Abstract
High-density lipoproteins (HDL) are the major plasma carriers for sphingosine 1-phosphate (S1P) in healthy individuals, but their S1P content is unknown for patients with coronary artery disease (CAD). The aim of the study was to determine whether the S1P levels in plasma and HDL are altered in coronary artery disease. S1P was determined in plasma and HDL isolated by ultracentrifugation from patients with myocardial infarction (MI, n = 83), stable CAD (sCAD, n = 95), and controls (n = 85). In our study, total plasma S1P levels were lower in sCAD than in controls (305 vs. 350 pmol/mL). However, normalization to HDL-cholesterol (a known determinant of plasma S1P) revealed higher normalized plasma S1P levels in sCAD than in controls (725 vs. 542 pmol/mg) and even higher ones in MI (902 pmol/mg). The S1P amount contained in isolated HDL from these individuals was lower in sCAD than in controls (S1P per protein in HDL: 132 vs. 153 pmol/mg). The amount of total plasma S1P bound to HDL was lower in sCAD and MI than in controls (sCAD: 204, MI: 222, controls: 335 pmol/mL), while the non-HDL-bound S1P was, accordingly, higher (sCAD: 84, MI: 81, controls: 10 pmol/mL). HDL-bound plasma S1P was dependent on the plasma HDL-C in all groups, but normalization to HDL-C still yielded lower HDL-bound plasma S1P in patients with sCAD than in controls (465 vs. 523 pmol/mg). The ratio of non-HDL-bound plasma S1P to HDL-C-normalized HDL-bound S1P was also higher in both sCAD (0.18 mg/mL) and MI (0.15 mg/mL) than in controls (0.02 mg/mL). Remarkably, levels of non-HDL-bound plasma S1P correlated with the severity of CAD symptoms as graded by Canadian Cardiovascular Score, and discriminated patients with MI and sCAD from controls. Furthermore, a negative association was present between non-HDL-bound plasma S1P and the S1P content of isolated HDL in controls, but was absent in sCAD and MI. Finally, MI patients with symptom duration of less than 12 h had the highest levels of total and normalized plasma S1P, as well as the highest levels of S1P in isolated HDL. The HDL-C-normalized plasma level of S1P is increased in sCAD and even further in MI. This may be caused by an uptake defect of HDL for plasma S1P in CAD, and may represent a novel marker of HDL dysfunction.




Similar content being viewed by others
References
Murata N, Sato K, Kon J, Tomura H, Yanagita M, Kuwabara A, Ui M, Okajima F (2000) Interaction of sphingosine 1-phosphate with plasma components, including lipoproteins, regulates the lipid receptor-mediated actions. Biochem J 352:809–815
von Eckardstein A, Hersberger M, Rohrer L (2005) Current understanding of the metabolism and biological actions of HDL. Curr Opin Clin Nutr Metab Care 8:147–152
Zhang B, Tomura H, Kuwabara A, Kimura T, Miura S, Noda K, Okajima F, Saku K (2005) Correlation of high density lipoprotein (HDL)-associated sphingosine 1-phosphate with serum levels of HDL-cholesterol and apolipoproteins. Atherosclerosis 178:199–205
Nofer JR, van der Giet M, Tolle M, Wolinska I, von Wnuck Lipinski K, Baba HA, Tietge UJ, Godecke A, Ishii I, Kleuser B, Schafers M, Fobker M, Zidek W, Assmann G, Chun J, Levkau B (2004) HDL induces NO-dependent vasorelaxation via the lysophospholipid receptor S1P3. J Clin Invest 113:569–581
Theilmeier G, Schmidt C, Herrmann J, Keul P, Schafers M, Herrgott I, Mersmann J, Larmann J, Hermann S, Stypmann J, Schober O, Hildebrand R, Schulz R, Heusch G, Haude M, von Wnuck Lipinski K, Herzog C, Schmitz M, Erbel R, Chun J, Levkau B (2006) High-density lipoproteins and their constituent, sphingosine-1-phosphate, directly protect the heart against ischemia/reperfusion injury in vivo via the S1P3 lysophospholipid receptor. Circulation 114:1403–1409
