Abstract
Purpose
Descemet membrane endothelial keratoplasty (DMEK) is a standard procedure in patients with endothelial corneal disorders. We investigated the difficulty of unfolding and attaching the graft lamella and its correlation to characteristics of the graft lamella donor, preoperative patient characteristics, and the postoperative outcome.
Methods
After preparation of the graft lamella, we prospectively graded the unfolding of the graft lamella in 169 consecutive DMEK procedures between September 2012 and August 2013 at the Charité-Universitätsmedizin Berlin with four different grades. Various donor characteristics and preoperative patient characteristics were analyzed and correlated to the grading. Additionally, visual acuity, corneal thickness and endothelial cell density were measured and correlated.
Results
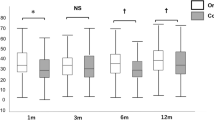
Donor characteristics (age [range, 49 – 79 years], gender, endothelial cell density, total storage time, storage de-swelling time, postmortem time) did not correlate to the grading. Preoperative visual acuity significantly influenced the grade of unfolding and attaching of the graft lamella (p = 0.023), while all other preoperative parameters (age, gender, indication for DMEK, preoperative endothelial cell density and preoperative central corneal thickness) showed no correlation. Visual acuity improved significantly after surgery (p < 0.001, preoperative 0.73 ±0.43 LogMAR versus 0.31 ±0.28 LogMAR after one month, 0.25 ±0.29 LogMAR after three months, and 0.21 ±0.25 LogMAR after six months). Visual acuity did not differ significantly between the grading groups at any time point postoperatively. After 6 months, the mean loss rate of endothelial cell density was 24.7 %. Grading group IV developed significantly higher endothelial loss after one month, after three months and after six months compared to the other groups (p = 0.039, p = 0.008, p = 0.048). Graft detachment requiring an additional intracameral air injection to fix the graft detachment (re-bubbling) occurred in 61 eyes (38.1 %). In eyes graded IV, more re-bubblings were necessary than in all other groups (grade I: 37.0 %; grade II: 44.7 %; grade III: 43.8 %; grade IV: 50.0 %; p = 0.128; df = 3; χ 2 = 5.676).
Conclusion
There is no correlation between corneal donor tissue characteristics and the degree of difficulty of unfolding using graft lamella older than 49 years. Therefore, it is not possible to select grafts best suited for DMEK surgery on the basis of donor characteristics when the donor age is above 50 years. Preoperative visual acuity influences the grade of difficulty. The rate of graft detachments and endothelial cell loss increases significantly with a more difficult graft unfolding. The proposed grading system may therefore be relevant for postoperative management.


Similar content being viewed by others
References
Melles GR, Wijdh RH, Nieuwendaal CP (2004) A technique to excise the descemet membrane from a recipient cornea (descemetorhexis). Cornea 23(3):286–288
Price FW Jr, Price MO (2005) Descemet’s stripping with endothelial keratoplasty in 50 eyes: a refractive neutral corneal transplant. J Refract Surg 21:339–345
Price FW Jr, Price MO (2006) Descemet’s stripping with endothelial keratoplasty in 200 eyes: Early challenges and techniques to enhance donor adherence. J Cataract Refract Surg 32:411–418
Melles GR, Ong TS, Ververs B, van der Wees J (2006) Descemet membrane endothelial keratoplasty (DMEK). Cornea 25:987–990
Melles GR, Ong TS, Ververs B, van der Wees J (2008) Preliminary clinical results of Descemet membrane endothelial keratoplasty. Am J Ophthalmol 145(2):222–227
Heinzelmann S, Hüther S, Böhringer D, Eberwein P, Reinhard T, Maier P (2014) Influence of donor characteristics on descemet membrane endothelial keratoplasty. Cornea 33(6):644–648
Dapena I, Ham L, Droutsas K, van Dijk K, Moutsouris K, Melles GR (2011) Learning curve in Descemet’s membrane endothelial keratoplasty: first series of 135 consecutive cases. Ophthalmology 118(11):2147–2154
Droutsas K, Giallouros E, Melles GR, Chatzistefanou K, Sekundo W (2013) Descemet membrane endothelial keratoplasty: learning curve of a single surgeon. Cornea 32(8):1075–1079
Monnereau C, Quilendrino R, Dapena I, Liarakos VS, Alfonso JF, Arnalich-Montiel F, Böhnke M, Pereira NC, Dirisamer M, Parker J, Droutsas K, Geerling G, Gerten G, Hashemi H, Kobayashi A, Naveiras M, Oganesyan O, Orduña Domingo E, Priglinger S, Stodulka P, Torrano Silva J Jr, Venzano D, Vetter JM, Yiu E, Melles GR (2014) Multicenter study of descemet membrane endothelial keratoplasty: first case series of 18 surgeons. JAMA Ophthalmol 132(10):1192–1198
Dapena I, Moutsouris K, Droutsas K, Ham L, van Dijk K, Melles GR (2011) Standardized “no-touch” technique for descemet membrane endothelial keratoplasty. Arch Ophthalmol 129(1):88–94
Joussen AM, Heussen FM, Joeres S, Llacer H, Prinz B, Rohrschneider K, Maaijwee KJ, van Meurs J, Kirchhof B (2006) Autologous translocation of the choroid and retinal pigment epithelium in age-related macular degeneration. Am J Ophthalmol 142(1):17–30
Heindl LM, Bucher F, Caramoy A, Hos D, Matthaei M, Cursiefen C (2014) Safety of donor tissue preparation and use of descemetoschisis and torn tissue in descemet membrane endothelial keratoplasty. Cornea 33(10):e7–e9
Laaser K, Bachmann BO, Horn FK, Schlötzer-Schrehardt U, Cursiefen C, Kruse FE (2011) Donor tissue culture conditions and outcome after descemet membrane endothelial keratoplasty. Am J Ophthalmol 151(6):1007–1018
Zhang J, Patel DV (2015) The pathophysiology of Fuchs’ endothelial dystrophy - A review of molecular and cellular insights. Exp Eye Res 130C:97–105
Dirisamer M, van Dijk K, Dapena I, Ham L, Oganes O, Frank LE, Melles GR (2012) Prevention and management of graft detachment in descemet membrane endothelial keratoplasty. Arch Ophthalmol 130(3):280–291
Acknowledgments
The authors thank Simone Baar and Dirk Scharf for technical support.
Anna-Karina B. Maier financial support provided by the “Friedrich C. Luft” Clinical Scientist Pilot Program funded by the Volkswagen Foundation and the Charité Foundation
Enken Gundlach financial support provided by the “Ernst und Bertha Grimmke Stiftung.”
Competing interest
None declared for all authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Anna-Karina B. Maier and Enken Gundlach contributed equally to this work.
Rights and permissions
About this article
Cite this article
Maier, AK.B., Gundlach, E., Schroeter, J. et al. Influence of the difficulty of graft unfolding and attachment on the outcome in descemet membrane endothelial keratoplasty. Graefes Arch Clin Exp Ophthalmol 253, 895–900 (2015). https://doi.org/10.1007/s00417-015-2939-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-2939-9