Abstract
Background
Sarcoidosis patients suffer from fatigue and exercise limitation. The aim of this study was to establish whether a physical training program improves these and other outcomes important to sarcoidosis patients.
Methods
From 11/2012 to 9/2014, 201 sarcoidosis patients were referred to the ild care expertise team, Ede, the Netherlands. In our center, all patients are routinely recommended to undergo testing at baseline to determine their physical functioning and encouraged to complete a 12-week, supervised physical training program. Ninety patients underwent baseline testing and returned for repeat testing at 3 months in the interim, 49 completed the training program (Group I) and 41 chose not to participate (Group II). Change over time (from baseline to 3 months) in fatigue, exercise capacity, and skeletal muscle strength were assessed between the two groups.
Results
At baseline, there were no between-group differences for fatigue, DLCO %, FVC %, or exercise capacity [assessed by percent predicted six-minute walk distance (6MWD %) and Steep Ramp Test (SRT)]. The 6MWD for Group I improved between baseline and 3 months, while the 6MWD remained the same in Group II (F = 72.2, p < 0.001). Group I showed a significantly larger decrease of fatigue compared with Group II (F = 6.27, p = 0.014). Lung function tests did not change in either group.
Conclusion
A supervised physical training program improves exercise capacity and fatigue among sarcoidosis patients and should be included in their management regimen.
Similar content being viewed by others
Introduction
Sarcoidosis is a multisystem disorder of unknown cause(s) characterized by the formation of immune granulomas in involved organs, most often the lung and lymphatic system (but virtually any organ can be affected). The clinical presentation of sarcoidosis is highly variable: certain patients present acutely, with severe symptoms and/or multi-organ involvement; although some patients are entirely asymptomatic. Symptoms are generally nonspecific and include general weakness, arthralgias, reduced exercise capacity, dyspnea, and fatigue [1–5]. In addition to the specific organ-related symptoms, these less specific disabling symptoms may have a major influence on the daily activities and the social and professional lives of the patients, resulting in a reduced quality of life (QOL) [6]. Distance covered during the six-minute walk test (6MWD) is often reduced and correlates with forced vital capacity (FVC) and fatigue severity [7, 8]. Fatigue may be explained by peripheral muscle weakness and exercise intolerance—each is influenced by multiple factors, including sarcoidosis-related skeletal muscle abnormalities, decreased pulmonary function, small fiber neuropathy, and deconditioning [9–11].
In several chronic—including lung—diseases, physical training has been shown to improve exercise intolerance and peripheral muscle weakness [12, 13]. Limited data suggest that pulmonary rehabilitation—the backbone of which is an exercise program that most often includes a combination of aerobic and resistance training—or an exercise training program that runs outside the confines of a formal pulmonary rehabilitation program is a safe intervention [14–17] that improves symptoms, physical functioning, and QoL in these patients [12, 14]. Recently, Marcellis and colleagues observed that in sarcoidosis patients, fatigue, physical functioning, and psychological health all improved in response to physical training [13]. Our group showed that a 12-week physical training program improved or maintained exercise capacity in patients with severe fibrotic sarcoidosis or progressive idiopathic pulmonary fibrosis [18].
The aim of this study was to examine whether a physical training program supervised by a physical therapist improves fatigue and exercise capacity in sarcoidosis patients.
Material and Methods
Study Design and Subjects
In this retrospective observational study, outcomes were compared between sarcoidosis patients who completed an exercise training program and those who did not. Patients were included in the cohort if they were evaluated by the ild care expertise team of Hospital Gelderse Vallei, Ede, the Netherlands from 11/2012 to 9/2014 and underwent testing at baseline and 3 months later at the department of physical therapy. The diagnosis of sarcoidosis was confirmed by the multidisciplinary ild care expertise team in accordance with accepted guidelines [1].
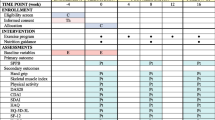
Of the 201 patients evaluated 147 underwent the standard baseline testing; 54 did not complete the baseline testing for various reasons (no reason given, no combined appointment possible along with travel distance, etc.). Of these 147 patients, 90 underwent baseline testing and returned for repeat testing at 3 months. Finally, 49 out of 90 patients completed the training program (Group I) and 41 chose not to participate (Group II) (see also Fig. 1). Fatigue, exercise capacity and skeletal muscle strength were measured in all 90 patients by the same tester.