Kontush A, Therond P, Zerrad A, Couturier M, Negre-Salvayre A, de Souza JA, Chantepie S, Chapman MJ (2007) Preferential sphingosine-1-phosphate enrichment and sphingomyelin depletion are key features of small dense HDL3 particles: relevance to antiapoptotic and antioxidative activities. Arterioscler Thromb Vasc Biol 27:1843–1849
Xia P, Gamble JR, Rye KA, Wang L, Hii CS, Cockerill P, Khew-Goodall Y, Bert AG, Barter PJ, Vadas MA (1998) Tumor necrosis factor-alpha induces adhesion molecule expression through the sphingosine kinase pathway. Proc Natl Acad Sci USA 95:14196–14201
Shimamura K, Takashiro Y, Akiyama N, Hirabayashi T, Murayama T (2004) Expression of adhesion molecules by sphingosine 1-phosphate and histamine in endothelial cells. Eur J Pharmacol 486:141–150
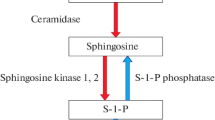
Sattler K, Levkau B (2009) Sphingosine-1-phosphate as a mediator of high-density lipoprotein effects in cardiovascular protection. Cardiovasc Res 82:201–211
Deutschman DH, Carstens JS, Klepper RL, Smith WS, Page MT, Young TR, Gleason LA, Nakajima N, Sabbadini RA (2003) Predicting obstructive coronary artery disease with serum sphingosine-1-phosphate. Am Heart J 146:62–68
Hamm CW (2004) Guidelines: acute coronary syndrome (ACS). 2: Acute coronary syndrome with ST-elevation. Z Kardiol 93:324–341
Hamm CW (2004) Guidelines: acute coronary syndrome (ACS). 1: ACS without persistent ST segment elevations. Z Kardiol 93:72–90
Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB (1975) A reporting system on patients evaluated for coronary artery disease Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 51:5–40
Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, Rosengren A, Steg PG, Tubaro M, Verheugt F, Weidinger F, Weis M, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Aguirre FV, Al-Attar N, Alegria E, Andreotti F, Benzer W, Breithardt O, Danchin N, Di Mario C, Dudek D, Gulba D, Halvorsen S, Kaufmann P, Kornowski R, Lip GY, Rutten F (2008) Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J 29:2909–2945
Hannun YA, Obeid LM (2008) Principles of bioactive lipid signalling: lessons from sphingolipids. Nat Rev Mol Cell Biol 9:139–150
Assmann G, Schulte H, von Eckardstein A, Huang Y (1996) High-density lipoprotein cholesterol as a predictor of coronary heart disease risk. The PROCAM experience and pathophysiological implications for reverse cholesterol transport. Atherosclerosis 124(Suppl):S11–S20
Miller M, Seidler A, Kwiterovich PO, Pearson TA (1992) Long-term predictors of subsequent cardiovascular events with coronary artery disease and ‘desirable’ levels of plasma total cholesterol. Circulation 86:1165–1170
(1992) Lipids and lipoproteins in symptomatic coronary heart disease. Distribution, intercorrelations, and significance for risk classification in 6,700 men and 1,500 women. The Bezafibrate Infarction Prevention (BIP) Study Group, Israel. Circulation 86:839–848
Freedman DS, Otvos JD, Jeyarajah EJ, Barboriak JJ, Anderson AJ, Walker JA (1998) Relation of lipoprotein subclasses as measured by proton nuclear magnetic resonance spectroscopy to coronary artery disease. Arterioscler Thromb Vasc Biol 18:1046–1053
Asztalos BF, Roheim PS, Milani RL, Lefevre M, McNamara JR, Horvath KV, Schaefer EJ (2000) Distribution of ApoA-I-containing HDL subpopulations in patients with coronary heart disease. Arterioscler Thromb Vasc Biol 20:2670–2676
Zheng L, Nukuna B, Brennan ML, Sun M, Goormastic M, Settle M, Schmitt D, Fu X, Thomson L, Fox PL, Ischiropoulos H, Smith JD, Kinter M, Hazen SL (2004) Apolipoprotein A-I is a selective target for myeloperoxidase-catalyzed oxidation and functional impairment in subjects with cardiovascular disease. J Clin Invest 114:529–541
