Abstract
Purpose
We aimed to present the factors associated with lymph node harvest (LNH) and seek whether surgical quality control measures can improve LNH.
Methods
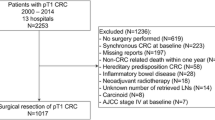
From a prospectively collected data at a single institution, 874 CRC patients who underwent curative surgery between 2004 and 2013 were included. Factor and survival analyses were performed regarding LNH. Subgroup analysis was performed according to LNH group (LNH ≥ 12 vs LNH < 12) and year of surgery (2004–2008, 2009–2011, and 2012–2013 group).
Results
In the multivariate analysis, tumor location (OR 0.6, p < 0.001), stage (OR 1.95, p < 0.001), and year of surgery (OR 3.86, p < 0.001) showed an association with adequate LNH. In the subgroup analysis categorized by the year of surgery, surgical quality control measures by standardized laparoscopic surgery (OR 52.91, p < 0.001) showed notable association with adequate LNH. Comparing the 2009–2011 and 2012–2013 group, the national quality assessment program additionally improved adequate LNH percentage (83.9 vs 94.3%). In the survival analysis, disease-free survival (DFS) differed according to year of surgery, standardized laparoscopic surgery with high vascular ligation, and adequate LNH by stage. In the overall survival (OS) analysis, the LNH-related factors did not show significant difference.
Conclusions
Through standardized laparoscopic surgery with high vascular ligation and national quality assessment program, surgical quality control had a positive impact on the increase of adequate LNH. Improving the modifiable LNH factors resulted in the enhancement of adequate LNH and related DFS.


Similar content being viewed by others

References
(1990) NIH consensus conference. Adjuvant therapy for patients with colon and rectal cancer. JAMA 264(11):1444–1450
Chen SL, Bilchik AJ (2006) More extensive nodal dissection improves survival for stages I to III of colon cancer: a population-based study. Ann Surg 244(4):602–610
Goldstein NS (2002) Lymph node recoveries from 2427 pT3 colorectal resection specimens spanning 45 years: recommendations for a minimum number of recovered lymph nodes based on predictive probabilities. Am J Surg Pathol 26(2):179–189
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ et al (2003) Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 21(15):2912–2919
Chen HH, Chakravarty KD, Wang JY, Changchien CR, Tang R (2010) Pathological examination of 12 regional lymph nodes and long-term survival in stages I-III colon cancer patients: an analysis of 2,056 consecutive patients in two branches of same institution. Int J Color Dis 25(11):1333–1341
Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA (2007) Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst 99(6):433–441
Porter GA, Urquhart R, Bu J, Johnson P, Grunfeld E (2011) The impact of audit and feedback on nodal harvest in colorectal cancer. BMC Cancer 11:2
Larson DW, Marcello PW, Larach SW, Wexner SD, Park A, Marks J et al (2008) Surgeon volume does not predict outcomes in the setting of technical credentialing: results from a randomized trial in colon cancer. Ann Surg 248(5):746–750
Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A et al (2007) Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg 142(3):298–303
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W et al (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol 30(15):1763–1769
Slanetz CA Jr, Grimson R (1997) Effect of high and intermediate ligation on survival and recurrence rates following curative resection of colorectal cancer. Dis Colon Rectum 40(10):1205–1219
Lujan J, Valero G, Hernandez Q, Sanchez A, Frutos MD, Parrilla P (2009) Randomized clinical trial comparing laparoscopic and open surgery in patients with rectal cancer. Br J Surg 96(9):982–989
Evans MD, Barton K, Rees A, Stamatakis JD, Karandikar SS (2008) The impact of surgeon and pathologist on lymph node retrieval in colorectal cancer and its impact on survival for patients with Dukes’ stage B disease. Color Dis 10(2):157–164
Law CH, Wright FC, Rapanos T, Alzahrani M, Hanna SS, Khalifa M et al (2003) Impact of lymph node retrieval and pathological ultra-staging on the prognosis of stage II colon cancer. J Surg Oncol 84(3):120–126
Sjo OH, Merok MA, Svindland A, Nesbakken A (2012) Prognostic impact of lymph node harvest and lymph node ratio in patients with colon cancer. Dis Colon Rectum 55(3):307–315
Stocchi L, Fazio VW, Lavery I, Hammel J (2011) Individual surgeon, pathologist, and other factors affecting lymph node harvest in stage II colon carcinoma. Is a minimum of 12 examined lymph nodes sufficient? Ann Surg Oncol 18(2):405–412
Nedrebø BS, Søreide K, Nesbakken A, Eriksen MT, Søreide JA, Kørner H (2013) Risk factors associated with poor lymph node harvest after colon cancer surgery in a national cohort. Color Dis 15(6):e301–e308
Ha YH, Jeong SY, Lim SB, Choi HS, Hong YS, Chang HJ et al (2010) Influence of preoperative chemoradiotherapy on the number of lymph nodes retrieved in rectal cancer. Ann Surg 252(2):336–340
Wang J, Kulaylat M, Rockette H, Hassett J, Rajput A, Dunn KB et al (2009) Should total number of lymph nodes be used as a quality of care measure for stage III colon cancer? Ann Surg 249(4):559–563
Vather R, Sammour T, Kahokehr A, Connolly AB, Hill AG (2009) Lymph node evaluation and long-term survival in stage II and stage III colon cancer: a national study. Ann Surg Oncol 16(3):585–593
Chou JF, Row D, Gonen M, Liu YH, Schrag D, Weiser MR (2010) Clinical and pathologic factors that predict lymph node yield from surgical specimens in colorectal cancer: a population-based study. Cancer 116(11):2560–2570
Boutros M, Hippalgaonkar N, Silva E, Allende D, Wexner SD, Berho M (2013) Laparoscopic resection of rectal cancer results in higher lymph node yield and better short-term outcomes than open surgery: a large single-center comparative study. Dis Colon Rectum 56(6):679–688
Horne J, Bateman AC, Carr NJ, Ryder I (2014) Lymph node revealing solutions in colorectal cancer: should they be used routinely? J Clin Pathol 67(5):383–388
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The manuscript was in accordance with the ethical standards of the institutional research board and with the 1964 Helsinki declaration.
Conflicts of interest
The authors declare that they have no conflict of interest.
Funding
This study did not have any external funding.
Rights and permissions
About this article
Cite this article
Won, D.D., Choi, S.B., Lee, Y.S. et al. The positive impact of surgical quality control on adequate lymph node harvest by standardized laparoscopic surgery and national quality assessment program in colorectal cancer. Int J Colorectal Dis 32, 975–982 (2017). https://doi.org/10.1007/s00384-017-2771-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2771-2