During the study period, data of 201 out patients suffering from sarcoidosis were collected. At baseline, the majority of these patients (n = 147) completed a physical assessment and surveys at the department of physical therapy. These patients received a tailored advice and were encouraged to start a 12-week physical training program supervised by a physical therapist in accordance with their physical performance assessed at baseline. In 90 patients, a second physical assessment after a 3-month period follow-up was achieved. Between-group evaluation of patients who completed a supervised physical training (n = 49) and those who decided not to follow a physical training program (n = 41)
Outcome Variables
Body Composition
Height, weight, and body mass index (BMI) were measured as reported previously [19].
Lung Function Tests
FVC and forced expiratory volume in one second (FEV1) were measured with a pneumotachograph (Masterlab, Jaeger, Würzburg, Germany). The diffusing capacity of the lung for carbon monoxide (DLCO) was measured using the single-breath method (Masterlab, Jaeger, Würzburg, Germany). Values were expressed as percentage of the predicted value (i.e., FVC %, FEV1 %, and DLCO %, respectively).
Muscle Strength
The maximal isometric grip strength of the dominant hand was measured with the Jamar dynamometer (Fabrication Enterprises Inc., Irvington, NY, USA) and expressed in kilograms (kg) [20]. Percentage of predicted value was calculated using normative data of Mathiowetz and colleagues [21]. Biceps brachii strength was assessed during elbow flexion with the microFET (Biometrics, Almere, The Netherlands), an electronic hand-held dynamometer. The ‘break’ method was used to measure the maximal peak force of the dominant arm in Newton (N). The highest value of at least two measurements was recorded [22].
Exercise Capacity
Maximal oxygen uptake—and other commonly collected variables—were measured during a cardiopulmonary exercise test using the Steep Ramp Test (SRT) protocol on a cycle ergometer. The protocol as described by Meyer et al. was used [23]. Outcome of the SRT was used to determine estimated VO2max value according to DeBacker and coworkers [24]. Reference values determined by McArdle et al. were used to classify obtained values [25]. Maximal oxygen uptake was defined as reduced when values were classified ‘very poor’ and ‘poor’ according to McArdle. The six-minute walk test (6MWT) was administered according to the American Thoracic Society Guidelines [26]. Predicted 6MWD values were calculated according to Gibson and colleagues [27].
Questionnaires
Fatigue was measured with the 10-item Fatigue Assessment Scale (FAS). Each item uses a 5-point rating scale, so the total score range is 10–50. Scores below 22 indicate no fatigue; scores of 22–34 indicate mild–moderate fatigue; and scores of 35 or more indicate extreme fatigue. In sarcoidosis, the FAS has acceptable psychometric properties [28]. The minimal clinically important difference in sarcoidosis is 4 points or a 10% change [29].
The Borg Rating of Perceived Exertion (RPE) Scale was used to assess perceived exertion during the 6MWT. Scores range from 6 to 20, where 6 means “no exertion at all” and 20 means “maximal exertion.” Average breathlessness intensity over a 2-week period was assessed with an 8-point, modified Borg scale (from 0 to 7), for which higher scores indicate greater breathlessness [30]. Patients also ticked a box to indicate whether their breathlessness was brief, periodic, or continuous.
Intervention
Patients were encouraged to start a 12-week physical training program supervised by a physical therapist in accordance with their physical performance assessed at baseline. In accordance with the American Thoracic Society standards, the exercise program contained two major components: aerobic endurance training (stationary cycling, treadmill) and peripheral muscle strengthening (upper and lower body) [12]. A physical therapist supervised the training program which consisted of twice-weekly 60 minute sessions that included both components.
