Abstract
Background
There is currently a trend toward minimally invasive total knee arthroplasty (TKA) to decrease the morbidity related to the standard approach. The aim of our study was to clarify whether the mini-subvastus surgical had an advantage over the standard in term of pain level, blood loss, and postoperative recovery, whether the mini-subvastus surgical was prone to radiographic malalignment, prolonged operative time, and increased complications.
Methods
In a prospective randomized study, we compared the clinical and radiological results of primary TKA using a mini-subvastus approach or a standard approach in 68 patients. The mini-subvastus approach was used on 35 patients (group I) and the standard approach on 33 patients (group II).
Results
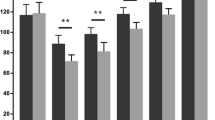
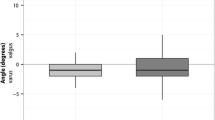
The mean follow-up was 28 months (range 24–36 months). Patients in group I had less blood loss and better visual analogue scale score at 1 day postoperatively. They achieved active straight leg raise earlier and underwent less lateral retinacular releases. The mean Knee Society function score, Oxford knee score, and range of movement were significantly better in group I up to 9 months after surgery (all, p < 0.05). However, there were no significant differences in these parameters between the groups at final follow-up. Reduced access and visibility in group I prolonged tourniquet time by an average of 22 min and resulted in five technical errors on radiographic evaluation.
Conclusions
Patients can receive marked but temporary benefits from the mini-subvastus technique, with a definite cost: that of component malposition and prolongation of operative time.





Similar content being viewed by others
References
Stern SH, Insall JN (1992) Posterior stabilized prosthesis: results after follow-up of 9–12 years. J Bone Jt Surg Am 74:980–986
Ranawat CS, Flynn WF Jr, Saddler S et al (1993) Long-term results of the total condylar knee arthroplasty: a 15-year survivorship study. Clin Orthop Relat Res 286:94–102
Colizza WA, Insall JN, Scuderi GR (1995) The posterior stabilized total knee prosthesis: assessment of polyethylene damage and osteolysis after a 10-year-minimum follow-up. J Bone Jt Surg Am 77:1713–1720
Buechel FF Sr (2002) Long-term follow-up after mobile-bearing total knee replacement. Clin Orthop Relat Res 404:40–50
Bullens PH, van Loon CJ, de Waal Malefijt MC et al (2001) Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplast 16:740–747
Walton NP, Jahromi I, Dobson PJ et al (2005) Arthrofibrosis following total knee replacement; does therapeutic warfarin make a difference? Knee 12:103–106
Tenholder M, Clarke HD, Scuderi GR (2005) Minimal-incision total knee arthroplasty: the early clinical experience. Clin Orthop Relat Res 440:67–76
Haas SB, Cook S, Beksac B (2004) Minimally invasive total knee replacement through a mini midvastus approach: a comparative study. Clin Orthop Relat Res 428:68–73
Laskin RS, Beksac B, Phongjunakorn A et al (2004) Minimally invasive total knee replacement through a mini-midvastus incision: an outcome study. Clin Orthop Relat Res 428:74–81
Karachalios T, Giotikas D, Roidis N et al (2008) Total knee replacement performed with either a mini-midvastus or a standard approach: a prospective randomized clinical and radiological trial. J Bone Jt Surg Br 90:584–591
Haas SB, Manitta MA, Burdick P (2006) Minimally invasive total knee arthroplasty: the mini midvastus approach. Clin Orthop Relat Res 452:112–116
Schroer WC, Diesfeld PJ, Reedy ME et al (2008) Mini-subvastus approach for total knee arthroplasty. J Arthroplast 23:19–25
Schroer WC, Diesfeld PJ, Reedy ME et al (2007) Evaluation of complications associated with six hundred mini-subvastus total knee arthroplasties. J Bone Jt Surg Am 89:76–81
Kashyap SN, van Ommeren JW (2008) Clinical experience with less invasive surgery techniques in total knee arthroplasty: a comparative study. Knee Surg Sports Traumatol Arthrosc 16:544–548
