Abstract
In patients with severe to profound hearing loss, cochlear implants (CIs) are currently the only therapeutic option when the amplification with conventional hearing aids does no longer lead to a useful hearing experience. Despite its great success, there are patients in which benefit from these devices is rather limited. One reason may be a poor neuron-device interaction, where the electric fields generated by the electrode array excite a wide range of tonotopically organized spiral ganglion neurons at the cost of spatial resolution. Coating of CI electrodes to provide a welcoming environment combined with suitable surface chemistry (e.g. with neurotrophic factors) has been suggested to create a closer bioelectrical interface between the electrode array and the target tissue, which might lead to better spatial resolution, better frequency discrimination, and ultimately may improve speech perception in patients. Here we investigate the use of a collagen surface with a cholesteric banding structure, whose orientation can be systemically controlled as a guiding structure for neurite outgrowth. We demonstrate that spiral ganglion neurons survive on collagen-coated surfaces and display a directed neurite growth influenced by the direction of collagen fibril deposition. The majority of neurites grow parallel to the orientation direction of the collagen. We suggest collagen coating as a possible future option in CI technology to direct neurite outgrowth and improve hearing results for affected patients.
Similar content being viewed by others
Introduction
Profound to severe hearing loss is one of the most common birth defects in industrialized countries with an incidence of up to 2–3 in 1,000 births. Another similar fraction of patients develops hearing loss before reaching adulthood. Toxic noise, ototoxic drugs, and the effects of aging combined with ongoing wear and tear, and genetic disposition result in hearing loss-related impairment in the quality of life in about half of the population at the age of 65. Whereas hearing aids provide some help for mild forms, cochlear implants (CIs) are currently the only therapeutic option in profound deaf patients [1–4].
CIs consist of an electrode array that is surgically inserted into the cochlea of affected patients. They functionally replace lost sensory hair cells, which are located in the organ of Corti, and work by providing direct stimulation of auditory nerve fibers that originate in the spiral ganglion and extend to the hair cells.
Worldwide, more than 140,000 patients use a CI [5], which is the only routinely implanted electronic device capable of functionally restoring a lost sensory function. Despite its large success, there is a substantial variability in the performance of implanted devices. Among other factors, the CIs’ performance greatly depends on the correct positioning of the electrode array inside the cochlea, and a close distance between the electrode array and its target cells, the spiral ganglion neurons/neurites. A correctly positioned device with tight neuron/device interactions requires much less power for nerve stimulation than a sub-optimally positioned implant. More significantly, it is thought that the ability of an implant patient to learn and perform advanced communication tasks, such as participating in a telephone conversation, greatly depends on proper interfacing between the electrodes and the auditory nerve over a broad frequency range. It is generally acknowledged that strategies aimed at improving the interface between the electrodes and the nerve fibers would greatly improve cochlear implant efficacy [6, 7].
Despite extensive research on electrode design for more than 30 years, it is not possible to achieve optimal stimulation of the auditory nerve because of the anatomical gap between the insertion place inside the scala tympani and the remaining deafferented nerve fibers localized nearby in Rosenthal’s canal, a fissure connecting the spiral ganglion with the organ of Corti. Unfortunately, there is generally little growth of auditory nerve fibers toward the electrode array. Factors likely impeding growth includes fibrous tissue accumulating around the implant and the lack of attractant signals for spiral ganglion neurites. Various strategies are currently under investigation to improve this situation. Novel, atraumatic CI electrode design and drug delivery systems [8, 9] are the two possible strategies. Coating of the electrode array with bioactive substrates is another one [10–12].
Collagen is widely used in cosmetic surgery. One of its many functions is guidance of cellular growth in the extracellular matrix [13, 14]. The orientation of collagen fibrils can be influenced by the action of hydrodynamic flow and rapid desiccation leading to a resulting collagen film with a cholesteric banding structure. This oriented collagen has been shown to influence the growth and migration of mammalian fibroblasts [15]. Due to its technically easy handling, oriented collagen offers a mechanism for contact guidance and biomaterial tissue productions [16]. There are no studies available whether collagen orientation is useful for neurite guidance, which prompted our study to assess oriented collagen fibrils as a future component of CI technology.
The aim of this study was to test if spiral ganglion neurons survive on collagen surfaces, whether the orientation of collagen affects the direction of neurite outgrowth, and whether oriented collagen may be useful for CI electrode coating to direct neurite outgrowth along the array surface.
Materials and methods
Animals and tissue preparation
BALB/c mice were used for all experiments. All research was conducted under an approved institutional protocol according to the National Institutes of Health guidelines. Every effort was made to minimize the number of research animals used, as well as their suffering.
