Abstract
In amyotrophic lateral sclerosis (ALS) cerebrospinal fluid (CSF) analysis is usually performed to exclude inflammatory processes of the central nervous system. Although in a small subset of patients an intrathecal synthesis of IgG is detectable, usually there is no clear explanation for this evidence. This study investigates the occurrence of oligoclonal bands (OCBs) in the CSF of a large series of ALS patients, attempting a correlation with genotype data. CSF was collected from 259 ALS patients. CSF parameters were measured according to standard procedures, and detection of OCBs performed by isoelectric focusing. The patients were screened for mutations in SOD1, FUS, TARDBP, ANG, OPTN, and C9ORF72. We observed the presence of OCBs in the CSF of 9/259 ALS patients (3.5 %), and of disease-associated mutations in 12 cases. OCBs were significantly more frequent in mutation carriers compared to the remaining cohort (3/12 vs 6/247; p < 0.01). Among patients with OCBs, two patients had the TARDBP p.A382T mutation (one of which in homozygous state), and one the ANG p.P-4S variant. Both patients carrying the p.A382T mutation had an atypical phenotype, one of them manifesting signs suggestive of a cerebellar involvement, and the other presenting neuroradiological findings suggestive of an inflammatory disorder of the central nervous system. Our results suggest that ALS patients with OCBs may harbor mutations in disease-causing genes. We speculate that mutations in both TARDBP and ANG genes may disrupt the blood–brain barrier (BBB), promoting local immune responses and neuroinflammation. The role of mutant TARDBP and ANG genes on BBB integrity of ALS patients warrants further investigation.
Similar content being viewed by others
Introduction
Amyotrophic lateral sclerosis (ALS) is an adult-onset, rapidly progressive neurodegenerative disease mainly caused by the loss of motor neurons. Although most ALS cases are sporadic (SALS), ~10 % of them are familial (FALS), usually transmitted as an autosomal dominant trait. Pathogenic mutations are found in ~50 % of FALS and ~5 % of SALS cases, most commonly in SOD1, C9ORF72, TARDBP, FUS, but also in ANG and OPTN genes [8, 36, 40].
Several mechanisms have been proposed to explain the pathogenesis of ALS, including neuroinflammatory processes [33]. Although results from routine cerebrospinal fluid (CSF) analysis are usually unremarkable, several studies have shown an increase in total protein levels, and an altered CSF/serum albumin ratio (QAlb) in the CSF of ALS patients, suggesting an altered blood–brain barrier (BBB) permeability. Moreover, CSF oligoclonal bands (OCBs), indicating intrathecal synthesis of IgG, can be detected in 0.5–2 % of all ALS cases [2, 20, 37].
Although there is no evidence so far that the ALS-associated genes encode for proteins directly involved in maintaining BBB integrity, it is possible that disease-causing mutations may lead to BBB disruption and neuroinflammation. For instance, transgenic mice expressing mutant human SOD1G93A display an early BBB dysfunction [14, 31], while VEGF is one of the main modulators of the BBB integrity [24, 38]. Lastly, TDP-43, FUS, and OPTN immunoreactive inclusions have been observed in motor neurons as well as in astrocytic cytoplasmic processes [3, 19, 23], possibly altering the glial–vascular interface.
The aim of this study was to evaluate the occurrence of OCBs in the CSF of ALS individuals genetically characterized for ALS-associated genes.
Methods
Patients and controls
Our cohort included 259 ALS patients of Italian descent. All patients received a diagnosis of probable or definite ALS according to the El Escorial revised criteria at a tertiary care ALS Center. A subset of 13 patients had probable or definite familial ALS (FALS), according to the recently proposed criteria for FALS classification [4]. The demographic and clinical characteristics of our cohort are summarized in supplemental table 1. A panel of 40 control individuals without neurodegenerative or inflammatory diseases was used for comparison of CSF parameters. Specifically, the control panel included individuals with psychiatric disorders (16), vascular encephalopathy (15), cervical spondylotic myelopathy (6), diabetic neuropathy (2), and hereditary neuropathy with liability to pressure palsies (1).
