Abstract
Background
The main objective of hemodialysis (HD) is to correct the excessive accumulation and abnormal distribution of body fluid. Therefore, changes in the systemic hemodynamic parameters and in the ocular fluid volume and composition can occur during a single HD session. The aim of this study is to evaluate the short-term changes in the ophthalmologic findings after HD.
Methods
Thirty eyes of 30 patients with chronic renal failure (CRF) undergoing HD were analyzed. The subjects were categorized into two groups according to the cause of CRF. Detailed ophthalmologic examinations were performed immediately before and after HD. The relationships between the systemic hemodynamic changes and the ophthalmologic changes during a single HD session were evaluated.
Results
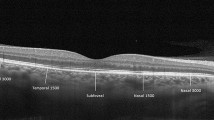
The results show that a body fluid correction after HD involves a change in the plasma colloid osmotic pressure. The mean intraocular pressure (IOP) decreased after HD with a mean decrease of 2.4 ± 2.1 mmHg and the central corneal thickness decreased with a mean change of 6.9 ± 5.4 μm. After HD, the ocular surface changed significantly; the tear break-up time (TBUT) and basal tear secretion (Schirmer's test) decreased, whereas the keratoepitheliopathy score increased. The macular thickness measured by spectral domain optical coherence tomography (SD-OCT) decreased after HD. The mean decrease in the central subfield thickness was 7.4 ± 9.9 μm. The ocular surface changes after HD affected the visual acuity and examination quality. A significant correlation was found between the changes in the systemic hemodynamic parameters and those in the ophthalmologic findings, except for the retinal thickness.
Conclusions
The changes in the ophthalmologic findings after HD were consistent and significant in all CRF subjects. These changes correlated with the increase in plasma colloid osmotic pressure. HD can correct the volume and composition of ocular fluid. Therefore, it can affect the ophthalmologic findings in a short period of time. In addition, for good examination quality, it is recommended that an ophthalmologic examination in CRF patients be performed on a non-dialysis day or prior to HD on a dialysis day. Furthermore, for accurate comparison of examination results, the time interval from an HD session to an ophthalmologic examination must be considered.


Similar content being viewed by others
References
Diaz-Couchoud P, Bordas FD, Garcia JR, Camps EM, Carceller A (2001) Corneal disease in patients with chronic renal insufficiency undergoing hemodialysis. Cornea 20:695–702
Charlton JF, Schwab IR, Stuchell R (1996) Tear hyperosmolarity in renal dialysis patients asymptomatic for dry eyes. Cornea 15:335–339
Hamed LM, Winward KE, Glaser JS, Schatz NJ (1989) Optic neuropathy in uremia. Am J Ophthalmol 108:30–35
Niutta A, Spicci D, Barcaroli I (1993) Fluoroangiographic findings in hemodialyzed patients. Ann Ophthalmol 25:375–380
Ravelli M, Scaroni P, Mombelloni S, Movilli E, Feller P, Apostoli P, De Maria G, Valotti C, Sciuto G, Maiorca R (1990) Acute visual disorders in patients on regular dialysis given desferrioxamine as a test. Nephrol Dial Transplant 5:945–949
Pahor D, Gracner B, Gracner T, Hojs R (2008) Optical coherence tomography findings in hemodialysis patients. Klin Monbl Augenheilkd 225:713–717
Tokuyama T, Ikeda T, Sato K (2000) Effects of haemodialysis on diabetic macular leakage. Br J Ophthalmol 84:1397–1400
Perkovich BT, Meyers SM (1988) Systemic factors affecting diabetic macular edema. Am J Ophthalmol 105:211–212
Matsuo T (2006) Disappearance of diabetic macular hard exudates after hemodialysis introduction. Acta Med Okayama 60:201–205
Miyata K, Amano S, Sawa M, Nishida T (2003) A novel grading method for superficial punctate keratopathy magnitude and its correlation with corneal epithelial permeability. Arch Ophthalmol 121:1537–1539
Early Treatment Diabetic Retinopathy Study Research Group (1991) ETDRS report No. 7: Early Treatment Diabetic Retinopathy Study design and baseline patient characteristics. Ophthalmology 98:741–756
