Abstract
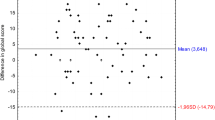
The study was carried out to determine the impact of some co-morbid otological symptoms and demographic factors on the emotional distress and cognitive functioning in patients with tinnitus. One hundred consecutive patients, complaining of constant idiopathic tinnitus, were enrolled into the study. Four tests were administered: Beck Depression Inventory, Hospital Anxiety Depression Scale (HADS, A—anxiety, D—depression), Mini-Mental State Examination (MMSE) and Trail Making Test (TMT). A multivariate stepwise linear regression analysis was performed to estimate the relationship between the results of each of the tests and following co-morbid factors: age, sex, tinnitus duration, tinnitus laterality, hearing status (normal hearing, unilateral hearing loss and bilateral hearing loss) and vertigo/dizziness. It was found that the scores of MMSE and TMT were negatively correlated with age and with hearing status and the scores of HADS-A were slightly correlated with sex. In regression analysis, in HADS-A, sex and to a lesser extent tinnitus duration, in MMSE and TMT age and to a lesser extent tinnitus laterality were the variables that were comprised in the final model. Demographic factors had contributed more than overlapping otological symptoms to the psychological outcome in tinnitus patients.


Similar content being viewed by others
References
Andersson G, Mc Kenna L (1997) Contributions of clinical psychology in audiology: hearing impairment and tinnitus. Clin Psychol Psychother 4:42–50
Halford JBS, Anderson SD (1991) Anxiety and depression in tinnitus sufferers. J Psychosom Res 35:383–390
Stephens SDG, Hallam RS (1985) The Crown–Crisp Experiential Index in patients complaining of tinnitus. Br J Audiol 19:151–158
Collet L, Moussu MF, Disant F, Ahami T, Morgon A (1990) Minnesota Multiphasic Personality Inventory in tinnitus disorders. Audiology 29:101–106
Eriksson-Mangold M, Carlsson SG (1991) Psychological and somatic distress in relation to perceived hearing disability, hearing handicap, and hearing measurements. J Psychosom Res 35:729–740
Monzani D, Casolari L, Guidetti G, Rigatelli M (2007) Psychological distress and disability in patients with vertigo. J Psychosom Res 50:319–333
Hanes DA, McCollum G (2006) Cognitive-vestibular interactions: a review of patient difficulties and possible mechanisms. J Vestib Res 16:75–91
Andersson G, Westin V (2008) Understanding tinnitus distress: introducing the concepts of moderators and mediators. Int J Audiol 47(Suppl 2):S106–S111
Sindhusake D, Golding M, Wigney D, Nevall P, Jakobsen K, Mitchell P (2004) Factors predicting severity of tinnitus: a population-based assessment. J Am Acad Audiol 15:269–280
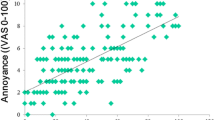
Hiller W, Goebel G (2006) Factors influencing tinnitus loudness and annoyance. Arch Otolaryngol Head Neck Surg 132:1323–1330
Allsup SJ, Gosney MA (2002) Anxiety and depression in an older research population and their impact on clinical outcomes in a randomized controlled trial. Postgrad Med J 78:674–677
Castaneda AE, Tuulio-Henriksson A, Marttunen M, Suvisaari J, Lönnqvist J (2008) A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord 106:1–27
Mirowsky J, Ross CE (1995) Sex differences in distress: real or artifact? Am Sociol Rev 60:449–468
Hallberg LR, Hallberg U, Kramer SE (2008) Self-reported hearing difficulties, communication strategies and psychological general well-being (quality of life) in patients with acquired hearing impairment. Disabil Rehabil 30:203–212
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psych 4:561–571
Lezak MD (1995) Neuropsychological assessment, 3rd edn. Oxford University Press, New York
Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67:361–370
McDowell I (2006) Measuring health: a guide to rating scales and questionnaires. Oxford University Press, New York
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Reitan RM (1958) Validity of the trail making test as an indicator of organic brain damage. Percept Mot Skills 8:271–276
Spreen O, Strauss EA (1998) Compendium of neuropsychological tests: administration, norms, and commentary, 2nd edn. Oxford University Press, New York
Stanik J (1983) Selected diagnostics techniques in clinical psychology. Wydawnictwo Uniwersytetu Śląskiego, Katowice
Darowski ES, Helder E, Zacks RT, Hasher L, Hambrick DZ (2008) Age-related differences in cognition: the role of distraction control. Neuropsychology 22:638–644
Searchfield GD, Morrison-Low J, Wise K (2007) Object identification and attention training for treating tinnitus. Prog Brain Res 166:441–460
Salonen J, Johansson R, Joukamaa M (2007) Alexithymia, depression and tinnitus in elderly patients. Gen Hosp Psych 29:431–435
Dineen R, Doyle J, Bench J (1997) Audiological and psychological characteristics of a group of tinnitus sufferers, prior to tinnitus management training. Br J Audiol 31:27–33
Andersson G, Vretblad P (2000) Anxiety sensitivity in patients with chronic tinnitus. Scand J Behav Ther 29:57–64
Erlandsson SI, Holgers KM (2001) The impact of perceived tinnitus severity on health-related quality of life with aspects of gender. Noise Health 3:39–51
Holgers KM, Juul J (2006) The suffering of tinnitus in childhood and adolescence. Int J Audiol 45:267–272
Erlandsson SI (2000) Psychological profiles of tinnitus patients. In: Tyler RS (ed) Tinnitus handbook. Singular Publishing Group, San Diego, pp 25–58
Stevens C, Walker G, Boyer M, Gallagher M (2007) Severe tinnitus and its effect on selective and divided attention. Int J Audiol 46:208–216
Rutter DR, Stein MJ (1999) Psychological aspects of tinnitus: a comparison with hearing loss and ear, nose and throat disorders. Psychol Health 14:711–718
Ratnayake SA, Jayarajan V, Bartlett J (2009) Could an underlying hearing loss be a significant factor in the handicap caused by tinnitus? Noise Health 11:156–160
Savastano M (2008) Tinnitus with or without hearing loss: are its characteristics different? Eur Arch Otorhinolaryngol 265:1295–1300
Pinto PCL, Sanchez TG, Tomita S (2010) The impact of gender, age and hearing loss on tinnitus severity. Braz J Otorhinolaryngol 76:18–24
Erlandsson SI, Hallberg LRM, Axelsson A (1992) Psychological and audiological correlates of perceived tinnitus severity. Audiology 31:168–179
Langenbach M, Olderog M, Michel O, Albus C, Köhle K (2005) Psychosocial and personality predictors of tinnitus-related distress. Gen Hosp Psych 27:73–77
Erlandsson SI, Hallberg LR (2000) Prediction of quality of life in patients with tinnitus. Br J Audiol 34:11–20
Kirsch CA, Blanchard EB, Parnes SM (1989) Psychological characteristics of individuals high and low in their ability to cope with tinnitus. Psychosom Med 51:209–217
Hallberg LRM, Erlandsson SI (1993) Tinnitus characteristics in tinnitus complainers and noncomplainers. Br J Audiol 27:19–27
Acknowledgments
The work was granted by Medical University of Lodz, grant no. 503/2-036-01/503-01.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pajor, A.M., Ormezowska, E.A. & Jozefowicz-Korczynska, M. The impact of co-morbid factors on the psychological outcome of tinnitus patients. Eur Arch Otorhinolaryngol 270, 881–888 (2013). https://doi.org/10.1007/s00405-012-2079-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-012-2079-3