Abstract
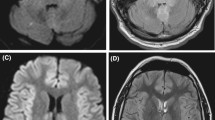
This study aims to explore the clinical features, radiological findings, management and the factors influencing prognosis in PCR-confirmed herpes simplex virus encephalitis (HSE). This is a retrospective review of consecutive patients diagnosed with HSE at Mayo Clinic, Rochester, MN, between January 1995 and December 2013. Only HSE cases confirmed by PCR were included. Univariate and multivariate analysis was used to identify factors associated with good (modified Rankin Scale of 0–2) or poor outcome (mRS of 3–6) at hospital discharge and 1-year follow-up. We identified 45 patients with HSE. Median age was 66 (IQR 53.5–78) years. HSE was caused by HSV-1 in 33 cases and by HSV-2 in 9. Nearly half had seizures upon admission or during hospitalization. The most common regions involved on MRI were the temporal lobe in 35 (87.5 %), insula in 28 (70.0 %), frontal lobe in 27 (67.5 %) and thalamus in 11 (27.5 %) patients. MRI pattern was quite homogeneous with HSV-1 infection, but much more heterogeneous with HSV-2. Good outcome at discharge and at 6–12 months was seen in 16 (35.6 %) and 27 (65.9 %) patients, respectively. On multivariate analyses, older age (p = 0.001), coma (p = 0.008), restricted diffusion on MRI (p = 0.005) and acyclovir started after the first day of admission (p = 0.050) were associated with poor outcome at discharge. Older age, development of coma, presence of restricted diffusion on brain MRI and delay in the administration of acyclovir portend poor outcome in HSE. Conversely, presence of seizures, focal neurological deficits, EEG abnormalities and location or extension of FLAIR/T2 abnormalities did not influence functional outcome.



Similar content being viewed by others
References
Cinque P, Cleator GM, Weber T, Monteyne P, Sindic CJ, van Loon AM (1996) The role of laboratory investigation in the diagnosis and management of patients with suspected herpes simplex encephalitis: a consensus report. The EU Concerted Action on Virus Meningitis and Encephalitis. J Neurol Neurosurg Psychiatry 61(4):339–345
Aurelius E, Johansson B, Skoldenberg B, Forsgren M (1993) Encephalitis in immunocompetent patients due to herpes simplex virus type 1 or 2 as determined by type-specific polymerase chain reaction and antibody assays of cerebrospinal fluid. J Med Virol 39(3):179–186
Whitley RJ, Soong SJ, Dolin R, Galasso GJ, Ch’ien LT, Alford CA (1977) Adenine arabinoside therapy of biopsy-proved herpes simplex encephalitis. National Institute of Allergy and Infectious Diseases collaborative antiviral study. N Engl J Med 297(6):289–294. doi:10.1056/NEJM197708112970601
Skoldenberg B, Forsgren M, Alestig K, Bergstrom T, Burman L, Dahlqvist E, Forkman A, Fryden A, Lovgren K, Norlin K et al (1984) Acyclovir versus vidarabine in herpes simplex encephalitis. Randomised multicentre study in consecutive Swedish patients. Lancet 2(8405):707–711
Whitley RJ, Alford CA, Hirsch MS, Schooley RT, Luby JP, Aoki FY, Hanley D, Nahmias AJ, Soong SJ (1986) Vidarabine versus acyclovir therapy in herpes simplex encephalitis. N Engl J Med 314(3):144–149. doi:10.1056/NEJM198601163140303
Aurelius E, Johansson B, Skoldenberg B, Staland A, Forsgren M (1991) Rapid diagnosis of herpes simplex encephalitis by nested polymerase chain reaction assay of cerebrospinal fluid. Lancet 337(8735):189–192
Sili U, Kaya A, Mert A (2014) Herpes simplex virus encephalitis: clinical manifestations, diagnosis and outcome in 106 adult patients. J Clin Virol 60(2):112–118. doi:10.1016/j.jcv.2014.03.010
Stahl JP, Mailles A, De Broucker T (2012) Herpes simplex encephalitis and management of acyclovir in encephalitis patients in France. Epidemiol Infect 140(2):372–381. doi:10.1017/S0950268811000483
Sheybani F, Arabikhan HR, Naderi HR (2013) Herpes simplex encephalitis (HSE) and its outcome in the Patients who were Admitted to a Tertiary Care Hospital in Mashhad, Iran, over a 10-year Period. J Clin Diagn Res 7(8):1626–1628. doi:10.7860/JCDR/2013/5661.3221
Hughes PS, Jackson AC (2012) Delays in initiation of acyclovir therapy in herpes simplex encephalitis. Can J Neurol Sci 39(5):644–648
