Abstract
Purpose
To compare the perinatal outcome in multifetal pregnancies containing a monochorionic twin pair, managed either expectantly or by fetal reduction (MFPR).
Methods
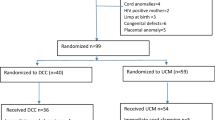
This was a retrospective analysis of prospectively collected data on 47 triplet and 10 quadruplet pregnancies recruited between 10 and 14 weeks. Main outcome measures were miscarriage <24 weeks, preterm birth, fetal growth restriction, birth weight and survival rates.
Results
For triplets the miscarriage rates <24 weeks were 6.3 % after reduction and 20.0 % for expectant management and MFPR, respectively. While we recorded no case of severe preterm delivery <30 weeks in the reduction group, it was 25 % in those with expectant management. Mean gestational age and birth weight were significantly higher after fetal reduction than for the conservative approach (37.7 ± 1.6 weeks vs. 30.9 ± 3.2 weeks, p < 0.01 and 2676 ± 705 g vs. 1429 ± 542 g, p < 0.01). Expectantly managed triplets were complicated by twin–twin transfusion syndrome in 18.8 % and intrauterine fetal death in 8.3 %. Survival rates were 85.4 % for those managed expectantly and 80.0 % after fetal reduction. Mean gestational age of ongoing quadruplets was 26.9 ± 2.0 weeks vs. 34.5 ± 4.3 weeks for those with reduction of the monochorionic pair (p < 0.05). Survival rates were 100 % in the reduction group and 58.3 % in the expectant management group (p < 0.05). There was an inverse correlation between the final number of fetuses and the birth weight.
Conclusion
Fetal reduction in triplets and quadruplets including a monochorionic pair is associated with decreased early prematurity. While in quadruplets the overall survival is higher after reduction, there was no difference for dichorionic triplets with reduction or conservative management. Complications owing to monochorionicity are frequently observed.
Similar content being viewed by others
References
Sebire NJ, Snijders RJ, Hughes K, Sepulveda W, Nicolaides KH (1997) The hidden mortality of monochorionic twin pregnancies. Br J Obstet Gynaecol 104:1203–1207
Antsaklis A, Souka AP, Daskalakis G, Papantoniou N, Koutra P, Kavalakis Y et al (2004) Pregnancy outcome after multifetal pregnancy reduction. J Matern Fetal Neonatal Med 16:27–31
Skiadas CC, Missmer SA, Benson CB, Acker D, Racowsky C (2011) Spontaneous reduction before 12 weeks’ gestation and selective reduction similarly extend time to delivery in in vitro fertilization of trichorionic-triamniotic triplets. Fertil Steril 95:596–599
Blickstein I, Keith LG (2005) The decreased rates of triplets births: temporal trends and biologic speculations. Am J Obstet Gynecol 193:327–331
Chow JS, Benson CB, Racowsky C, Doubilet PM, Ginnsberg E (2001) Frequency of a monochorionic pair in multiple gestations. Relationship to mode of conception. J Ultrasound Med 20:757–760
De Catte L, Camus M, Foulon W (2002) Monochorionic high-order multiple pregnancies and multifetal pregnancy reduction. Obstet Gynecol 100:561–566
Geipel A, Berg C, Katalinic A, Plath H, Hansmann M, Germer U et al (2005) Prenatal diagnosis and obstetric outcomes in triplet pregnancies in relation to chorionicity. BJOG 112:554–558
Bajoria R, Ward SB, Adegbite AL (2006) Comparative study of perinatal outcome of dichorionic and trichorionic iatrogenic triplets. Am J Obstet Gynecol 194:415–424
Adegbite AL, Ward SB, Bajoria R (2005) Perinatal outcome of spontaneously conceived triplet pregnancies in relation to chorionicity. Am J Obstet Gynecol 193:1463–1471