Standard protocol approvals and patient consent
We received approval from the ethical standards committee on human experimentation of the IRCCS Istituto Auxologico Italiano. Written informed consent was obtained from all patients and healthy subjects participating in the study (consent for research). The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
CSF analysis
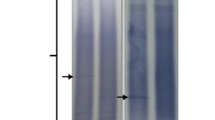
Lumbar puncture was performed in 259 ALS patients as part of the routine diagnostic procedures after they had given a written informed consent. The following CSF parameters were measured according to standard procedures and compared to serum levels: glucose, total proteins, total IgG, albumin, cell count. QAlb was calculated using the formula albuminCSF/albuminserum. Since CSF albumin completely derives from serum albumin and there is no intrathecal synthesis of the protein, QAlb represents the most useful parameter to assess the permeability of the BBB. Link index, an indirect parameter to evaluate intrathecal synthesis of IgG, was calculated using the formula (IgGCSF × albuminserum)/(IgGserum × albuminCSF). Normal ranges for CSF parameters, including QAlb and Link index, were determined according to international standards. Detection of OCBs was performed by isoelectric focusing on agarose gel and subsequent immunoblotting (IEF) with an anti-IgG antibody. By comparing OCBs in CSF and serum, a specific IEF pattern type was determined for each patient according to consensus criteria [12]. IEF is the current “gold standard” for detection of intrathecal IgG synthesis over other quantitative methods such as the Link index. In addition to biochemical tests, CSF samples were assayed for the presence of genetic material of the most common neurotropic viruses.
Hematological analysis
Complete blood cell count, erythrocyte sedimentation rate, C-reactive protein, serum protein electrophoresis, autoantibody screening, VDRL testing were performed in all patients. When the clinical presentation was suggestive, dosage of antibodies against Borrelia Burgdoferi and Human Immunodeficiency Virus 1 was also performed.
Genetic analysis
Genomic DNA was extracted from peripheral blood according to standard procedures. The coding regions of SOD1, TARDBP, FUS, ANG and OPTN genes were amplified by PCR and directly sequenced using BigDyeTerminator v 3.1 cycle sequencing kit on an automated 3100 ABI Prism Genetic Analyzer (Applied Biosystems, Foster City, CA, USA) as previously described [7, 9, 15, 16, 39]. The identified sequence variations were confirmed by sequencing an independent PCR product. The presence of the GGGGCC hexanucleotide repeat expansion in the first intron of C9ORF72 was also assessed through repeat-primed PCR. For the patient carrying the homozygous TARDBP p.A382T mutation we also performed a high-resolution array-Comparative Genomic Hybridization (CGH) analysis using the 244 K Human Genome CGH Microarray Kit (Agilent Technologies, Santa Clara, CA, USA) and a whole-genome single nucleotide polymorphism (SNP) genotyping using the Human660 W-Quad BeadChip (Illumina, San Diego, CA, USA). SNP genotype data were subsequently analyzed for Loss of Heterozigosity (LOH) and copy number variations (CNV) using the Genome Studio software (Illumina).
Results
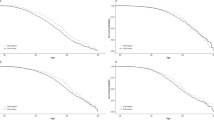
Cerebrospinal fluid (CSF) analysis in a cohort of 259 ALS patients (246 sporadic and 13 familial cases) revealed an average age-adjusted QAlb value of 5.2 ± 0.8, not dissimilar from that observed in a panel of 40 controls (4.6 ± 1.3; p > 0.05). Similarly, the average Link index, which quantifies the intrathecal IgG production, was not different among patients and controls (0.48 vs 0.47; p > 0.05). Interestingly, age-adjusted QAlb was elevated in 15/259 (5.8 %) ALS cases, while it was normal in all control individuals. OCBs were observed in the CSF of 9/259 (3.5 %) ALS patients and in no control samples. All patients with OCBs had apparently sporadic ALS (SALS). Five patients displayed on IEF a pattern type 2, indicating the presence of specific bands in the CSF only, but not in the serum. The remaining four presented OCBs in the CSF and additional identical bands both in the CSF and in the serum (pattern type 3, also indicative of intrathecal IgG synthesis). In two patients intrathecal IgG synthesis could be explained either by concurrent active neurosyphilis, or by a previous fetal olfactory ensheathing cells transplant in the frontal lobes. The remaining seven patients had no evidence of infectious or inflammatory diseases of the central nervous system. Paraproteinemia, lymphoma or any other systemic inflammatory or infectious conditions were also excluded. Other CSF parameters, including glucose levels and cell count, were normal in all individuals studied, and the screening for neurotrophic virus genomes was negative in all patients. The clinical features of the patients carrying OCBs are reported in Table 1.
