Abstract
Purpose
Each year, nearly 1 million children in the USA are victims of non-accidental trauma (NAT). Missed diagnosis or poor case management often leads to repeat/escalation injury. Victims of recurrent NAT are at higher risk for severe morbidity and mortality resulting from abuse. The objective of this review is to describe the evolution and implementation of this tool and evaluate our institutional response to NAT prior to implementation.
Methods
A systematic guideline for the evaluation of pediatric patients in which NAT is suspected or confirmed was developed and implemented at a level II pediatric trauma hospital. To understand the state of our institution prior to implementation of the guideline, a review of 117 confirmed NAT cases at our hospital over the prior 4 years was conducted.
Results
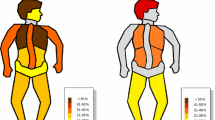
In the absence of a systematic management guideline, important and relevant social and family history red flags were often missing in the initial evaluation. Patients with perineal bruising experienced significantly higher mortality than patients without perineal bruising (27.3 vs. 5.7 %; p = 0.03) and were significantly more likely to require surgery (45.5 vs. 14.2 %; p = 0.02).
Conclusion
Development and implementation of a standardized tool for the differentiation and diagnosis of NAT and creation of a structured electronic medical record note should improve the description and documentation of child abuse cases in a community hospital setting. A retrospective analysis demonstrated that in the absence of such a tool, management of NAT may be inconsistent or incomplete. Perineal injury is an especially ominous red flag finding.



Similar content being viewed by others
References
US Department of Health and Human Services (2013) Child Maltreatment Children’s Bureau Administration for Children, Youth, and Families
Wang C-T, Holton J, America PCA (2007). Total estimated cost of child abuse and neglect in the United States, Citeseer
Roach JP, Acker SN, Bensard DD, Sirotnak AP, Karrer FM, Partrick DA (2014) Head injury pattern in children can help differentiate accidental from non-accidental trauma. Pediatr Surg Int 30(11):1103–1106
Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC (1999) Analysis of missed cases of abusive head trauma. JAMA 281(7):621–626
Larimer EL, Fallon SC, Westfall J, Frost M, Wesson DE, Naik-Mathuria BJ (2013) The importance of surgeon involvement in the evaluation of non-accidental trauma patients. J Pediatr Surg 48(6):1357–1362
Deans KJ, Thackeray J, Askegard-Giesmann JR, Earley E, Groner JI, Minneci PC (2013) Mortality increases with recurrent episodes of nonaccidental trauma in children. J Trauma Acute Care Surg 75(1):161–165
Martrille L, Cattaneo C, Dorandeu A, Baccino E (2006) A multicentre and prospective study of suspected cases of child physical abuse. Int J Legal Med 120(2):73–78
Hurme T, Alanko S, Anttila P, Juven T, Svedstrom E (2008) Risk factors for physical child abuse in infants and toddlers. Eur J Pediatr Surg 18(6):387–391
R Core Team (2013) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/
Deans KJ, Minneci PC, Lowell W, Groner JI (2013) Increased morbidity and mortality of traumatic brain injury in victims of nonaccidental trauma. J Trauma Acute Care Surg 75(1):157–160
Pierce MC, Kaczor K, Aldridge S, O’Flynn J, Lorenz DJ (2010) Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics 125(1):67–74
Naik-Mathuria B, Akinkuotu A, Wesson D (2015) Role of the surgeon in non-accidental trauma. Pediatr Surg Int 31(7):605–610
Acknowledgments
This work was funded by the MultiCare Institute for Research and Innovation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Escobar, M.A., Pflugeisen, B.M., Duralde, Y. et al. Development of a systematic protocol to identify victims of non-accidental trauma. Pediatr Surg Int 32, 377–386 (2016). https://doi.org/10.1007/s00383-016-3863-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3863-8