Chaveeva P, Kosinski P, Puglia D, Poon LC, Nicolaides KH (2013) Trichorionic and dichorionic triplet pregnancies at 10–14 weeks: outcome after embryo reduction compared to expectant management. Fetal Diagn Ther 34:199–205
Papageorghiou AT, Avgidou K, Bakoulas V, Sebire NJ, Nicolaides KH (2006) Risks of miscarriage and early preterm birth in trichorionic triplet pregnancies with embryo reduction versus expectant management: new data and systematic review. Hum Reprod 21:1912–1917
Stone J, Ferrara L, Kamrath J, Getrajdman J, Berkowitz R, Moshier E et al (2008) Contemporary outcomes with the latest 1000 cases of multifetal pregnancy reduction (MPR). Am J Obstet Gynecol 199(406):e1–e4
Wimalasundera RC (2010) Selective reduction and termination of multiple pregnancies. Semin Fetal Neonatal Med 15:327–335
Morlando M, Ferrara L, D’Antonio F, Lawin-O’Brien A, Sankaran S, Pasupathy D et al (2015) Dichorionic triplet pregnancies: risk of miscarriage and severe preterm delivery with fetal reduction versus expectant management. Outcomes of a cohort study and systematic review. BJOG 122:1053–1060
Voigt M, Schneider KTM, Jährig K (1996) Analyse des Geburtsgutes des Jahrgangs 1992 der Bundesrepublik Deutschland. Teil 1: Neue Perzentilwerte für die Körpermaße von Neugeborenen. Geburtsh Frauenheilk 56:550–558
Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK, Kruger M (1999) Staging of twin-twin transfusion syndrome. J Perinatol 19:550–555
Peeters SH, Middeldorp JM, Lopriore E, Klumper FJ, Oepkes D (2012) Monochorionic triplets complicated by fetofetal transfusion syndrome: a case series and review of the literature. Fetal Diagn Ther 32:239–245
McPherson JA, Odibo AO, Shanks AL, Roehl KA, Macones GA, Cahill AG (2012) Impact of chorionicity on risk and timing of intrauterine fetal demise in twin pregnancies. Am J Obstet Gynecol 207:190.e1–190.e6
Adegbite AL, Ward BS, Bajora R (2007) Perinatal outcome of quadruplet pregnancies in relation to chorionicity. J Perinatol 27:15–21
Evans MI, Berkowitz RL, Wapner RJ, Carpenter RJ, Goldberg JD, Ayoub MA et al (2001) Improvement in outcomes of multifetal pregnancy reduction with increased experience. Am J Obstet Gynecol 184:97–103
Stone J, Eddleman K, Lynch L, Berkowitz RL (2002) A single center experience with 1000 consecutive cases of multifetal pregnancy reduction. Am J Obstet Gynecol 187:1163–1167
van de Mheen L, Everwijn SM, Knapen MF, Oepkes D, Engels M, Manten GT, Zondervan H et al (2014) The effectiveness of multifetal pregnancy reduction in trichorionic triplet gestation. Am J Obstet Gynecol 210:536
Li R, Chen X, Yang S, Yang R, Ma C, Liu P et al (2013) Retain singleton or twins? Multifetal pregnancy reduction strategies in triplet pregnancies with monochorionic twins. Eur J Obstet Gynecol Reprod Biol 167:146–148
Chaveeva P, Kosinski P, Birdir C, Orosz L, Nicolaides KH (2014) Embryo reduction in dichorionic triplets to dichorionic twins by intrafetal laser. Fetal Diagn Ther 35:83–86
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The institutional review boards of the University of Bonn do not require formal approval for retrospective archive studies therefore an ethical approval was not sought.
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Abel, J.S., Flöck, A., Berg, C. et al. Expectant management versus multifetal pregnancy reduction in higher order multiple pregnancies containing a monochorionic pair and a review of the literature. Arch Gynecol Obstet 294, 1167–1173 (2016). https://doi.org/10.1007/s00404-016-4145-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4145-3