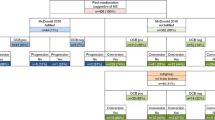
The genetic analysis revealed eight different ALS-associated mutations in 12 patients (4 %). In particular, we identified five individuals carrying mutations in SOD1 (p.A4V, p.F45C, p.G93D, p.I113T, and p.L144F), 4 in TARDBP (one p.G287S, and three p.A382T), and one each in FUS (p.R521C), OPTN (c.1401 + 4A > G) and ANG (p.P-4S). All mutations were observed in SALS cases, with the exception of p.A4V and p.L144F in the SOD1gene, which were found in two FALS patients. The clinical features of the mutated patients in the analyzed cohort are also summarized in Table 1. Several of them have already been described in other papers [7, 9, 15, 16, 39], and the mutations have been deposited in the ALSoD database (http://alsod.iop.kcl.ac.uk/). The nine ALS patients with OCBs in their CSF were screened for the presence of C9ORF72 hexanucleotide repeat expansion, and none of them was found to carry this mutation.
Among the group presenting with OCBs in the CSF, three patients (33.3 %) had ALS-associated mutations, namely the TARDBP p.A382T variant in two cases and the p.P-4S variant in the signal peptide of ANG in one case (Table 2). Interestingly, the TARDBP p.A382T mutation was found in homozygous state in one ALS individual. By performing high-resolution array-CGH we excluded deletions involving TARDBP genomic region (chr 1p36.22) or gene copy loss (supplemental fig. 1). Genotype data also confirmed the absence of CNV, consistent with the array-CGH results. LOH analysis demonstrated a 2.8 Mb region of extended homozygosity (chr1:10,891,317-13,713,882) encompassing TARDBP locus, suggesting that both alleles are identical by descent (supplemental fig. 2).
Average age-adjusted QAlb and Link index were similar both in the individuals positive for OCBs and in those harboring ALS-associated mutations, compared with the remaining cohort. Only patient A46, which carried the ANG p.P-4S mutation, had a mildly elevated QAlb, suggestive of a BBB leakage. The patient had a spinal onset, classic ALS phenotype (Table 1).
Conversely, both patients having OCBs in their CSF and the TARDBP p.A382T mutation displayed an atypical clinical phenotype. Patient A399, carrying the p.A382T variant in homozygous state, developed a bulbar-onset, rapidly progressive motor neuron disease at age 44, requiring invasive ventilation and a percutaneous endoscopic gastrostomy 17 months after onset of first symptoms. The clinical phenotype was mainly characterized by the presence of upper motor neuron signs. Brain MRI showed the presence of multiple small periventricular and subcortical white matter lesions (WMLs) (Fig. 1), without gadolinium contrast enhancement. This finding, together with the presence of OCBs in the CSF, and the absence of systemic inflammatory, infectious or autoimmune diseases, and of cardiovascular risk factors including thrombophilic conditions, was suggestive of a coexisting inflammatory demyelinating disease of the CNS.
The other patient (A338) developed a spinal onset motor neuron disease at age 59. The disease progression was markedly slow, and ten years after symptom onset the patient was still able to walk independently and had only mild bulbar signs. The neurological examination, however, showed uncharacteristic signs suggestive of an extramotoneuronal involvement. Ocular movement examination demonstrated saccadation of slow pursuit eye movements, slow saccades, and left gaze-evoked nystagmus. A postural as well as intention tremor of the upper limbs was present, together with dysmetria, bilateral dysdiadochokinesia and Holmes’ sign. Gait evaluation showed a spastic and ataxic paraparesis, with evident reduction of right-arm swinging. Postural reflexes were impaired with marked retropulsion at the pull test. Collectively, these findings suggested that the disease also affected the cerebellar and, possibly, the extrapyramidal system. Brain MRI was normal.
Noteworthy, the other two patients A10 and A349, carrying mutations in TARDBP gene, but without OCBs in the CSF, displayed a classic ALS phenotype, in particular the A349 individual with the same p.A382T variant.
Discussion
Several observations suggest that inflammatory processes contribute to ALS pathogenesis. Increased levels of albumin and immunoglobulin G (IgG) have been found in the CSF [25], while T-lymphocyte infiltration and local activation of immune cells have been observed in the spinal cord of ALS patients [11, 18]. Cerebral microglial activation is also a prominent feature of early-stage ALS, as demonstrated by neuroradiological studies [41]. Additionally, BBB dysfunction with subsequent neuroinflammation has been described as an early feature in ALS animal models [13].
Intrathecal synthesis of OCBs is suggestive of a local humoral immune response, and is a common feature of multiple sclerosis and other chronic inflammatory or infectious diseases of the CNS. OCBs, however, are rarely detected in neurodegenerative diseases such as ALS, being present in only 0.5–2 % of patients with motor neuron disease [20, 37]. This particular finding has usually been explained either by a former infection of the CNS or by an ongoing immune process in a subset of patients. In particular, patients with a concurrent paraproteinemia have a higher probability of presenting OCBs [43].
