Abstract
Aims
This study aimed to assess the relative efficacy and tolerability of etoricoxib, celecoxib, and naproxen at recommended dosages in patients with osteoarthritis (OA).
Methods
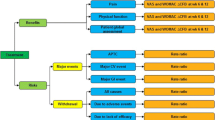
Randomized controlled trials (RCTs) examining the efficacy and tolerability of etoricoxib 30–60 mg, celecoxib 200–400 mg, and naproxen 1000 mg, based on the number of patient withdrawals among those with OA, were included in this network meta-analysis. We performed a Bayesian random-effects network meta-analysis to combine direct and indirect evidence from the RCTs.
Results
Eight RCTs, including 5,942 patients, met the inclusion criteria. The proportion of patient withdrawals due to lack of efficacy was significantly lower in the etoricoxib 30–60 mg (OR 0.21, 95 % CrI 0.12–0.38), celecoxib 200–400 mg (OR 0.29, 95 % CrI 0.18–0.47), and naproxen 1000 mg (OR 0.31, 95 % CrI 0.18–0.51) groups than in the placebo group. The number of patient withdrawals due to lack of efficacy tended to be lower in the etoricoxib 30–60 mg group than in the naproxen 1000 mg and celecoxib 200–400 mg groups, although they did not reach statistical significance (OR 0.68, 95 % CrI 0.36–1.33 and OR 0.70, 95 % CrI 0.38–1.37, respectively). Ranking probabilities based on the surface under the cumulative ranking curve (SUCRA) indicated that etoricoxib 30–60 mg had the highest probability of being the best treatment based on the number of withdrawals due to lack of efficacy (SUCRA = 0.9168) followed by celecoxib 200–400 mg (SUCRA = 0.5659), naproxen 1000 mg (SUCRA = 0.5171), and placebo (SUCRA = 0.000189). With respect to tolerability, the number of withdrawals due to adverse events was not significantly different among etoricoxib, celecoxib, naproxen, and placebo, although it tended to be lower with etoricoxib and placebo.
Conclusions
Etoricoxib 30–60 mg, celecoxib 200–400 mg, and naproxen 1000 mg were more efficacious than placebo. However, there was no significant difference in efficacy and tolerability between the medications.
Zusammenfassung
Ziele
Ziel dieser Studie ist es, die relative Wirksamkeit und Verträglichkeit von Etoricoxib, Celecoxib und Naproxen in den empfohlenen Dosierungen bei Patienten mit Osteoarthritis (OA) zu bewerten.
Methoden
Randomisiert-kontrollierte Studien (RCTs), die die Wirksamkeit und Verträglichkeit von Etoricoxib 30–60 mg, Celecoxib 200–400 mg und Naproxen 1000 mg untersucht haben, wurden auf Grundlage der Anzahl von Ausschlüssen unter Patienten mit OA in diese Netzwerkmetaanalyse einbezogen. Wir haben eine Netzwerkmetaanalyse nach bayesschen Random Effects durchgeführt, um die direkte und indirekte Evidenz von den RCTs zu kombinieren.
Ergebnisse
Acht RCTs mit 5942 Patienten haben die Einschlusskriterien erfüllt. Der Anteil von Patientenausschlüssen wegen mangelnder Wirksamkeit war in den Gruppen mit Etoricoxib 30–60 mg (OR 0,21, 95 % CrI 0,12–0,38), Celecoxib 200–400 mg (OR 0,29, 95 % CrI 0,18–0,47) und Naproxen 1000 mg (OR 0,31, 95 % CrI 0,18–0,51) signifikant niedriger als in der Placebogruppe. Die Anzahl von Patientenausschlüssen wegen mangelnder Wirksamkeit hatte in der Gruppe mit Etoricoxib 30–60 mg eine niedrigere Tendenz als in den Gruppen mit Naproxen 1000 mg und Celecoxib 200–400 mg, obwohl sie keine statistische Signifikanz erreichte (OR 0,68, 95 % CrI 0,36–1,33 bzw. OR 0,70, 95 % CrI 0,38–1,37). Die Ranking-Wahrscheinlichkeiten aufgrund der SUCRA („surface under the cumulative ranking curve“) zeigen, dass Etoricoxib 30–60 mg auf Grundlage der Zahl von Ausschlüssen wegen mangelnder Wirksamkeit (SUCRA = 0,9168) mit höchster Wahrscheinlichkeit die beste Behandlung ist, danach folgen Celecoxib 200–400 mg (SUCRA = 0,5659), Naproxen 1000 mg (SUCRA = 0,5171) und das Placebo (SUCRA = 0,000189). Hinsichtlich der Verträglichkeit war die Zahl der Ausschlüsse wegen Nebenwirkungen zwischen Etoricoxib, Celecoxib, Naproxen und Placebo nicht signifikant unterschiedlich, auch wenn sie bei Etoricoxib und beim Placebo eine niedrigere Tendenz hatte.
