Abstract
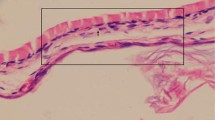
Myringosclerosis is hyalinization and calcification of certain areas of the tympanic membrane, especially the fibrous lamina propria layer and appears as white sclerotic lesions. Ventilation tube insertion is one of the most performed operations in the pediatric otorhinolaryngology practice to treat chronic otitis media with effusion. Myringosclerosis is a very common sequela of ventilation tube insertion. In this experimental study, our aim was to show the histopathological effects of caffeic acid phenethyl ester on myringosclerosis development in rat tympanic membrane after myringotomy. The rats were randomly categorized into four experimental groups including the comparison group (n = 4), non-treated group (n = 7), the saline (control) group (n = 7), the caffeic acid phenethyl ester group (n = 7). Non-treated group did not receive any treatment for 15 days. Saline (2.5 mL/kg, intraperitoneal) was administered to the third group once a day for 15 days. Fourth group received caffeic acid phenethyl ester intraperitoneally once a day at a dose of 10 μmol/kg for 15 days. Myringotomy was performed on the right tympanic membrane of all rats except comparison group using a sterile pick with the help of an operating microscope. Histopathological examination of myringosclerosis formation was done by a pathologist under light microscope. In histopathological analysis of groups, the severity of inflammation was milder in caffeic acid phenethyl ester group compared to non-treated and saline groups (p < 0.05). There was less myringosclerotic plaques in caffeic acid phenethyl ester group than in non-treated and saline groups (p < 0.05). TM thickness measurements were very close to each other in non-treated and saline groups. The tympanic membrane thickness of caffeic acid phenethyl ester group was much thinner than the other two groups (p < 0.05). Caffeic acid phenethyl ester decreases inflammation severity and the formation of myringosclerotic plaques. These two effects resulted in thinner tympanic membranes of rats which were treated with caffeic acid phenethyl ester. As a result, caffeic acid phenethyl ester has potential preventive effects on myringosclerosis development after myringotomy and ventilation tube insertion.




Similar content being viewed by others
References
Albiin N, Hellström S, Salen B, Stenfors LE, Söderberg O (1983) The anatomy of the eustachian tube in the rat: a macro-and microscopical study. Anat Rec 207:513–521
Mattsson C, Marklund SL, Hellström S (1997) Application of oxygen free radical scavengers to diminish the occurrence of myringosclerosis. Ann Otol Rhinol Laryngol 106:513–518
Mattsson C, Stierna P, Hellstrom S (2000) Treatment with dexamethasone arrests the development of myringosclerosis after myringotomy. Am J Otol 21:804–808
Özcan C, Görür K, Cinel L, Talas DU, Unal M, Cinel I (2002) The inhibitory effect of topical N-acetylcysteine application on myringosclerosis in perforated rat tympanic membrane. Int J Pediatr Otorhinolaryngol 63:179–184
Tos M, Bonding P, Paulsen G (1983) Tympanosclerosis of the drum in secretory otitis media after insertion of grommets: a prospective, comparative study. J Laryngol Otol 97:489–496
Mattsson C, Magnuson K, Hellström S (1995) An increased oxygen concentration causes myringosclerosis in traumatized tympanic membranes. Experimental study. Ann Otol Rhinol Laryngol 104:625–632
Uneri C, Sari M, Akboğa J, Yüksel M (2006) Vitamin E-coated tympanostomy tube insertion decreases the quantity of free radicals in tympanic membrane. Laryngoscope 116:140–143
Mattsson C, Hellström S (1997) Inhibition of the development of myringosclerosis by local administration of fenspiride, an anti-inflammatory drug. Eur Arch Otorhinolaryngol 254:425–429
Asiri S, Hasham A, al Anazy F, Zakzouk S, Banyar A (1999) Tympanosclerosis: review of literature and incidence among patients with middle-ear infection. J Laryngol Otol 113:1076–1080
Paparella MM, Schachern P (1994) New developments in treating otitis media. Ann Otol Rhinol Laryngol Suppl 163:7–10