In our cohort we observed the presence of CSF OCBs in 3.5 % of all analyzed ALS cases, a frequency almost double than previously reported. This finding suggests that immune processes may play a role in a subset of ALS patients, either by contributing directly to the pathogenesis of the disease, or by representing a secondary event in response to neuronal damage. In either case, understanding why some individuals display inflammatory features may help comprehend the pathomechanisms of ALS.
In the majority of the patients positive for OCBs all the remaining CSF parameters analyzed were normal. In particular, with the exception of two individuals, QAlb was within normal limits, indicating a normal BBB permeability at the time the lumbar puncture was performed. It must be observed, however, that the evidence of intrathecal synthesis of IgG is nonetheless strongly suggestive of a qualitative BBB dysfunction leading to exposure of brain antigens to the systemic circulation, penetration of immunocompetent cells into the CNS, and ultimately, to a partial loss of the immune privilege of the CNS itself.
Since an evident cause for OCBs in the CSF could not be found for most of our patients, we aimed to evaluate if genetic factors might be associated to our observation. Interestingly, we found that the occurrence of OCBs was significantly higher in patients carrying ALS-associated mutations than in the remaining cohort (3/12, 25 % vs 6/247, 2.4 %; p < 0.01; Fisher’s exact test).
In particular, this association was stronger for the TARDBP p.A382T mutation, which was found in 2/9 (22.2 %) of patients with OCBs compared to 1/250 (0.4 %) in the remaining cohort (p < 0.01). The p.A382T variant is the most common TARDBP mutation identified in ALS patients, especially in countries of the Mediterranean basin [7, 21]. The mutation has a very low penetrance, having been identified in an exceeding number of apparently sporadic patients and in about one-third of all ALS patients of Sardinian descent [5, 32]. It has been reported that individuals carrying this particular variant may display parkinsonian features or dementia, and up to 2.5 % of patients with idiopathic Parkinson’s disease from Sardinia also harbor this mutation [35]. Our description of an ALS patient presenting with prominent cerebellar involvement thus broadens the spectrum of the extramotoneuronal involvement associated with the TARDBP p.A382T mutation. Interestingly, a recent neuropathological report has shown the presence of cerebellar p62-positive inclusions in a proportion (26 %) of patients affected by TDP-43 proteinopathies (ALS, frontotemporal lobar degeneration or both) [22], although the possible correlation between such inclusions with clinical manifestations remains to be determined.
Although our results seem to suggest an association between TARDBP variants and intrathecal synthesis of IgG, it is not clear whether and how such mutations are responsible for the BBB damage and local immune response, since TDP-43 is not known to be directly involved in either of these processes. A recent study, however, showed the presence of TDP43-immunoreactive aggregates adjacent to or within the capillary basal lamina of small brain vessels in patients with frontotemporal lobar degeneration [28]. It is thus possible that intrathecal IgG synthesis in our patients may be consequent to the deposition of mutant TDP43 protein in astrocytic end-feet, loss of BBB integrity, and penetration of immunocompetent cells into the CNS. We speculate that a mutant gene dose effect may be responsible for the development of subcortical WMLs and the more severe phenotype in the individual carrying the homozygous p.A382T mutation compared to the other patient with the same mutation in heterozygous state.
It must be observed that we could not prove with certainty that Patient A399 had a concurrent demyelinating disease of the CNS, since temporal dissemination of inflammatory lesions was not demonstrated, and the observed WMLs could be nonspecific, being limited in number and without gadolinium contrast enhancement. Several observations, however, suggest a possible demyelinating nature these lesions. Firstly, age-associated nonspecific WMLs are rare in individuals younger than 50 years [27]. Moreover, Patient A399 did not present any feature commonly associated with WMLs, such as cardiovascular risk factors, systemic vasculitis and/or migraine. Lastly, WMLs were observed more frequently in individuals with OCBs compared to the remaining ALS patients (66.7 vs 15.2 %), indicating a strong association with intrathecal IgG syntesis. The concurrence of ALS and a demyelinating disease of the CNS of multiple sclerosis-type in the same patient is in fact an extremely rare event, having been previously reported in only four cases, none of which were tested for TARDBP mutations [6, 10, 17, 26].
