Abstract
Background
There is no good prognostic indicator for biliary atresia (BA). We reviewed liver biopsies taken during the initial procedure to find a prognostic marker.
Methods
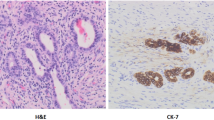
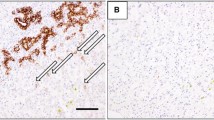
Thirty-two BA cases underwent Kasai operation from 1976 to 2009. We compared two groups at 1, 3, and 9 years. Group A required liver transplantation or died. Group B survived with their native liver. Biopsies were analyzed for liver fibrosis, portal-central vein bridging (P–C bridging), ductal plate malformation (DPM) and the number of the bile ducts in portal canal/measured surface area of the portal canal (BDP ratio). Statistical comparisons of the multiple data were evaluated by Mann–Whitney U test, Student’s t test and Pearson’s Chi-square test. Regression analysis with P < 0.05 was considered significant.
Results
BDP ratios (/mm2) were 2.4 ± 1.5 in Group A1 (n = 9) vs 4.6 ± 2.4 in Group B1 (n = 23) (P = 0.01); 2.6 ± 1.4 in Group A3 (n = 14) vs 5.1 ± 2.5 in Group B3 (n = 18) (P < 0.01), 3.0 ± 2.2 in Group A9 (n = 15) vs 4.9 ± 2.5 in Group B9 (n = 15) (P < 0.05). There was no significant difference in any other finding.
Conclusion
The BDP ratio is a sound prognostic indicator in BA.





Similar content being viewed by others
References
Suruga K, Nagashima K, Kono S et al (1972) A clinical and pathological study of congenital biliary atresia. J Pediatr Surg 7:655–659
Baruah RR, Bhatnagar V, Agarwala S et al (2015) Correlation of pre- and post-operative liver function, duct diameter at porta hepatis, and portal fibrosis with surgical outcomes in biliary atresia. J Indian Assoc Pediatr Surg 20:184–188
Mukhopadhyay SG, Roy P, Chatterjee U et al (2014) A histopathological study of liver and biliary remnants in the long-term survivors (>10 years) of cases of biliary atresia. Indian J Pathol Microbiol 57:380–385
Weerasooriya VS, White FV, Shepherd RW (2004) Hepatic fibrosis and survival in biliary atresia. J Pediatr 144:123–125
Tomita H, Masugi Y, Hoshino K et al (2014) Long-term native liver fibrosis in biliary atresia: development of a novel scoring system using histology and standard liver tests. J Hepatol 60:1242–1248
Xiao JC, Ruck P, Kaiserling E (1999) Small epithelial cells in extrahepatic biliary atresia: electron microscopic and immunoelectron microscopic findings suggest a close relationship to liver progenitor cells. Histopathology 35:454–460
Oi R, Kasai M, Takahashi T (1969) Intrahepatic biliary obstruction in congenital bile duct atresia. Tohoku J Exp Med 99:129–149
Chiba T, Kasai M, Sasano N (1975) Reconstruction of intrahepatic bile ducts in congenital biliary atresia. Tohoku J Exp Med 115:99–110
Chiba T (1977) Histopathological studies on the prognosis of biliary atresia. Tohoku J Exp Med 122:249–258
Tagge DU, Tagge EP, Drongowski RA et al (1991) A long-term experience with biliary atresia. Reassessment of prognostic factors. Ann Surg 214:590–598
Patrick RS, McGEE JO’D (1980) Biopsy pathology of the liver. Chapman and Hall, London
Nakamura H, Koga H, Wada M et al (2012) Reappraising the portoenterostomy procedure according to sound physiologic/anatomic principles enhances postoperative jaundice clearance in biliary atresia. Pediatr Surg Int 28:205–209
Pape L, Olsson K, Petersen C et al (2009) Prognostic value of computerized quantification of liver fibrosis in children with biliary atresia. Liver Transpl 15:876–882
Roskams TA, Theise ND, Balabaud C et al (2004) Nomenclature of the finer branches of the biliary tree: canals, ductules, and ductular reactions in human livers. Hepatology 39:1739–1745
Desmet VJ (1998) Ludwig symposium on biliary disorders–part I. Pathogenesis of ductal plate abnormalities. Mayo Clin Proc 73:80–89
Pacheco MC, Campbell KM, Bove KE (2009) Ductal plate malformation-like arrays in early explants after a Kasai procedure are independent of splenic malformation complex (heterotaxy). Pediatr Dev Pathol 12:355–360
Safwan M, Ramachandran P, Vij M et al (2015) Impact of ductal plate malformation on survival with native liver in children with biliary atresia. Pediatr Surg Int 31:837–843
Hartley JL, Davenport M, Kelly DA (2009) Biliary atresia. Lancet 374:1704–1713
Acknowledgments
The authors thank Shigeko Ohnuma and the other staffs in the Department of Pathology in St. Marianna University school of Medicine for assistance in processing the histology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Obayashi, J., Tanaka, K., Ohyama, K. et al. Relation between amount of bile ducts in portal canal and outcomes in biliary atresia. Pediatr Surg Int 32, 833–838 (2016). https://doi.org/10.1007/s00383-016-3941-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3941-y