Abstract
Purpose
Sigmoid resection for diverticulitis is usually the first procedure performed when starting the learning process for laparoscopic colorectal surgery. The aim of this study is to evaluate the difficulty of laparoscopic sigmoid resection for diverticulitis in comparison to sigmoid malignancy in order to assess its role in the residents training program.
Methods
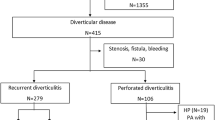
A cohort of patients was selected who suffered either from malignancy or recurrent diverticulitis in the sigmoid colon. Laparoscopic sigmoid resection was performed. The degree of difficulty was assessed by intraoperative complications and intraoperative technical challenges. Furthermore, take-overs from assistant to surgeon, surgeon to surgeon, and conversion were reported.
Results
A total of 224 patients were included, 119 (53.1%) men and 105 (46.9%) women.
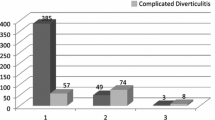
Patients suffering from diverticulitis had significantly less co-morbidities than those with malignancies. In the diverticulitis group, there were significantly more technical challenges. There was a higher rate in take-overs from residents (p = 0.02) as well as surgeon to surgeon (p = 0.04). The rate of conversions was also significantly higher in the diverticulitis group (p = 0.03) when compared to the malignancy group.
Conclusions
The outcomes of our study show that diverticulitis may not be the ideal condition to start the learning process for laparoscopic colorectal surgery.
Similar content being viewed by others
References
Bosker R, Hoogenboom F, Groen H, Hoff C, Ploeg R, Pierie JP (2013) Early learning effect of residents for laparoscopic sigmoid resection. J Surg 70:200–205
Leong S, Cahill RA, Mehigan BJ, Stephens RB (2007) Considerations on the learning curve for laparoscopic colorectal surgery: a view from the bottom. Int J Color Dis 22(9):1109–1115
Klarenbeek BR, Veenhof AA, Bergamaschi R et al (2009) Laparoscopic sigmoid resection for diverticulitis decreases major comorbidity rates: a randomized control trial: short term results of the Sigma Trial. Ann Surg 249:39–44
Klingensmith ME, Lewis FR (2013) General surgery residency training issues. Adv Surg 47:251–270
Holmer C, Lehmann KS, Engelmann S et al (2011) Long-term outcome after conservative and surgical treatment of acute sigmoid diverticulitis. Langenbeck's Arch Surg 396(6):825–832
Rafferty J, Shellito P, Hyman NH et al (2006) Standards Committee of American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon rectum 49:939–944
Andeweg CS, Felt-Bersma R, Verbon A et al (2013) Summary of the practice guideline on diverticulitis in the colon: diagnostics and treatment in specialty care. Ned TijdschrGeneeskd 157(15):A6124
Naguib N, Masoud A (2013) Laparoscopic colorectal surgery for diverticular disease is not suitable for the early part of the learning curve. A retrospective cohort study. Int J Surg 11(10):1092–1096
Quan H, Li B, Couris CM et al (2011) Updating and validating the Charlson Comorbidity Index and Score for risk asjustment in hospital discharge abtracts using data from 6 countries. Am J Epidemiol 173:676–682
Schwandner O, Farke S, Bruch HP (2005) Laparoscopic colectomy for diverticulitis is not associated with increased morbidity when compared with non-diverticular disease. Int J Color Dis 20(2):165–172
Lee SW (2009) Laparoscopic procedures for colon and rectal surgery. Clin Colon Rectal Surg 22(4):218–224
Nedrebo BS, Soreide K, Nesbakken A et al (2013) Risk factors associated with poor lymph node harvest after colon cancer surgery in a national cohort. Color Dis 15:e301–e308
Veen T, Nedrebo BS, Stormark K et al (2013) Qualitive and quantitive issues of lymph nodes as prognostic factors in colon cancer. Dig Surg 30(1):1–11
Yacoub M, Swistak S, Chan S et al (2013) Factors that influence lymph node retrieval in the surgical treatment of colorectal cancer: a comparison of the laparoscopic versus open approach. Am J Surg 205(3):339–342
Bamboat ZM, Deperalta D, Dursun A, Berger DL, Bordeianou L (2011) Factors affecting lymph node yield from patients undergoing colectomy for cancer. Int J Color Dis 26(9):1163–1168
Akmal Y, Bailey C, Baek J, Metchikian M, Pigazzi A (2011) Oncological outcomes of laparoscopic colon resection for cancer after implementation of a full-time preceptorship. Surg Endosc 25:2967–2971
Alves A, Panis Y, Mathieu P et al Prospective mortality and morbidity in French patients undergoing colorectal surgey: results of a prospective multicenter study. Arch Surg 140(3):278–283
Kirchhoff P, Clavien PA, Hahnloser D (2010) Complications in colorectal surgery: risk factors and preventive strategies. Patient Saf Surg 4:5
Kirchhoff P, Matz D, Dincler S et al (2011) Predictive risk factor for intra- and postoperative complications in 526 laparoscopic sigmoid resections due to recurrent diverticulitis: a multivariate analysis. World J Surg 35:677–683
Acknowledgements
The authors would like to thank the department of surgery and anesthesiology from the Meander Medical Center for their cooperation in this study.
Authors’ contribution
MAW Stam: Study design, data collection, data analysis and interpretation, and writing of the manuscript.
WA Draaisma: Study design, data interpretation, and writing of the manuscript.
PCM Pasker: Study design, data analysis, and data interpretation.
ECJ Consten: Study design, data interpretation, and writing of the manuscript.
IAMJ Broeders: Study design, data interpretation, and writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Meander Medical Centre ethical board. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Stam, M., Draaisma, W., Pasker, P. et al. Sigmoid resection for diverticulitis is more difficult than for malignancies. Int J Colorectal Dis 32, 891–896 (2017). https://doi.org/10.1007/s00384-017-2756-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2756-1