Conversely to TARDBP, several genes involved in angiogenesis have been implicated in maintaining the integrity of the BBB. Increased expression of VEGF in response to hypoxia contributes to the disruption of the BBB and vascular leakage in the ischemic brain [44]. Moreover, the VEGF-mediated breakdown of the BBB was shown to result in the contact of sequestered CNS antigens with systemic immunocompetent cells, leading to neuroinflammatory processes [34]. Angiogenin, the principal downstream effector of VEGF, may also play a role in maintaining the BBB integrity. A recent report suggested a CNS-specific dysregulation of ANG expression in ALS [29], and a lack of up-regulation of both ANG and VEGF in hypoxaemic conditions has been observed in the CSF of ALS patients compared to controls [30]. The ANG p.P-4S variant, observed in Patient A46, has been found in individuals with ALS, idiopathic Parkinson’s disease and controls, albeit with a reduced frequency in the latter group [42]. The mutation leads to the substitution of a partially conserved proline with a serine in the signal peptide, possibly altering the correct maturation, subcellular localization, and/or secretion of the mature protein. Altered levels of angiogenin in patient A46’s CNS may thus be responsible of the damage to the BBB, as expressed by the increased QAlb, leading in turn to neuroinflammation and intrathecal IgG synthesis.
In conclusion, our results provide evidence that genetic defects are frequent in ALS patients with OCBs and that genetic determinants may play a role in immune processes in these patients. Recent reports suggest that the distinction between familial and sporadic ALS may be artificial and in fact, disease-associated mutations are often observed in apparently sporadic individuals [1]. Since genetic screening of every SALS patient is not usually feasible in a clinical setting, the identification of phenotypically distinct subgroups with a higher mutational frequency may assist clinicians when asking for specific genetic testing and during counseling. Our data suggest that the incidence of mutations of TARDBP and ANG gene is ten times higher among individuals with OCBs in the CSF compared to the remaining ALS patients. As such, we believe that disease-associated mutations in these two genes should be actively looked for in all patients with evidence of BBB dysfunction and/or intrathecal IgG synthesis. The possible role of mutant TDP-43 and angiogenin proteins in these processes warrants further investigation.
References
Al-Chalabi A, Lewis CM (2011) Modelling the effects of penetrance and family size on rates of sporadic and familial disease. Hum Hered 71:281–288
Apostolski S, Nikolic J, Bugarski-Prokopljevic C, Miletic V, Pavlovic S, Filipovic S (1991) Serum and CSF immunological findings in ALS. Acta Neurol Scand 83:96–98
Baumer D, Hilton D, Paine SM, Turner MR, Lowe J, Talbot K, Ansorge O (2010) Juvenile ALS with basophilic inclusions is a FUS proteinopathy with FUS mutations. Neurology 75:611–618
Byrne S, Bede P, Elamin M, Kenna K, Lynch C, McLaughlin R, Hardiman O (2011) Proposed criteria for familial amyotrophic lateral sclerosis. Amyotroph Lateral Scler 12:157–159
Chio A, Borghero G, Pugliatti M, Ticca A, Calvo A, Moglia C, Mutani R, Brunetti M, Ossola I, Marrosu MG, Murru MR, Floris G, Cannas A, Parish LD, Cossu P, Abramzon Y, Johnson JO, Nalls MA, Arepalli S, Chong S, Hernandez DG, Traynor BJ, Restagno G (2012) Large proportion of amyotrophic lateral sclerosis cases in Sardinia due to a single founder mutation of the TARDBP gene. Arch Neurol 68:594–598
Confavreux C, Moreau T, Jouvet A, Tommasi M, Aimard G (1993) Association of amyotrophic lateral sclerosis and multiple sclerosis. Rev Neurol (Paris) 149:351–353