The temporal bones of postnatal day 2 (P2) mice were harvested and dissected in ice cold phosphate buffered saline (PBS). After removal of the bony capsule, the entire membranous cochleae of four animals were collected in a 270 μl drop of PBS. For dissociation, 30 μl of dispase (50 units/ml) was added and incubated at 37°C for 40 min. The cochleae were then transferred into 500 μl fresh PBS and incubated at room temperature for another 40 min, and subsequently transferred into a 15 ml centrifuge tube; 500 μl of basic media (BM, 500 ml Dulbecco’s modified Eagle’s medium (DMEM)/high glucose and F-12 media mixed 1:1 containing N2 and B27 supplement) and 10% fetal bovine serum (FBS) were added. Dissociation was performed by gently pipetting up and down with a 1,000 μl filter tip (~30 times). After adding 800 μl more of BM with 10% FBS, 100 μl of the cell suspension was transferred into individual wells of coated 8-well Lab-Tek® II Chamber Slide tissue culture plates filled with 100 μl of prewarmed culture medium, and cultured for 48 h at 37°C and 5% CO2.
Surface coating of tissue culture plates
8-well Lab-Tek® II Chamber Slide tissue culture plates or Greiner 4-well cell culture plastic dishes (Greiner Bio-One) were incubated with poly-d-lysine at 10 mg/ml in PBS for 1 h at 37°C and washed twice with PBS. A subgroup of these wells was then coated with 1 mg/ml mouse laminin in PBS overnight at 4°C. Before tissue or cell transfer, the wells were rinsed once with PBS, twice with BM, and filled with 100 μl culture medium (BM containing 10% FBS, neurotrophin-3 at 30 ng/ml, brain-derived neurotrophic factor at 30 ng/ml, and penicillin at 30 U/ml) and prewarmed for 1–2 h at 37°C, 5% CO2, and 95% humidity.
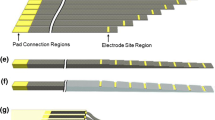
Oriented collagen preparation
Collagen films were created as described before [15, 16]. Briefly, rat tail collagen, type I (BD Biosciences) was purchased at stock concentrations of 10 mg/ml in 0.02 N acetic acid and then dialysed against polyethylene glycol for 20 min at 4°C until the solution reached a final concentration of 20 mg/ml. The substrate used was the glass slide of a Lab-Tek® II Chamber Slide 8-well plate after removal of the upper plastic part and cleaning the glass surface by plasma treatment using a plasma cleaner (Gala instrumente, prep 5). Consistent application of the collagen films was ensured by using a three-axis robotic arm and a syringe pump (I&J Fisnar 500 LN, Harvard Apparatus millilitre OEM pump). Velocity gradients to orient the collagen molecules during deposition were provided by the extensional flow to a relative motion of the syringe tip and the substrate, coupled with the pressure-driven flow out of the syringe. After deposition, the collagen solution was allowed to dry under ambient conditions. Atomic force microscopy was performed to verify the orientation of collagen films depending on the flow parameters (Fig. 1).
Immunolabeling
Cells were fixed for 15 min with 4% paraformaldehyde in PBS at room temperature. Nonspecific binding sites were blocked for 1 h in 0.1% Triton-100, 1% bovine serum albumin, and 5% heat-inactivated goat serum in PBS (PBT1). The fixed cells were incubated overnight at 4°C with a diluted antibody 1:200 for monoclonal mouse antibody to neurofilament M (NF-M) (AbD Serotec). Unbound antibodies were removed by three PBT1 washes and one PBT2 (same as PBT1 without serum) wash for 15 min each at room temperature. An FITC-conjugated species and a subtype-specific secondary antibody (Jackson Immuno Research) were used 1:400 in PBT2 to detect primary antibodies. Short-wavelength nuclear staining agent DAPI (Molecular Probes) was used to visualize cell nuclei. The slides were analyzed by fluorescence microscopy and digital image acquisition (Zeiss Axioimager and AxioCam).
Evaluation and statistical analysis
After immunolabeling, neuronal survival was analyzed by counting all neurons/well and compared relative to maximal survival on poly-l-lysine/laminin-coated surfaces. Data are presented as mean values ± standard deviation (SD) with the number of independent experiments (n) indicated. Statistical differences were determined with paired two-tailed t tests using Excel (Microsoft). Graphs were created using Aabel (Gigawiz) or Excel (Microsoft).
