes. Arch Ophthalmol 118(4):495–498
Smiddy WE, Feuer W, Cordahi G (2001) Internal limiting membrane peeling in macular hole surgery. Ophthalmology 108(8):1471–1476, discussion 7–8
Freeman WR, Azen SP, Kim JW et al (1997) Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes. Results of a multicentered randomized clinical trial. The Vitrectomy for Treatment of Macular Hole Study Group. Arch Ophthalmol 115(1):11–21
Polk TD, Smiddy WE, Flynn HW Jr (1996) Bilateral visual function after macular hole surgery. Ophthalmology; 103(3):422–426
Brooks HL Jr (2000) Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology 107(10):1939–1948, discussion 48–49
Lai MM, Williams GA (2007) Anatomical and visual outcomes of idiopathic macular hole surgery with internal limiting membrane removal using low-concentration indocyanine green. Retina 27(4):477–482
Haritoglou C, Neubauer AS, Reiniger IW et al (2007) Long-term functional outcome of macular hole surgery correlated to optical coherence tomography measurements. Clin Experiment Ophthalmol 35(3):208–213
Mester U, Becker M (1998) Prognosefaktoren bei der Makulachirurgie. Ophthalmologe 95:158–162
Haritoglou C, Gass CA, Schaumberger M et al (2001) Macular changes after peeling of the internal limiting membrane in macular hole surgery. Am J Ophthalmol 132:363–368
Gupta B, Laidlaw DA, Williamson TH et al (2009) Predicting visual success in macular hole surgery. Br J Ophthalmol 93:1488–1491
Kusuhara S, Teraoka Escano MF, Fujii S et al (2004) Prediction of postoperative visual outcome based on hole configuration by optical coherence tomography in eyes with idiopathic macular holes. Am J Ophthalmol 138(5):709–716
Ip MS, Baker BJ, Duker JS et al (2002) Anatomical outcomes of surgery for idiopathic macular hole as determined by optical coherence tomography. Arch Ophthalmol 120:29–35
Wakely L, Rahman R, Stephenson J (2012) A comparison of several methods of macular hole measurement using optical coherence tomography, and their value in predicting anatomical and visual outcomes. Br J Ophthalmol 96:1003–1007
Funata M, Wendel RT, De la Cruz Z et al (1992) Clinico-pathologic study of bilateral macular holes treated with pars plana vitrectomy and gas tamponade. Retina 12:289–298
Madreperla SA, Geiger GL, Funata M et al (1994) Clinicopathologic correlation of a macular hole treated by cortical vitreous peeling and gas tamponade. Ophthalmology 101:682–686
Ruiz-Moreno JM, Staicu C, Pinero DP et al (2008) Optical coherence tomography predictive factors for macular hole surgery outcome. Br J Ophthalmol 92(5):640–644
Chung SE, Lim DH, Kang SW et al (2010) Central photoreceptor viability and prediction of visual outcome in patients with idiopathic macular holes. Korean J Ophthalmol 24(4):213–218
Ullrich S, Haritoglou C, Gass C et al (2002) Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol 86(4):390–393
Jaycock PD, Bunce C, Xing W et al (2005) Outcomes of macular hole surgery: implications for surgical management and clinical governance. Eye (Lond) 19:879–884
Gass JD (1988) Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol 106:629–639
Almony A, Nudleman E, Shah GK et al (2012) Techniques, rationale, and outcomes of internal limiting membrane peeling. Retina (Philadelphia, Pa) 32(5):877–891
Recchia FM, Ruby AJ, Carvalho Recchia CA (2005) Pars plana vitrectomy with removal of the internal limiting membrane in the treatment of persistent diabetic macular edema. Am J Ophthalmol 139:447–454
Matsunaga N, Ozeki H, Hirabayashi Y et al (2005) Histopathologic evaluation of the limiting membrane surgically excised from eyes with diabetic maculopathy. Retina 25:311–316
Gandorfer A, Messmer EM, Ulbig MW, Kampik A (2000) Resolution of diabetic macular edema after surgical removal of the posterior hyaloids and the inner limiting membrane. Retina 20:126–133
Acknowledgments
This work was supported by a grant from the National Science and Technology Major Project (2011ZX09302-007-02). Co-corresponding author: Xiaoxin Li, Department of Ophthalmology, Peking University People’s Hospital, Xizhimen South Street 11, Xi Cheng District, 100044 Beijing, China. Telephone number: +861088325413. E-mail address: dr_lixiaoxin@163.com
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
The first two authors contributed equally to this work.
Rights and permissions
About this article
Cite this article
Liu, P., Sun, Y., Dong, C. et al. A new method to predict anatomical outcome after idiopathic macular hole surgery. Graefes Arch Clin Exp Ophthalmol 254, 683–688 (2016). https://doi.org/10.1007/s00417-015-3116-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3116-x