Corrado L, Ratti A, Gellera C, Buratti E, Castellotti B, Carlomagno Y, Ticozzi N, Mazzini L, Testa L, Taroni F, Baralle FE, Silani V, D’Alfonso S (2009) High frequency of TARDBP gene mutations in Italian patients with amyotrophic lateral sclerosis. Hum Mutat 30:688–694
Dejesus-Hernandez M, Mackenzie IR, Boeve BF, Boxer AL, Baker M, Rutherford NJ, Nicholson AM, Finch NA, Flynn H, Adamson J, Kouri N, Wojtas A, Sengdy P, Hsiung GY, Karydas A, Seeley WW, Josephs KA, Coppola G, Geschwind DH, Wszolek ZK, Feldman H, Knopman DS, Petersen RC, Miller BL, Dickson DW, Boylan KB, Graff-Radford NR, Rademakers R (2011) Expanded GGGGCC Hexanucleotide Repeat in Noncoding Region of C9ORF72 Causes Chromosome 9p-Linked FTD and ALS. Neuron 72:245–256
Del Bo R, Tiloca C, Pensato V, Corrado L, Ratti A, Ticozzi N, Corti S, Castellotti B, Mazzini L, Soraru G, Cereda C, D’Alfonso S, Gellera C, Comi GP, Silani V (2011) Novel optineurin mutations in patients with familial and sporadic amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 82(11):1239–1243
Dynes GJ, Schwimer CJ, Staugaitis SM, Doyle JJ, Hays AP, Mitsumoto H (2000) Amyotrophic lateral sclerosis with multiple sclerosis: a clinical and pathological report. Amyotroph Lateral Scler Other Motor Neuron Disord 1:349–353
Engelhardt JI, Tajti J, Appel SH (1993) Lymphocytic infiltrates in the spinal cord in amyotrophic lateral sclerosis. Arch Neurol 50:30–36
Freedman MS, Thompson EJ, Deisenhammer F, Giovannoni G, Grimsley G, Keir G, Ohman S, Racke MK, Sharief M, Sindic CJ, Sellebjerg F, Tourtellotte WW (2005) Recommended standard of cerebrospinal fluid analysis in the diagnosis of multiple sclerosis: a consensus statement. Arch Neurol 62:865–870
Garbuzova-Davis S, Rodrigues MC, Hernandez-Ontiveros DG, Louis MK, Willing AE, Borlongan CV, Sanberg PR (2011) Amyotrophic lateral sclerosis: a neurovascular disease. Brain Res 1398:113–125
Garbuzova-Davis S, Saporta S, Haller E, Kolomey I, Bennett SP, Potter H, Sanberg PR (2007) Evidence of compromised blood–spinal cord barrier in early and late symptomatic SOD1 mice modeling ALS. PLoS One 2:e1205
Gellera C, Castellotti B, Riggio MC, Silani V, Morandi L, Testa D, Casali C, Taroni F, Di Donato S, Zeviani M, Mariotti C (2001) Superoxide dismutase gene mutations in Italian patients with familial and sporadic amyotrophic lateral sclerosis: identification of three novel missense mutations. Neuromuscul Disord 11:404–410
Gellera C, Colombrita C, Ticozzi N, Castellotti B, Bragato C, Ratti A, Taroni F, Silani V (2008) Identification of new ANG gene mutations in a large cohort of Italian patients with amyotrophic lateral sclerosis. Neurogenetics 9:33–40
Hader WJ, Rpzdilsky B, Nair CP (1986) The concurrence of multiple sclerosis and amyotrophic lateral sclerosis. Can J Neurol Sci 13:66–69
Henkel JS, Engelhardt JI, Siklos L, Simpson EP, Kim SH, Pan T, Goodman JC, Siddique T, Beers DR, Appel SH (2004) Presence of dendritic cells, MCP-1, and activated microglia/macrophages in amyotrophic lateral sclerosis spinal cord tissue. Ann Neurol 55:221–235
Hortobagyi T, Troakes C, Nishimura AL, Vance C, van Swieten JC, Seelaar H, King A, Al-Sarraj S, Rogelj B, Shaw CE (2011) Optineurin inclusions occur in a minority of TDP-43 positive ALS and FTLD-TDP cases and are rarely observed in other neurodegenerative disorders. Acta Neuropathol 121:519–527
Jesse S, Brettschneider J, Sussmuth SD, Landwehrmeyer BG, von Arnim CA, Ludolph AC, Tumani H, Otto M (2011) Summary of cerebrospinal fluid routine parameters in neurodegenerative diseases. J Neurol 258:1034–1041
Kabashi E, Valdmanis PN, Dion P, Spiegelman D, McConkey BJ, Vande Velde C, Bouchard JP, Lacomblez L, Pochigaeva K, Salachas F, Pradat PF, Camu W, Meininger V, Dupre N, Rouleau GA (2008) TARDBP mutations in individuals with sporadic and familial amyotrophic lateral sclerosis. Nat Genet 40:572–574