Results
Spiral ganglion neurons survive on collagen and display neurite outgrowth
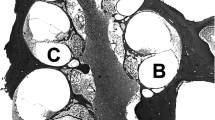
Spiral ganglion neuron survival and neurite growth in vitro is affected by culture substrate such as poly-d-lysine, laminin, or poly-ornithine. Compared to uncoated cell culture plastic, spiral ganglion neuron survival was significantly higher on poly-d-lysine/laminin-coated surfaces (Fig. 2a). When we tested the survival of dissociated spiral ganglion neurons, we first used randomly oriented collagen stripes. We observed a good cell attachment and survival on these stripes (Fig. 2b). Compared to poly-d-lysine/laminin coating, neuronal survival on randomly oriented collagen coating was significantly lower (75.6 ± 10.2%), but it was higher when compared to uncoated cell culture-treated plastic surfaces (45.3 ± 11.1%, Fig. 2a).
Neuronal survival after different surface treatments. a When we count the survival of neurons (NF-M positive cells) after 48 h, a significantly better neuronal survival was observed on poly-d-lysine/laminin-coated surfaces (100%) compared to untreated (p < 0.01), poly-d-lysine-, poly-ornithine-, or collagen-coated surfaces (p < 0.05). b Both neurons and non-neuronal cells (the majority of cells in our assay) preferred to attach on collagen stripes compared to untreated culture dish surfaces
Neurite growth direction is influenced by the flow deposition of collagen
Dissociated spiral ganglion neurons mainly display mono- or bipolar neurite outgrowth in vitro (Fig. 3a). To analyse the influence of oriented collagen on neurite growth, we cultured spiral ganglion neurons in 8-well chamber slides and compared the angle of neurite outgrowth relative to the orientation direction of the collagen. In controls using randomly oriented collagen, we employed the direction of the collagen stripe as benchmark. When we analyzed the controls, there was no significant preference in the outgrowth angle of neurites; they showed a random distribution (Fig. 3b). When we analyzed the neurite growth angle on oriented collagen, we observed a significant preference. The majority of the evaluated neurites grew out from the cell body along the orientation direction of the collagen. Just a few neurites in each experiment were not influenced by the orientation of the collagen and grew out in various angles (Fig. 3b–d).
Collagen orientation was able to influence neurite growth direction. a Typical monopolar spiral ganglion neuron with neurite displays a random, circle shaped neurite outgrowth direction. b Analysis of the angle deviation of neurite growth relative to collagen orientation shows a significant neurite outgrowth along the orientation direction of the collagen compared to non oriented collagen or poly-d-lysine, when we measured the angle of neurite outgrowth relative to the orientation direction of the collagen (subdivided in 15° units, p < 0.05). c, d Higher magnification of spiral ganglion neurites grown on oriented collagen along the orientation direction of the collagen
Discussion
In this study, we show that spiral ganglion neurons survive on collagen-coated culture surfaces and that their neurites grow oriented in the direction of the collagen fibrils. Achieving a directed neuronal growth would be a great advance in neural tissue engineering and especially in improving neuron-device interactions in neural prostheses. During neural development, and especially for the innervation of the cochlear inner hair cells, ephrins and their receptors have been put forward as potential guidance cues [17, 18]. Furthermore, neurotrophins released by sensory hair cells have been suggested as major attractants for afferent fibers during the development of the auditory system [19]. There is a complex dynamic mixture of guidance cues in the local environment of developing peripheral innervation patterns, but in general, the topographies of anisotropic tissue structures have been shown to be sufficient for providing a basic framework for neuronal guidance [20, 21]. These findings suggest that both the shape as well as the surface chemistry of bridging devices for neuronal regeneration affect neurite outgrowth.
A directed spiral ganglion neurite outgrowth toward specific contacts on CI electrode arrays could be a useful strategy to bundle and direct afferent connections once they reach the CI surface. Based on our findings, we suggest that oriented collagen could be a useful biocompatible coating substrate for future CI devices. Multiple layers of collagen can be effectively transferred onto substrates, such as the silicon polymer used in implant devices. Furthermore, collagen can be used to attach neurotrophins such as brain-derived neurotrophic factor, either in a slow-release formulation, or covalently, for example, with appropriate spacers [22], to promote spiral ganglion survival and neurite outgrowth toward the CI and further along the device surface. Due to a covalent attachment, and local release of neurotrophic factors there would be little risk for side effects outside the cochlea, which results in easier clinical trials and with reduced risk for patients.