The aerobic endurance component was started at a level of 50–60 % of peak work achieved during the SRT [23]. An interval protocol was used while subjects exercised continuously with a goal time of more than 30 min. After a 10 min warm-up period, subjects completed alternating exercise intervals of 40 s at high resistance and 60 s at low resistance. After completing ten intervals, subjects cooled down for 5 min. Intensity and duration were gradually increased (both within sessions and over time) to build tolerance and confidence. During each session, the targeted exercise intensity was 13–15 on the Borg RPE Scale [31]. Pulse oxymetry was used to monitor peripheral oxygen saturation levels during exercise, and supplemental oxygen use during training was commensurate with current prescriptions.
The strength training component consisted of exercises using Life Fitness Circuit Series equipment (Life Fitness, Barendrecht, the Netherlands). During each training sessions, subjects performed three sets of 15–20 repetitions of 6–8 different exercises—some lower and some upper body. At least two lower-body exercises were performed each training session. The resistance level was individualized for each patient (according to patient preference) and reassessed and adjusted after every session using the Borg Score. The targeted exercise intensity was between 13 and 15 on the Borg score [31].
Statistical Analysis
Descriptive statistics were generated for baseline characteristics. To examine differences between the two patient groups who participated in this study at baseline, independent sample t tests (Mann–Whitney U tests) or Chi-square (or Fisher’s exact) tests were performed depending on the type of variables and normality of data. Analyses of variance for repeated measures were performed to examine whether the effect of the training on fatigue, the MWD, and perceived exertion, taking (if necessary) variables on which the two patient groups differed at baseline into account. Furthermore, a Chi-square test was performed to examine the difference between groups concerning the MCID of fatigue. We considered p < 0.05 to represent statistical significance. All statistical analyses were performed using SPSS statistical software (version 19.0 for Windows) (SPSS Inc., Chicago, IL, USA).
Results
Baseline characteristics for the 147 patients with evaluable data—including the 90 patients who returned at 3 months—are summarized in Table 1. Figure 1 displays the flow chart of the study.
At baseline, there were no between-group differences in demographic or clinical variables (e.g., pulmonary function tests, inflammatory markers, radiological findings, peripheral muscle strength or exercise capacity, or treatment (Tables 1, 2)). There were also no between-group differences with regard to fatigue and perceived exertion.
Concerning fatigue, we found an interaction effect of time with group (F = 6.27, p = 0.014). This indicates that while both groups started with the same level of fatigue, Group I showed a significantly larger decrease of fatigue compared with Group II (see Fig. 2). The change in fatigue was also found when looking at the cut-off scores. At baseline, the majority of patients were fatigued. At 3 months, FAS scores improved by 4 or more points (i.e., the minimal clinically important difference or MCID) in 74.4 % of the patients in Group I and 48.5% of patients in Group II (p = 0.032). Lung function tests did not change in either group (data not shown).
An interaction effect was also found with regard to the 6MWD % norm (F = 59.5, p < 0.001). The 6MWD % norm for Group I improved between baseline and 3 months, while the 6MWD remained the same in Group II. As shown in Fig. 3, similar results were found with regard to 6MWD distance (interaction effect: F = 72.2, p < 0.001).
Concerning EFMS, % predicted, no significant interaction effect (p = 0.129) was found. There is a significant increase across time in both groups (F = 9.25, p = 0.003) but no difference between the two groups (p = 0.907). For HGS % norm, no significant interaction effect (p = 0.933) was present, but we did find that the % decreased significantly across time (F = 446.5, p < 0.001) in both groups. No group difference was found.
With regard to the two types of Borg scores, the Modified Borg and the Borg RPE, no difference was found between the groups and across time.
We did find an interaction effect on the two SRT measures, SRT watts (F = 4.6, p = 0.034) and SRT VO2 max, ml/kg/min (F = 6.3, p = 0.014), indicating different changes across time for both groups. Although the main effects for both measures showed that the difference between the groups was not significant.
Discussion
In this study, we observed that a supervised, 12-week, aerobic exercise, and strength training program improves exercise performance, strength, and fatigue in patients with sarcoidosis. The results were independent of age, gender, time since diagnosis, baseline pulmonary function (and other markers of sarcoidosis severity), inflammatory status, or pharmacological interventions. Currently, a program like the one used at our center is not standard of care for patients with sarcoidosis, but we think it should be. The exercise program is similar to those used in pulmonary rehabilitation programs throughout the world; thus, most clinicians caring for sarcoidosis patients have access to this valuable adjunctive therapeutic modality. In fact, we would argue that pulmonary rehabilitation should be considered as a first-line therapy for patients suffering from sarcoidosis.