King A, Maekawa S, Bodi I, Troakes C, Al-Sarraj S (2011) Ubiquitinated, p62 immunopositive cerebellar cortical neuronal inclusions are evident across the spectrum of TDP-43 proteinopathies but are only rarely additionally immunopositive for phosphorylation-dependent TDP-43. Neuropathology 31:239–249
Kwong LK, Neumann M, Sampathu DM, Lee VM, Trojanowski JQ (2007) TDP-43 proteinopathy: the neuropathology underlying major forms of sporadic and familial frontotemporal lobar degeneration and motor neuron disease. Acta Neuropathol 114:63–70
Lambrechts D, Storkebaum E, Morimoto M, Del-Favero J, Desmet F, Marklund SL, Wyns S, Thijs V, Andersson J, van Marion I, Al-Chalabi A, Bornes S, Musson R, Hansen V, Beckman L, Adolfsson R, Pall HS, Prats H, Vermeire S, Rutgeerts P, Katayama S, Awata T, Leigh N, Lang-Lazdunski L, Dewerchin M, Shaw C, Moons L, Vlietinck R, Morrison KE, Robberecht W, Van Broeckhoven C, Collen D, Andersen PM, Carmeliet P (2003) VEGF is a modifier of amyotrophic lateral sclerosis in mice and humans and protects motoneurons against ischemic death. Nat Genet 34:383–394
Leonardi A, Abbruzzese G, Arata L, Cocito L, Vische M (1984) Cerebrospinal fluid (CSF) findings in amyotrophic lateral sclerosis. J Neurol 231:75–78
Li G, Esiri MM, Ansorge O, Deluca GC (2012) Concurrent multiple sclerosis and amyotrophic lateral sclerosis: where inflammation and neurodegeneration meet? J Neuroinflamm 9:20
Liao D, Cooper L, Cai J, Toole J, Bryan N, Burke G, Shahar E, Nieto J, Mosley T, Heiss G (1997) The prevalence and severity of white matter lesions, their relationship with age, ethnicity, gender, and cardiovascular disease risk factors: the ARIC Study. Neuroepidemiology 16:149–162
Lin WL, Castanedes-Casey M, Dickson DW (2009) Transactivation response DNA-binding protein 43 microvasculopathy in frontotemporal degeneration and familial Lewy body disease. J Neuropathol Exp Neurol 68:1167–1176
McLaughlin RL, Phukan J, McCormack W, Lynch DS, Greenway M, Cronin S, Saunders J, Slowik A, Tomik B, Andersen PM, Bradley DG, Jakeman P, Hardiman O (2010) Angiogenin levels and ANG genotypes: dysregulation in amyotrophic lateral sclerosis. PLoS One 5:e15402
Moreau C, Gosset P, Brunaud-Danel V, Lassalle P, Degonne B, Destee A, Defebvre L, Devos D (2009) CSF profiles of angiogenic and inflammatory factors depend on the respiratory status of ALS patients. Amyotroph Lateral Scler 10:175–181
Nicaise C, Mitrecic D, Demetter P, De Decker R, Authelet M, Boom A, Pochet R (2009) Impaired blood-brain and blood–spinal cord barriers in mutant SOD1-linked ALS rat. Brain Res 1301:152–162
Orru S, Manolakos E, Orru N, Kokotas H, Mascia V, Carcassi C, Petersen M (2011) High frequency of the TARDBP p.Ala382Thr mutation in Sardinian patients with amyotrophic lateral sclerosis. Clin Genet 81:172–178
Papadimitriou D, Le Verche V, Jacquier A, Ikiz B, Przedborski S, Re DB (2010) Inflammation in ALS and SMA: sorting out the good from the evil. Neurobiol Dis 37:493–502
Proescholdt MA, Heiss JD, Walbridge S, Muhlhauser J, Capogrossi MC, Oldfield EH, Merrill MJ (1999) Vascular endothelial growth factor (VEGF) modulates vascular permeability and inflammation in rat brain. J Neuropathol Exp Neurol 58:613–627
Quadri M, Cossu G, Saddi V, Simons EJ, Murgia D, Melis M, Ticca A, Oostra BA, Bonifati V (2011) Broadening the phenotype of TARDBP mutations: the TARDBP Ala382Thr mutation and Parkinson’s disease in Sardinia. Neurogenetics 12(3):203–209