Fauchald P (1986) Transcapillary colloid osmotic gradient and body fluid volumes in renal failure. Kidney Int 29:895–900
Levy J, Tovbin D, Lifshitz T, Zlotnik M, Tessler Z (2005) Intraocular pressure during haemodialysis: a review. Eye 19:1249–1256
Dinc UA, Ozdek S, Aktas Z, Guz G, Onol M (2010) Changes in intraocular pressure, and corneal and retinal nerve fiber layer thickness during hemodialysis. Int Ophthalmol 30:337–340
Tokuyama T, Ikeda T, Sato K (1998) Effect of plasma colloid osmotic pressure on intraocular pressure during haemodialysis. Br J Ophthalmol 82:751–753
Cecchin E, De Marchi S, Teiso F (1986) Intraocular pressure and hemodialysis. Nephron 43:73–74
Thomas J, Wang J, Rollins AM, Sturm J (2006) Comparison of corneal thickness measured with optical coherence tomography, ultrasonic pachymetry, and a scanning slit method. J Refract Surg 22:671–678
Tomazzoli L, De Natale R, Lupo A, Parolini B (2000) Visual acuity disturbances in chronic renal failure. Ophthalmologica 214:403–405
Tutt R, Bradley A, Begley C, Thibos LN (2000) Optical and visual impact of tear break-up in human eyes. Invest Ophthalmol Vis Sci 41:4117–4123
Li DQ, Chen Z, Song XJ, Luo L, Pflugfelder SC (2004) Stimulation of matrix metalloproteinases by hyperosmolarity via a JNK pathway in human corneal epithelial cells. Invest Ophthalmol Vis Sci 45:4302–4311
Lee SH, Kim HR, Yoon KC (2009) Tear film and ocular surface changes in chronic renal failure patients undergoing hemodialysis. J Korean Ophthalmol Soc 50:1167–1173
Theodossiadis PG, Theodoropoulou S, Neamonitou G, Grigoropoulos V, Liarakos V, Triantou E, Theodossiadis GP, Vlahakos DV (2012) Hemodialysis-induced alterations in macular thickness measured by optical coherence tomography in diabetic patients with end-stage renal disease. Ophthalmologica 227:90–94
Nagaoka T, Takeyama Y, Kanagawa S, Sakagami K, Yoshida A (2004) Effect of haemodialysis on retinal circulation in patients with end stage renal disease. Br J Ophthalmol 88:1026–1029
Tarakçıoğlu M, Erbağci AB, Usalan C, Deveci R, Kocabaş R (2003) Acute effect of hemodialysis on serum levels of the proinflammatory cytokines. Mediators Inflamm 12:15–19
Kuo HL, Chou CY, Liu YL, Yang YF, Huang CC, Lin HH (2008) Reduction of pro-inflammatory cytokines through hemodiafiltration. Ren Fail 30:796–800
van Velthoven ME, van der Linden MH, de Smet MD, Faber DJ, Verbraak FD (2006) Influence of cataract on optical coherence tomography image quality and retinal thickness. Br J Ophthalmol 90:1259–1262
Cheung CY, Leung CK, Lin D, Pang CP, Lam DS (2008) Relationship between retinal nerve fiber layer measurement and signal strength in optical coherence tomography. Ophthalmology 115:1347–1351
Huang J, Liu X, Wu Z, Sadda S (2011) Image quality affects macular and retinal nerve fiber layer thickness measurements on Fourier-domain optical coherence tomography. Ophthalmic Surg Lasers Imaging 42:216–221
Balasubramanian M, Bowd C, Vizzeri G, Weinreb RN, Zangwill LM (2009) Effects of image quality on tissue measurements obtained with spectral-domain optical coherence tomography. Opt Express 17:4019–4036
Gordon PL, Doyle JW, Johansen KL (2011) Postdialysis fatigue is associated with sedentary behavior. Clin Nephrol 75:426–433
Acknowledgments
This study was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MEST) (No. 2010-0012245) and by the Converging Research Center Program funded by the Ministry of Education, Science and Technology (2011K000697)
Financial support
None.
Conflict of interest
The authors have no proprietary interest in the material used in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have full control of all primary data and agree to allow Graefe’s Archive for Clinical and Experimental Ophthalmology to review the data if requested.
Rights and permissions
About this article
Cite this article
Jung, J.W., Yoon, M.H., Lee, S.W. et al. Effect of hemodialysis (HD) on intraocular pressure, ocular surface, and macular change in patients with chronic renal failure. Graefes Arch Clin Exp Ophthalmol 251, 153–162 (2013). https://doi.org/10.1007/s00417-012-2032-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-012-2032-6