Bergt C, Pennathur S, Fu X, Byun J, O’Brien K, McDonald TO, Singh P, Anantharamaiah GM, Chait A, Brunzell J, Geary RL, Oram JF, Heinecke JW (2004) The myeloperoxidase product hypochlorous acid oxidizes HDL in the human artery wall and impairs ABCA1-dependent cholesterol transport. Proc Natl Acad Sci USA 101:13032–13037
Shao B, Oda MN, Bergt C, Fu X, Green PS, Brot N, Oram JF, Heinecke JW (2006) Myeloperoxidase impairs ABCA1-dependent cholesterol efflux through methionine oxidation and site-specific tyrosine chlorination of apolipoprotein A-I. J Biol Chem 281:9001–9004
Holvoet P, Peeters K, Lund-Katz S, Mertens A, Verhamme P, Quarck R, Stengel D, Lox M, Deridder E, Bernar H, Nickel M, Theilmeier G, Ninio E, Phillips MC (2001) Arg123-Tyr166 domain of human ApoA-I is critical for HDL-mediated inhibition of macrophage homing and early atherosclerosis in mice. Arterioscler Thromb Vasc Biol 21:1977–1983
Zerrad-Saadi A, Therond P, Chantepie S, Couturier M, Rye KA, Chapman MJ, Kontush A (2009) HDL3-mediated inactivation of LDL-associated phospholipid hydroperoxides is determined by the redox status of apolipoprotein A-I and HDL particle surface lipid rigidity: relevance to inflammation and atherogenesis. Arterioscler Thromb Vasc Biol 29:2169–2175
Bradamante S, Barenghi L, Giudici GA, Vergani C (1992) Free radicals promote modifications in plasma high-density lipoprotein: nuclear magnetic resonance analysis. Free Radic Biol Med 12:193–203
Vaisar T, Pennathur S, Green PS, Gharib SA, Hoofnagle AN, Cheung MC, Byun J, Vuletic S, Kassim S, Singh P, Chea H, Knopp RH, Brunzell J, Geary R, Chait A, Zhao XQ, Elkon K, Marcovina S, Ridker P, Oram JF, Heinecke JW (2007) Shotgun proteomics implicates protease inhibition and complement activation in the antiinflammatory properties of HDL. J Clin Invest 117:746–756
Zheng L, Settle M, Brubaker G, Schmitt D, Hazen SL, Smith JD, Kinter M (2005) Localization of nitration and chlorination sites on apolipoprotein A-I catalyzed by myeloperoxidase in human atheroma and associated oxidative impairment in ABCA1-dependent cholesterol efflux from macrophages. J Biol Chem 280:38–47
Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, Kastelein JJ, Bittner V, Fruchart JC (2007) HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med 357:1301–1310
Kontush A, Chapman MJ (2006) Functionally defective high-density lipoprotein: a new therapeutic target at the crossroads of dyslipidemia, inflammation, and atherosclerosis. Pharmacol Rev 58:342–374
Sorrentino SA, Besler C, Rohrer L, Meyer M, Heinrich K, Bahlmann FH, Mueller M, Horvath T, Doerries C, Heinemann M, Flemmer S, Markowski A, Manes C, Bahr MJ, Haller H, von Eckardstein A, Drexler H, Landmesser U (2010) Endothelial-vasoprotective effects of high-density lipoprotein are impaired in patients with type 2 diabetes mellitus but are improved after extended-release niacin therapy. Circulation 121:110–122
Alberti KG, Zimmet P, Shaw J (2005) The metabolic syndrome—a new worldwide definition. Lancet 366:1059–1062
Acknowledgments
We thank Anika Münk for her excellent technical assistance in sample preparation and lipid extraction. This work was supported by the Deutsche Forschungsgemeinschaft (LE940/4-1 to B.L., and GR1943/1-4, GR1943/2-1 to M.G.) and Hans und Gertie Fischer-Stiftung to B.L.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Waltenberger, Maastricht, NL served as guest editor for the manuscript and was responsible for all editorial decisions, including the selection of reviewers. The policy applies to all manuscripts with authors from the editor’s institution.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sattler, K.J.E., Elbasan, Ş., Keul, P. et al. Sphingosine 1-phosphate levels in plasma and HDL are altered in coronary artery disease. Basic Res Cardiol 105, 821–832 (2010). https://doi.org/10.1007/s00395-010-0112-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00395-010-0112-5