Schlussfolgerungen
Etoricoxib 30–60 mg, Celecoxib 200–400 mg und Naproxen 1000 mg waren wirksamer als das Placebo. Es gab jedoch keinen signifikanten Unterschied in der Wirksamkeit und Verträglichkeit zwischen den Medikamenten.



Similar content being viewed by others
References
Dieppe PA, Lohmander LS (2005) Pathogenesis and management of pain in osteoarthritis. Lancet 365:965–973
Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, Towheed T, Welch V, Wells G, Tugwell P (2012) American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 64:465–474
Mizuno K, Yamamoto S, Lands W (1982) Effects of non-steroidal anti-inflammatory drugs on fatty acid cyclooxygenase and prostaglandin hydroperoxidase activities. Prostaglandins 23:743
Gabriel SE, Jaakkimainen L, Bombardier C (1991) Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs: a meta-analysis. Ann Intern Med 115:787–796
Silverstein FE, Faich G, Goldstein JL, Simon LS, Pincus T, Whelton A, Makuch R, Eisen G, Agrawal NM, Stenson WF (2000) Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. JAMA 284:1247–1255
Curtis SP, Bockow B, Fisher C, Olaleye J, Compton A, Ko AT, Reicin AS (2005) Etoricoxib in the treatment of osteoarthritis over 52-weeks: a double-blind, active-comparator controlled trial. Bmc Musculoskelet Disord 6:58 (NCT00242489)
Yoo MC, Yoo WH, Kang SB, Park Y-W, Kim SS, Moon KH, Song YW, Min BW, Cho YJ, Moon S-H (2014) Etoricoxib in the treatment of Korean patients with osteoarthritis in a double-blind, randomized controlled trial. Curr Med Res Opin 30:2399–2408
Bingham C, Sebba A, Rubin B, Ruoff G, Kremer J, Bird S, Smugar S, Fitzgerald B, O’Brien K, Tershakovec A (2007) Efficacy and safety of etoricoxib 30 mg and celecoxib 200 mg in the treatment of osteoarthritis in two identically designed, randomized, placebo-controlled, non-inferiority studies. Rheumatology 46:496–507
Reginster J-Y, Malmstrom K, Mehta A, Bergman G, Ko A, Curtis S, Reicin A (2007) Evaluation of the efficacy and safety of etoricoxib compared with naproxen in two, 138-week randomised studies of patients with osteoarthritis. Ann Rheum Dis 66:945–951
Kongtharvonskul J, Anothaisintawee T, McEvoy M, Attia J, Woratanarat P, Thakkinstian A (2015) Efficacy and safety of glucosamine, diacerein, and NSAIDs in osteoarthritis knee: a systematic review and network meta-analysis. Eur J Med Res 20:24
Choy E, Smith C, Dore C, Scott D (2005) A meta-analysis of the efficacy and toxicity of combining disease-modifying anti-rheumatic drugs in rheumatoid arthritis based on patient withdrawal. Rheumatology 44:1414–1421
Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, Pitkin R, Rennie D, Schulz KF, Simel D (1996) Improving the quality of reporting of randomized controlled trials: the CONSORT statement. JAMA 276:637–639
Ravindran V, Scott D, Choy E (2008) A systematic review and meta-analysis of efficacy and toxicity of disease modifying anti-rheumatic drugs and biological agents for psoriatic arthritis. Ann Rheum Dis 67:855–859
Lee YH, Bae SC, Choi SJ, Ji JD, Song GG (2011) Associations between vitamin D receptor polymorphisms and susceptibility to rheumatoid arthritis and systemic lupus erythematosus: a meta-analysis. Mol Biol Rep 38:3643–3651
Lee YH, Rho YH, Choi SJ, Ji JD, Song GG (2007) PADI4 polymorphisms and rheumatoid arthritis susceptibility: a meta-analysis. Rheumatol Int 27:827–833
Catalá-López F, Tobías A, Cameron C, Moher D, Hutton B (2014) Network meta-analysis for comparing treatment effects of multiple interventions: an introduction. Rheumatol Int 34:1489–1496
Caldwell DM, Ades A, Higgins J (2005) Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ 331:897
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264–269
Brown S, Hutton B, Clifford T, Coyle D, Grima D, Wells G, Cameron C (2014) A Microsoft-Excel-based tool for running and critically appraising network meta-analyses--an overview and application of NetMetaXL. Syst Rev 3:110
Salanti G, Ades A, Ioannidis JP (2011) Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 64:163–171