References
Chen GD (2006) Prestin gene expression in the rat cochlea following intense noise exposure. Hear Res 222:54–61
Lautermann J, Dehne N, Schacht J, Jahnke K (2004) Aminoglycoside- and cisplatin-ototoxicity: from basic science to clinics. Laryngorhinootologie 83:317–323
Liu XZ, Yan D (2007) Ageing and hearing loss. J Pathol 211:188–197
Schwander M, Sczaniecka A, Grillet N, Bailey JS, Avenarius M, Najmabadi H, Steffy BM, Federe GC, Lagler EA, Banan R, Hice R, Grabowski-Boase L, Keithley EM, Ryan AF, Housley GD, Wiltshire T, Smith RJ, Tarantino LM, Muller U (2007) A forward genetics screen in mice identifies recessive deafness traits and reveals that Pejvakin is essential for outer hair cell function. J Neurosci 27:2163–2175
Wilson BS, Dorman MF (2007) The surprising performance of present-day cochlear implants. IEEE Trans Biomed Eng 54:969–972
Wilson BS, Dorman MF (2008) Cochlear implants: current designs and future possibilities. J Rehabil Res Dev 45:695–730
Rothschild RM (2010) Neuroengineering tools/applications for bidirectional interfaces, brain–computer interfaces, and neuroprosthetic implants—a review of recent progress. Front Neuroeng 3:112
Jolly C, Garnham C, Mirzadeh H, Truy E, Martini A, Kiefer J, Braun S (2009) Electrode features for hearing preservation and drug delivery strategies. Adv Otorhinolaryngol 67:28–42
Pettingill LN, Richardson RT, Wise AK, O’Leary SJ, Shepherd RK (2007) Neurotrophic factors and neural prostheses: potential clinical applications based upon findings in the auditory system. IEEE Trans Biomed Eng 54:1138–1148
Tykocinski M, Cowan RS (2005) Poly-vinyl-alcohol (PVA) coating of cochlear implant electrode arrays: an in vivo biosafety study. Cochlear Implants Int 6:16–30
Richardson RT, Thompson B, Moulton S, Newbold C, Lum MG, Cameron A, Wallace G, Kapsa R, Clark G, O’Leary S (2007) The effect of polypyrrole with incorporated neurotrophin-3 on the promotion of neurite outgrowth from auditory neurons. Biomaterials 28:513–523
Volkenstein S, Brors D, Hansen S, Minovi A, Laub M, Jennissen HP, Dazert S, Neumann A (2009) Influence of bone morphogenetic protein-2 on spiral ganglion neurite growth in vitro. Eur Arch Otorhinolaryngol 266:1381–1389
Mutsaers SE, Bishop JE, McGrouther G, Laurent GJ (1997) Mechanisms of tissue repair: from wound healing to fibrosis. Int J Biochem Cell Biol 29:5–17
Leitinger B, Hohenester E (2007) Mammalian collagen receptors. Matrix Biol 26:146–155
Goffin JJ, Rajadas J, Fuller GG (2010) Interfacial flow processing of collagen. Langmuir 26:3514–3521
Kirkwood JE, Fuller GG (2009) Liquid crystalline collagen: a self-assembled morphology for the orientation of mammalian cells. Langmuir 25:3200–3206
Klein R (2009) Bidirectional modulation of synaptic functions by Eph/ephrin signaling. Nat Neurosci 12:15–20
Brors D, Bodmer D, Pak K, Aletsee C, Schäfers M, Dazert S, Ryan AF (2003) EphA4 provides repulsive signals to developing cochlear ganglion neurite smediated through ephrin-B2 and -B3. J Comp Neurol 462:90–100
Rubel EW, Fritzsch B (2002) Auditory system development: primary auditory neurons and their targets. Annu Rev Neurosci 25:51–101
Smeal RM, Tresco PA (2008) The influence of substrate curvature on neurite outgrowth is cell type dependent. Exp Neurol 213:281–292
Kofron CM, Liu YT, López-Fagundo CY, Mitchel JA, Hoffman-Kim D (2010) Neurite outgrowth at the biomimetic interface. Ann Biomed Eng 38:2210–2225
Pardridge WM, Wu D, Sakane T (1998) Combined use of carboxyl-directed protein pegylation and vector-mediated blood-brain barrier drug delivery system optimizes brain uptake of brain-derived neurotrophic factor following intravenous administration. Pharm Res 15:576–582
Acknowledgments
This work was supported by a BioX-grant of Stanford University to Drs. G.F., Frank Longo, and S.H., by Med-El Worldwide Headquarters Innsbruck, Austria, by the US National Institutes of Health grants DC06167 and P30 DC010363 to S.H., and by a postdoctoral fellowship of the Deutsche Akademie der Naturforscher Leopoldina (German Academy of Science, BMBF-LPD 9901/8-171) to S.V.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Volkenstein, S., Kirkwood, J.E., Lai, E. et al. Oriented collagen as a potential cochlear implant electrode surface coating to achieve directed neurite outgrowth. Eur Arch Otorhinolaryngol 269, 1111–1116 (2012). https://doi.org/10.1007/s00405-011-1775-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-011-1775-8