Patients with sarcoidosis are frequently limited by reduced exercise tolerance, muscle weakness, and impaired QOL [7, 32, 33]. Sarcoidosis imposes a burden on patient’s lives and fatigue is ubiquitous among sarcoidosis patients. Exercise programs and pulmonary rehabilitation are beneficial for patients with many respiratory diseases [12], and evidence on the benefits of pulmonary rehabilitation (PR) and exercise for sarcoidosis patients is increasing [13, 18, 34–36]. Our study builds on the results of a study by Marcellis et al. who observed that fatigue declined and 6MWD and peripheral muscle strength improved after a 13-week physical training program in sarcoidosis patients [13]. Ryerson and his colleagues found that PR improved exercise capacity in interstitial lung disease (ILD) patients, regardless of baseline 6MWD, and patients with worse baseline functional capacity had greater improvements following PR [37]. This suggests that motivated patients with relatively severe functional impairment should still be offered PR (unless contraindications exist), because they stand to benefit most.
At baseline, we found strong—but far from perfect—correlations between SRT and both VO2max and 6MWD. This suggests that the SRT (submaximal exercise test, cycling, not every-day activity in all patients) and 6MWD (submaximal exercise test, walking, every-day activity) assess different aspects of physical functioning. Regardless, the between-groups differences in both variables were significantly greater in the group completing the intervention. Because there is lack of clarity [38], future studies are needed to address the issue of which exercise modality (cycle ergometry, walking, or both) should be used to assess the effects of interventions aimed at improving physical functional capacity.
Sarcoidosis is a heterogeneous disease, making assessments of disease severity complex. For example, pulmonary function test may not reflect the severity of pulmonary sarcoidosis [39]; thus, incorporating metrics across a broad range of outcomes is needed to generate a comprehensive determination of sarcoidosis severity. This is likely best performed via a multidisciplinary approach [5] that incorporates the assessment of multiple domains of physical functioning—and because it is so common and intrusive—fatigue [7, 40]. Patients with any chronic illness are at risk for physical inactivity, which in turn can induce general deconditioning. Poor physical conditioning contributes to fatigue, dyspnea, and the vicious cycle of more physical inactivity [10, 15]. Our results suggest that physical therapy and exercise are capable of breaking this cycle. Given the complexity of sarcoidosis and the potential for multi-system involvement, the therapeutic approach to any one patient, including rehabilitation or physical exercise programs, should be comprehensive, well thought-out and tailored to his/her needs [34, 41–44].
This study has several limitations. First, it was an observational study, lacking a randomized control group, and blinding was not possible. This could introduce bias. Patients who decided to complete the supervised training program were likely more motivated than the other patients to improve their physical performance. Finally, we did not assess the long-term effect of PR. Thus, it is unknown whether these benefits are sustained following a supervised trainings program and which patients experience the greatest benefits.
In conclusion, a supervised physical training program improves fatigue, exercise capacity, and peripheral muscle strength among sarcoidosis patients; these results were independent of age, gender, time since diagnosis, baseline pulmonary function (and other markers of sarcoidosis severity), inflammatory status, or pharmacological interventions. Physical training should be included in their management regimen. Further research is required to confirm which patients benefit most from exercise training (including the type offered in pulmonary rehabilitation programs), to determine which components of such a program are most valuable to patients with sarcoidosis and explore whether there are strategies that can be used to achieve long-term benefits.