Liao HF, Chen YY, Liu JJ, Hsu ML, Shieh HJ, Liao HJ, Shieh CJ, Shiao MS, Chen YJ (2003) Inhibitory effect of caffeic acid phenethyl ester on angiogenesis, tumor invasion, and metastasis. J Agric Food Chem 51:7907–7912
Gokalp O, Uz E, Cicek E, Yilmaz HR, Ozer MK, Altunbas A, Ozcelik N (2006) Ameliorating role of caffeic acid phenethyl ester (CAPE) against isoniazid-induced oxidative damage in red blood cells. Mol Cell Biochem 290:55–59
Sud’ina GF, Mirzoeva OK, Pushkareva MA, Korshunova GA, Sumbatyan NV, Varfolomeev SD (1993) Caffeic acid phenethyl ester as a lipoxygenase inhibitor with antioxidant properties. FEBS Lett 329:21–24
Institute of Laboratory Animal Research. Commission on Life Sciences. National Research Council (1996) The guide for the care and use of laboratory animals, 7th edn. National Academy of Sciences, Washington, DC
Banerjee T, Kuypers FA (2004) Reactive oxygen species and phosphatidylserine externalization in murine sickle red cells. Br J Haematol 124:392–402
Bhaya MH, Schachern PA, Morizono T, Paparella MM (1993) Pathogenesis of tympanosclerosis. Otolaryngol Head Neck Surg 109:413–420
Spratley JE, Hellström SO, Mattsson CK, Pais-Clemente M (2001) Topical ascorbic acid reduces myringosclerosis in perforated tympanic membranes. A study in rat. Ann Otol Rhinol Laryngol 110:585–591
Song JJ, Kwon SK, Cho CG, Park SW (2007) The effect of caffeic acid phenethyl ester on the prevention of experimentally induced myringosclerosis. Int J Pediatr Otorhinolaryngol 71:1287–1291
Dawes PJ, Bingham BJ, Ryhs R, Griffiths MV (1991) Aspirating middle ear effusions when inserting ventilation tubes: does it influence post-operative otorrhoea, tube obstruction or the development of tympanosclerosis? Clin Otolaryngol Allied Sci 16:457–461
Wielinga EW, Kerr AG (1993) Tympanosclerosis. Clin Otolaryngol Allied Sci 18:341–349
Sade J, Luntz M (1993) Dynamic measurements of gas composition in the middle ear II: steady state value. Acta Otolaryngol 113:353–357
Felding JU, Rasmussen JB, Lildholdt T (1987) Gas composition of the normal and the ventilated middle ear cavity. Scand J Clin Lab Invest Suppl 186:31–41
Mattsson C, Carlsson L, Marklund SL, Hellström S (1997) Myringotomized mice develop myringosclerosis in the pars flaccida and not in the pars tensa. Laryngoscope 107:200–205
Fadillioglu E, Oztas E, Erdogan H, Yagmurca M, Sogut S, Ucar M, Irmak MK (2004) Protective effects of caffeic acid phenethyl ester on doxorubicin-induced cardiotoxicity in rats. J Appl Toxicol 24:47–52
Bakır S, Özbay M, Gün R, Yorgancılar E, Kınış V, Keleş A, Abakay A, Gökalp O, Topçu İ (2013) The protective role of caffeic acid phenethyl ester against streptomycin ototoxicity. Am J Otolaryngol 34:16–21
Irmak MK, Fadillioglu E, Sogut S, Erdogan H, Gulec M, Ozer M, Yagmurca M, Gozukara ME (2003) Effects of caffeic acid phenethyl ester and alpha-tocopherol on reperfusion injury in rat brain. Cell Biochem Funct 21:283–289
Kazikdas KC, Uguz MZ, Erbil G, Tugyan K, Yilmaz O, Guneli E, Altun Z (2006) The antioxidant effect of alpha-tocopherol in the prevention of experimentally induced myringosclerosis. Otol Neurotol 27:882–886
Akbaş Y, Pata YS, Görür K, Polat G, Polat A, Ozcan C, Unal M (2003) Hear Res. The effect of l-carnitine on the prevention of experimentally induced myringosclerosis in rats. Hear Res 184:107–112
Dogan E, Erdag TK, Sarioglu S, Ecevit MC, Ikiz AO, Güneri EA (2011) The preventive effect of N-nitro l-arginine methyl ester in experimentally induced myringosclerosis. Int J Pediatr Otorhinolaryngol 75:1035–1039
Emir H, Kaptan ZK, Samim E, Sungu N, Ceylan K, Ustun H (2009) The preventive effect of ginkgo biloba extract in myringosclerosis: study in rats. Otolaryngol Head Neck Surg 140:171–176
Conflict of interest
We certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kinis, V., Ozbay, M., Alabalik, U. et al. Effect of caffeic acid phenethyl ester on myringosclerosis development in the tympanic membrane of rat. Eur Arch Otorhinolaryngol 272, 29–34 (2015). https://doi.org/10.1007/s00405-013-2832-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-013-2832-2