Renton AE, Majounie E, Waite A, Simon-Sanchez J, Rollinson S, Gibbs JR, Schymick JC, Laaksovirta H, van Swieten JC, Myllykangas L, Kalimo H, Paetau A, Abramzon Y, Remes AM, Kaganovich A, Scholz SW, Duckworth J, Ding J, Harmer DW, Hernandez DG, Johnson JO, Mok K, Ryten M, Trabzuni D, Guerreiro RJ, Orrell RW, Neal J, Murray A, Pearson J, Jansen IE, Sondervan D, Seelaar H, Blake D, Young K, Halliwell N, Callister JB, Toulson G, Richardson A, Gerhard A, Snowden J, Mann D, Neary D, Nalls MA, Peuralinna T, Jansson L, Isoviita VM, Kaivorinne AL, Holtta-Vuori M, Ikonen E, Sulkava R, Benatar M, Wuu J, Chio A, Restagno G, Borghero G, Sabatelli M, Heckerman D, Rogaeva E, Zinman L, Rothstein JD, Sendtner M, Drepper C, Eichler EE, Alkan C, Abdullaev Z, Pack SD, Dutra A, Pak E, Hardy J, Singleton A, Williams NM, Heutink P, Pickering-Brown S, Morris HR, Tienari PJ, Traynor BJ (2011) A Hexanucleotide Repeat Expansion in C9ORF72 Is the Cause of Chromosome 9p21-Linked ALS-FTD. Neuron 72:257–268
Sussmuth SD, Sperfeld AD, Ludolph AC, Tumani H (2010) Hypercapnia is a possible determinant of the function of the blood-cerebrospinal fluid barrier in amyotrophic lateral sclerosis. Neurochem Res 35:1071–1074
Thanabalasundaram G, Pieper C, Lischper M, Galla HJ (2010) Regulation of the blood-brain barrier integrity by pericytes via matrix metalloproteinases mediated activation of vascular endothelial growth factor in vitro. Brain Res 1347:1–10
Ticozzi N, Silani V, LeClerc AL, Keagle P, Gellera C, Ratti A, Taroni F, Kwiatkowski TJ Jr, McKenna-Yasek DM, Sapp PC, Brown RH Jr, Landers JE (2009) Analysis of FUS gene mutation in familial amyotrophic lateral sclerosis within an Italian cohort. Neurology 73:1180–1185
Ticozzi N, Tiloca C, Morelli C, Colombrita C, Poletti B, Doretti A, Maderna L, Messina S, Ratti A, Silani V (2011) Genetics of familial Amyotrophic lateral sclerosis. Arch Ital Biol 149:65–82
Turner MR, Cagnin A, Turkheimer FE, Miller CC, Shaw CE, Brooks DJ, Leigh PN, Banati RB (2004) Evidence of widespread cerebral microglial activation in amyotrophic lateral sclerosis: an [11C](R)-PK11195 positron emission tomography study. Neurobiol Dis 15:601–609
van Es MA, Schelhaas HJ, van Vught PW, Ticozzi N, Andersen PM, Groen EJ, Schulte C, Blauw HM, Koppers M, Diekstra FP, Fumoto K, Leclerc AL, Keagle P, Bloem BR, Scheffer H, van Nuenen BF, van Blitterswijk M, van Rheenen W, Wills AM, Lowe PP, Hu GF, Yu W, Kishikawa H, Wu D, Folkerth RD, Mariani C, Goldwurm S, Pezzoli G, Van Damme P, Lemmens R, Dahlberg C, Birve A, Fernandez-Santiago R, Waibel S, Klein C, Weber M, van der Kooi AJ, de Visser M, Verbaan D, van Hilten JJ, Heutink P, Hennekam EA, Cuppen E, Berg D, Brown RH Jr, Silani V, Gasser T, Ludolph AC, Robberecht W, Ophoff RA, Veldink JH, Pasterkamp RJ, de Bakker PI, Landers JE, van de Warrenburg BP, van den Berg LH (2011) Angiogenin variants in Parkinson disease and amyotrophic lateral sclerosis. Ann Neurol 70:964–973
Younger DS, Rowland LP, Latov N, Sherman W, Pesce M, Lange DJ, Trojaborg W, Miller JR, Lovelace RE, Hays AP et al (1990) Motor neuron disease and amyotrophic lateral sclerosis: relation of high CSF protein content to paraproteinemia and clinical syndromes. Neurology 40:595–599
Zhang ZG, Zhang L, Jiang Q, Zhang R, Davies K, Powers C, Bruggen N, Chopp M (2000) VEGF enhances angiogenesis and promotes blood-brain barrier leakage in the ischemic brain. J Clin Invest 106:829–838
Acknowledgments
A special thank to the Italian ALS patients and their caregivers. Generous support was provided by the Italian Ministry of Health (Malattie Neurodegenerative, ex Art.56, n.533F/N1) and by AriSLA—Agenzia Italiana per la Ricerca sulla Sclerosi Laterale Amiotrofica (grant EXOMEFALS 2009, co-financed with the support of “5 × 1000” —Healthcare Research of the Ministry of Health).
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
N. Ticozzi and C. Tiloca contributed equally to this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ticozzi, N., Tiloca, C., Mencacci, N.E. et al. Oligoclonal bands in the cerebrospinal fluid of amyotrophic lateral sclerosis patients with disease-associated mutations. J Neurol 260, 85–92 (2013). https://doi.org/10.1007/s00415-012-6589-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-012-6589-0