References
(1999) Statement on sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med 160(2):736–755
Baughman RP, Culver DA, Judson MA (2011) A concise review of pulmonary sarcoidosis. Am J Respir Crit Care Med 183(5):573–581
Iannuzzi MC, Fontana JR (2011) Sarcoidosis: clinical presentation, immunopathogenesis, and therapeutics. JAMA 305(4):391–399
Valeyre D, Nunes H, Bernaudin JF (2014) Advanced pulmonary sarcoidosis. Curr Opin Pulm Med 20(5):488–495
Valeyre D, Prasse A, Nunes H, Uzunhan Y, Brillet PY, Muller-Quernheim J (2014) Sarcoidosis. Lancet 383(9923):1155–1167
Drent M, Strookappe B, Hoitsma E, De Vries J (2015) Consequences of sarcoidosis. Clin Chest Med (in press)
Marcellis RG, Lenssen AF, Elfferich MD, De Vries J, Kassim S, Foerster K, Drent M (2011) Exercise capacity, muscle strength and fatigue in sarcoidosis. Eur Respir J 38(3):628–634
Spruit MA, Thomeer MJ, Gosselink R, Troosters T, Kasran A, Debrock AJ, Demedts MG, Decramer M (2005) Skeletal muscle weakness in patients with sarcoidosis and its relationship with exercise intolerance and reduced health status. Thorax 60(1):32–38
Marcellis RG, Lenssen AF, de Vries J, Drent M (2013) Reduced muscle strength, exercise intolerance and disabling symptoms in sarcoidosis. Curr Opin Pulm Med 19(5):524–530
Marcellis RGJ, Lenssen AF, Kleynen S, De Vries J, Drent M (2013) Exercise capacity, muscle strength and fatigue in sarcoidosis: a follow-up study. Lung 191(3):247–256
Drent M, Marcellis R, Lenssen A, De Vries J (2014) Association between physical functions and quality of life in sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 31(2):117–128
Spruit MA, Singh SJ, Garvey C et al (2013) An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 188(8):e13–e64
Marcellis RG, Veeke MAF, Mesters I, Drent M, de Bie RA, de Vries GJ, Lenssen AF (2015) Does physical training reduce fatigue in sarcoidosis? Sarcoidosis Vasc Diffuse Lung Dis 32(1):53–62
Spruit MA, Wouters EFM, Gosselink R (2005) Rehabilitation programmes in sarcoidosis: a multidisciplinary approach. Eur Respir Mon 32:316–326
Braam AW, de Haan SN, Vorselaars AD, Rijkers GT, Grutters JC, van den Elshout FJ, Korenromp IH (2013) Influence of repeated maximal exercise testing on biomarkers and fatigue in sarcoidosis. Brain Behav Immun 33:57–64
Holland A, Hill C (2008) Physical training for interstitial lung disease. Cochrane Database Syst Rev 4:CD006322
Swigris JJ, Brown KK, Make BJ, Wamboldt FS (2008) Pulmonary rehabilitation in idiopathic pulmonary fibrosis: a call for continued investigation. Respir Med 102(12):1675–1680
Strookappe B, Elfferich MDP, Swigris JJ, Verschoof AC, Verschakelen JA, Knevel T, Drent M (2015) Benefits of physical training in patients with idiopathic or end-stage sarcoidosis-related pulmonary fibrosis: a pilot study. Sarcoidosis Vasc Diffuse Lung Dis 32(1):43–52
Cremers JP, Drent M, Elfferich MD, Nelemans PJ, Wijnen PA, Witteman BJ, Schols AM (2013) Body composition profiling in a Dutch sarcoidosis population. Sarcoidosis Vasc Diffuse Lung Dis 30(4):289–299
Werle S, Goldhahn J, Drerup S, Simmen BR, Sprott H, Herren DB (2009) Age- and gender-specific normative data of grip and pinch strength in a healthy adult Swiss population. J Hand Surg Eur 34(1):76–84
Mathiowetz V, Wiemer DM, Federman SM (1986) Grip and pinch strength: norms for 6- to 19-year-olds. Am J Occup Ther 40(10):705–711
Bohannon RW (1988) Make tests and break tests of elbow flexor muscle strength. Phys Ther 68(2):193–194
Meyer K, Samek L, Schwaibold M, Westbrook S, Hajric R, Lehmann M, Essfeld D, Roskamm H (1996) Physical responses to different modes of interval exercise in patients with chronic heart failure-application to exercise training. Eur Heart J 17(7):1040–1047
De Backer IC, Schep G, Hoogeveen A, Vreugdenhil G, Kester AD, van Breda E (2007) Exercise testing and training in a cancer rehabilitation program: the advantage of the steep ramp test. Arch Phys Med Rehabil 88(5):610–616