Boerger TO, Aglietti P, Mondanelli N et al (2005) Mini-subvastus versus medial parapatellar approach in total knee arthroplasty. Clin Orthop Relat Res 440:82–87
Aglietti P, Baldini A, Sensi L (2006) Quadriceps-sparing versus mini-subvastus approach in total knee arthroplasty. Clin Orthop Relat Res 452:106–111
Tria AJ Jr, Coon TM (2003) Minimal incision total knee arthroplasty: early experience. Clin Orthop Relat Res 416:185–190
Chen AF, Alan RK, Redziniak DE et al (2006) Quadriceps sparing total knee replacement: the initial experience with results at 2–4 years. J Bone Jt Surg Br 88:1448–1453
Kim YH, Kim JS, Kim DY (2007) Clinical outcome and rate of complications after primary total knee replacement performed with quadriceps-sparing or standard arthrotomy. J Bone Jt Surg Br 89:467–470
Scuderi GR, Tenholder M, Capeci C (2004) Surgical approaches in mini-incision total knee arthroplasty. Clin Orthop Relat Res 428:61–67
Kim JG, Lee SW, Ha JK et al (2011) The effectiveness of minimally invasive total knee arthroplasty to preserve quadriceps strength: a randomized controlled trial. Knee 18:443–447
Liebensteiner MC, Krismer M, Koller A et al (2012) Does minimally invasive total knee arthroplasty improve isokinetic torque? Clin Orthop Relat Res 470:3233–3239
Insall JN, Dorr LD, Scott RD et al (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Baker PN, van der Meulen JH, Lewsey J et al (2007) The role of pain and function in determining patient satisfaction after total knee replacement: data from the national joint registry for England and Wales. J Bone Jt Surg Br 89:893–900
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Benjamin J, Chilvers M (2006) Correcting lateral patellar tilt at the time of total knee arthroplasty can result in overuse of lateral release. J Arthroplast 21:121–126
Pagnano MW, Meneghini RM, Trousdale RT (2006) Anatomy of the extensor mechanism in reference to quadriceps-sparing TKA. Clin Orthop Relat Res 452:102–105
Holt G, Nunn T, Allen RA et al (2008) Variation of the vastus medialis obliquus insertion and its relevance to minimally invasive total knee arthroplasty. J Arthroplast 23:600–604
Hoffman AA, Plaster RL, Murdock LE (1991) Subvastus (Southern) approach for primary knee arthroplasty. Clin Orthop Relat Res 269:70–77
Bindeglass DF, Vince KG (1996) Patellar tilt and subluxation following subvastus and parapatellar approach in total knee arthroplasty. J Arthroplast 11:507–511
Dalury DF, Dennis DA (2005) Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop Relat Res 440:77–81
King J, Stamper DL, Schaad DC et al (2007) Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty. Assessment of learning curve and the postoperative recuperative period. J Bone Jt Surg Am 89:1497–1503
Acknowledgments
We thank X. G. Li for linguistic revision and statistical data. We also thank the participating surgeons at the Department of Orthopaedics The First Hospital Affiliated to Suzhou University, J. Y. Sun, Y. Z. Xu, and T. S. Tang.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Archives of Orthopaedic and Trauma Surgery, Springer-Verlag Berlin Heidelberg 2014. This paper, published in Volume 134, Issue 8, pages 1155-1162, DOI 10.1007/s00402-014-1963-2, has been formally withdrawn by the two corresponding authors on ethical grounds because the article contains extensive and repeated instances of plagiarism. Archives of Orthopaedic and Trauma Surgery treats all identified evidence of plagiarism in the published articles most seriously. It is unfortunate that this misconduct was not detected before going to press. The authors apologize to the Editors and readers as well as the authors of the original article.
About this article
Cite this article
Lai, Z., Shi, S., Fei, J. et al. RETRACTED ARTICLE: Total knee arthroplasty performed with either a mini-subvastus or a standard approach: a prospective randomized controlled study with a minimum follow-up of 2 years. Arch Orthop Trauma Surg 134, 1155–1162 (2014). https://doi.org/10.1007/s00402-014-1963-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-1963-2