Abstract
Introduction
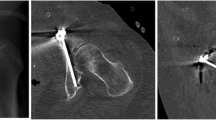
The number of pelvic fractures based on osteoporosis has been increasing. The infra-acetabular screw (IAS), which connected both osseous columns, is a safe method of screw placement going through the infra-acetabular corridor (IAC). However, the specifics of the anatomy of IAC have been far from completely understood, especially in the Asian population. The purpose of our study was to reveal the details of the IAC using computed tomography (CT) data.
Materials and methods
Traumatized in-patients having pelvic CT scans from 2014 to 2016 were enrolled. Pediatric and adult patients with pelvic fractures and hip prostheses were excluded. The male/female ratio and distribution of patients' age were equalized manually; 40 male and 40 female patients were included. The IAC was measured on the plane of the inlet view (25° caudal) in multi-planar reconstructed CT images. Measurements: infra-acetabular diameter (IAD), anterior–posterior length of the IAC (APL), length from the starting point of the IAC to the medial edge of the pelvis (LME), length from the starting point of the IAC to the top of the pubic symphysis (LPS), and tilting on inlet plate (TIP).
Results
Age was 59 ± 22 (mean ± SD). Height was 159 ± 11 cm, and body mass index (BMI) was 22.9 ± 4.1. IAD, APL, LME, LPS, and TIP was 4.0 ± 1.3 mm, 89.5 ± 7.1 mm, 8.7 ± 3.6 mm, 57.8 ± 4.8 mm, and 4.7 ± 5.2°, respectively. Over 20% of corridors (35 of 160) were not feasible for IAS placement, because of inadequate width (less than 3.0 mm). Nine corridors (5.6%) had curvature in IAC, which meant technically demanding to insert IAS. There was no difference in IAD between male and female patients, while APL, LME, LPS, and TIP had sex-related differences.
Conclusions
Surgeons should pay attention to the fact that over 20% of IACs are not feasible for infra-acetabular screw placement even with the perfect reduction of fragments when treating acetabular fractures.





Similar content being viewed by others
References
Matta MJ (2006) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Jt Surg 76:1632–1645
Kuma A, Shar NA, Kershaw SA, Clayson AD (2005) Operative management of acetabular fractures: a review of 73 fractures. Injury 36:605–612
Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD (2014) Acetabular fractures in patients aged > 55 years: a systematic review of the literature. J Bone Jt Surg 96:157–163
Rinne PP, Laitinen MK, Huttunen T, Kannus P, Mattila VM (2017) The incidence and trauma mechanism of acetabular fractures: a nationwide study in Finland between 1997 and 2014. Injury 48:2157–2161
Miller AN, Prasarn ML, Lorich DG, Helfet DL (2010) The radiological evaluation of acetabular fractures in the elderly. J Bone Jt Surg 92:560–564
Laflamme GY, Hevert-Davies J, Rouleau D, Benoit B, Leduc S (2011) Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury 42:1130–1134
Letournel E, Judet R (1993) Fractures of the acetabulum. Springer, New York
Culemann U, Marintschev I, Gras F, Pohlemann T (2011) Infra-acetabular corridor—technical tip for an additional screw placement to increase the fixation strength of acetabular fractures. J Trauma 70:244–246
Marintschev I, Gras F, Schwarz CE, Pohlemann T, Hofmann GO, Culemann U (2012) Biomechanical comparison of different acetabular plate systems and constructs: the role of infra-acetabular screw placement and use of locking plates. Injury 43:470–474
Gras F, Gottschling H, Schröder M, Marintschev I, Reimers N, Burgkart R (2015) Sex-specific differences of the infraacetabular corridor: a biomorphometric CT-based analysis on a database of 523 pelves. Clin Orthop Relat Res 473:361–369
Baumann F, Schmitz P, Mahr D, Kerschbaum M, Gänsslen A, Nerlich M et al (2018) A guideline for placement of an infra-acetabular screw based on anatomic landmarks via an intra-pelvic approach. J Orthop Surg Res 13:77
Uehara T, Noda T, Yoshimura M, Ozaki T, Yamakawa Y, Kinami Y (2016) Safe zone of posterior column screws and infraacetabular screws for acetabular fractures. Kossetsu (Japanese) 38:811–815
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or a member of their immediate family has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kanezaki, S., Miyazaki, M., Notani, N. et al. Analysis of computed tomography-based infra-acetabular morphometry to assess the feasibility of infra-acetabular screws. Arch Orthop Trauma Surg 140, 359–364 (2020). https://doi.org/10.1007/s00402-019-03280-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03280-x