Yoo MC, Yoo WH, Kang SB, Park YW, Kim SS, Moon KH, Song YW, Min BW, Cho YJ, Moon SH, Bin SI, Baek HJ, Shim SC, Lee SW, Yoo DH, Mehta A, Skuban A, Cukrow DM, Vandormael K, Yan L (2014) Etoricoxib in the treatment of Korean patients with osteoarthritis in a double-blind, randomized controlled trial. Curr Med Res Opin 30:2399–2408
Bingham CO 3rd, Sebba AI, Rubin BR, Ruoff GE, Kremer J, Bird S, Smugar SS, Fitzgerald BJ, O’Brien K, Tershakovec AM (2007) Efficacy and safety of etoricoxib 30 mg and celecoxib 200 mg in the treatment of osteoarthritis in two identically designed, randomized, placebo-controlled, non-inferiority studies. Rheumatology 46:496–507
Lisse J, Espinoza L, Zhao SZ, Dedhiya SD, Osterhaus JT (2001) Functional status and health-related quality of life of elderly osteoarthritic patients treated with celecoxib. The journals of gerontology Series A. Biol Sci Med Sci 56:M167–175
Bensen WG, Fiechtner JJ, McMillen JI, Zhao WW, Yu SS, Woods EM, Hubbard RC, Isakson PC, Verburg KM, Geis GS (1999) Treatment of osteoarthritis with celecoxib, a cyclooxygenase-2 inhibitor: a randomized controlled trial. Mayo Clin Proc 74:1095–1105
Kivitz AJ, Moskowitz RW, Woods E, Hubbard RC, Verburg KM, Lefkowith JB, Geis GS (2001) Comparative efficacy and safety of celecoxib and naproxen in the treatment of osteoarthritis of the hip. J Int Med Res 29:467–479
Leung AT, Malmstrom K, Gallacher AE, Sarembock B, Poor G, Beaulieu A, Castro R, Sanchez M, Detora LM, Ng J (2002) Efficacy and tolerability profile of etoricoxib in patients with osteoarthritis: A randomized, double-blind, placebo and active-comparator controlled 12-week efficacy trial. Curr Med Res Opin 18:49–58
Reginster JY, Malmstrom K, Mehta A, Bergman G, Ko AT, Curtis SP, Reicin AS (2007) Evaluation of the efficacy and safety of etoricoxib compared with naproxen in two, 138-week randomised studies of patients with osteoarthritis. Ann Rheum Dis 66:945–951
Essex MN, Bhadra P, Sands GH (2012) Efficacy and tolerability of celecoxib versus naproxen in patients with osteoarthritis of the knee: a randomized, double-blind, double-dummy trial. J Int Med Res 40:1357–1370
Lee YH, Woo J-H, Choi SJ, Ji JD, Song GG (2010) Effect of glucosamine or chondroitin sulfate on the osteoarthritis progression: a meta-analysis. Rheumatol Int 30:357–363
Moore A, Makinson G, Li C (2013) Patient-level pooled analysis of adjudicated gastrointestinal outcomes in celecoxib clinical trials: meta-analysis of 51,000 patients enrolled in 52 randomized trials. Arthritis Res Ther 15:R6
Ramey DR, Watson DJ, Yu C, Bolognese JA, Curtis SP, Reicin AS (2005) The incidence of upper gastrointestinal adverse events in clinical trials of etoricoxib vs. non-selective NSAIDs: an updated combined analysis. Curr Med Res Opin 21:715–722
Varas‐Lorenzo C, Riera‐Guardia N, Calingaert B, Castellsague J, Salvo F, Nicotra F, Sturkenboom M, Perez‐Gutthann S (2013) Myocardial infarction and individual nonsteroidal anti‐inflammatory drugs meta‐analysis of observational studies. Pharmacoepidemiol Drug Saf 22:559–570
Lindhardsen J, Gislason GH, Jacobsen S, Ahlehoff O, Olsen AM, Madsen OR, Torp-Pedersen C, Hansen PR (2013) Non-steroidal anti-inflammatory drugs and risk of cardiovascular disease in patients with rheumatoid arthritis: a nationwide cohort study. Ann Rheum Dis 73:1515–1521. doi:10.1136/annrheumdis-2012-203137
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G.G. Song, Y.H. Seo, J.‑H. Kim, S.J. Choi, J.D. Ji and Y.H. Lee state that there are no conflicts of interest.
The accompanying manuscript does not include studies on humans or animals.
Rights and permissions
About this article
Cite this article
Song, G.G., Seo, Y.H., Kim, JH. et al. Relative efficacy and tolerability of etoricoxib, celecoxib, and naproxen in the treatment of osteoarthritis . Z Rheumatol 75, 508–516 (2016). https://doi.org/10.1007/s00393-015-0023-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-015-0023-9