Kapur N, Barker S, Burrows EH, Ellison D, Brice J, Illis LS, Scholey K, Colbourn C, Wilson B, Loates M (1994) Herpes simplex encephalitis: long term magnetic resonance imaging and neuropsychological profile. J Neurol Neurosurg Psychiatry 57(11):1334–1342
McGrath N, Anderson NE, Croxson MC, Powell KF (1997) Herpes simplex encephalitis treated with acyclovir: diagnosis and long term outcome. J Neurol Neurosurg Psychiatry 63(3):321–326
Pleumpanupat P, Danchaivijitr N, Danchaivijitr C (2009) Retrospective study of patients with herpes simplex encephalitis and positive CSF PCR. J Med Assoc Thai 92(Suppl 2):S95–100
Raschilas F, Wolff M, Delatour F, Chaffaut C, De Broucker T, Chevret S, Lebon P, Canton P, Rozenberg F (2002) Outcome of and prognostic factors for herpes simplex encephalitis in adult patients: results of a multicenter study. Clin Infect Dis 35(3):254–260. doi:10.1086/341405
Tunkel AR, Glaser CA, Bloch KC, Sejvar JJ, Marra CM, Roos KL, Hartman BJ, Kaplan SL, Scheld WM, Whitley RJ (2008) The management of encephalitis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 47(3):303–327. doi:10.1086/589747
Venkatesan A, Tunkel AR, Bloch KC, Lauring AS, Sejvar J, Bitnun A, Stahl JP, Mailles A, Drebot M, Rupprecht CE, Yoder J, Cope JR, Wilson MR, Whitley RJ, Sullivan J, Granerod J, Jones C, Eastwood K, Ward KN, Durrheim DN, Solbrig MV, Guo-Dong L, Glaser CA (2013) Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium. Clin Infect Dis 57(8):1114–1128. doi:10.1093/cid/cit458
Singh TD, Fugate JE, Hocker SE, Rabinstein AA (2015) Postencephalitic epilepsy: clinical characteristics and predictors. Epilepsia 56(1):133–138. doi:10.1111/epi.12879
Chow FC, Glaser CA, Sheriff H, Xia D, Messenger S, Whitley R, Venkatesan A (2015) Use of clinical and neuroimaging characteristics to distinguish temporal lobe herpes simplex encephalitis from its mimics. Clin Infect Dis 60(9):1377–1383. doi:10.1093/cid/civ051
Misra UK, Kalita J, Phadke RV, Wadwekar V, Boruah DK, Srivastava A, Maurya PK, Bhattacharyya A (2010) Usefulness of various MRI sequences in the diagnosis of viral encephalitis. Acta Trop 116(3):206–211. doi:10.1016/j.actatropica.2010.08.007
Sawlani V (2009) Diffusion-weighted imaging and apparent diffusion coefficient evaluation of herpes simplex encephalitis and Japanese encephalitis. J Neurol Sci 287(1–2):221–226. doi:10.1016/j.jns.2009.07.010
Okanishi T, Yamamoto H, Hosokawa T, Ando N, Nagayama Y, Hashimoto Y, Maihara T, Goto T, Kubota T, Kawaguchi C, Yoshida H, Sugiura K, Itomi S, Ohno K, Takanashi J, Hayakawa M, Otsubo H, Okumura A (2015) Diffusion-weighted MRI for early diagnosis of neonatal herpes simplex encephalitis. Brain Dev 37(4):423–431. doi:10.1016/j.braindev.2014.07.006
Singh TD, Fugate JE, Rabinstein AA (2015) The spectrum of acute encephalitis: causes, management, and predictors of outcome. Neurology 84(4):359–366. doi:10.1212/WNL.0000000000001190
Poissy J, Wolff M, Dewilde A, Rozenberg F, Raschilas F, Blas M, Georges H, Chaffaut C, Yazdanpanah Y (2009) Factors associated with delay to acyclovir administration in 184 patients with herpes simplex virus encephalitis. Clin Microbiol Infect 15(6):560–564. doi:10.1111/j.1469-0691.2009.02735.x
Gnann JW Jr, Skoldenberg B, Hart J, Aurelius E, Schliamser S, Studahl M, Eriksson BM, Hanley D, Aoki F, Jackson AC, Griffiths P, Miedzinski L, Hanfelt-Goade D, Hinthorn D, Ahlm C, Aksamit A, Cruz-Flores S, Dale I, Cloud G, Jester P, Whitley RJ (2015) Herpes simplex encephalitis: lack of clinical benefit of long-term valacyclovir therapy. Clin Infect Dis. doi:10.1093/cid/civ369
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Mayo Clinic Institutional Review Board and all patients or their representatives signed a consent form allowing their participation in the study. The research has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Singh, T.D., Fugate, J.E., Hocker, S. et al. Predictors of outcome in HSV encephalitis. J Neurol 263, 277–289 (2016). https://doi.org/10.1007/s00415-015-7960-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7960-8