McArdle WD, Katch FI, Katch VL (2007) Exercise physiology: energy, nutrition, & human performance, 7th edn. Lippincott Williams and Wilkins, Baltimore
ATS Commitee (2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166(1):111–117
Gibbons WJ, Fruchter N, Sloan S, Levy RD (2001) Reference values for a multiple repetition 6-minute walk test in healthy adults older than 20 years. J Cardiopulm Rehabil 21(2):87–93
Michielsen HJ, Drent M, Peros-Golubicic T, De Vries J (2006) Fatigue is associated with quality of life in sarcoidosis patients. Chest 130(4):989–994
De Kleijn WP, De Vries J, Wijnen PA, Drent M (2011) Minimal (clinically) important differences for the Fatigue Assessment Scale in sarcoidosis. Respir Med 105(9):1388–1395
Skevington SM, Pilaar M, Routh D, MaCleod RD (1997) On the language of breathlessness. Psychol Health 12:677–689
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14(5):377–381
Marcellis RG, Lenssen AF, Kleynen S, De Vries J, Drent M (2013) Exercise capacity, muscle strength, and fatigue in sarcoidosis: a follow-up study. Lung 191(3):247–256
Marcellis RG, Lenssen AF, de Vries GJ, Baughman RP, van der Grinten CP, Verschakelen JA, De Vries J, Drent M (2013) Is there an added value of cardiopulmonary exercise testing in sarcoidosis patients? Lung 191(1):43–52
Holland AE, Hill CJ, Conron M, Munro P, McDonald CF (2008) Short term improvement in exercise capacity and symptoms following exercise training in interstitial lung disease. Thorax 63(6):549–554
Huppmann P, Sczepanski B, Boensch M, Winterkamp S, Schonheit-Kenn U, Neurohr C, Behr J, Kenn K (2013) Effects of inpatient pulmonary rehabilitation in patients with interstitial lung disease. Eur Respir J 42(2):444–453
Ries AL (2008) Pulmonary rehabilitation: summary of an evidence-based guideline. Respir Care 53(9):1203–1207
Ryerson CJ, Garvey C, Collard HR (2010) Pulmonary rehabilitation for interstitial lung disease. Chest 138(1):240–241 author reply 241–242
Man WD, Soliman MG, Gearing J, Radford SG, Rafferty GF, Gray BJ, Polkey MI, Moxham J (2003) Symptoms and quadriceps fatigability after walking and cycling in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 168(5):562–567
Baughman RP, Lower EE, Gibson K (2012) Pulmonary manifestations of sarcoidosis. Presse Med 41(6 Pt 2):e289–e302
Drent M, Lower EE, De Vries J (2012) Sarcoidosis-associated fatigue. Eur Respir J 40(1):255–263
De Vries J, Drent M (2008) Quality of life and health status in sarcoidosis: a review of the literature. Clin Chest Med 29(3):525–532
Hinz A, Brähler E, Möde R, Wirtz H, Bosse-Henck A (2012) Anxiety and depression in sarcoidosis: the influence of age, gender, affected organs, concomitant diseases and dyspnea. Sarcoidosis Vasc Diffuse Lung Dis 29:139–146
Elfferich MD, Nelemans PJ, Ponds RW, De Vries J, Wijnen PA, Drent M (2010) Everyday cognitive failure in sarcoidosis: the prevalence and the effect of anti-TNF-alpha treatment. Respiration 80(3):212–219
Judson MA (2011) Small fiber neuropathy in sarcoidosis: something beneath the surface. Respir Med 105(1):1–2
Acknowledgements
The authors wish to thank Petal Wijnen for helping preparing the manuscript.
Funding
This study was supported by a research grant of the ild care foundation: www.ildcare.nl. The study sponsor had no involvement in the study design; in the collection, analysis, and interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors who have part in this study declare that they do not have anything to disclose regarding funding or conflict of interest with respect to this manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Strookappe, B., Swigris, J., De Vries, J. et al. Benefits of Physical Training in Sarcoidosis. Lung 193, 701–708 (2015). https://doi.org/10.1007/s00408-015-9784-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-015-9784-9