Abstract
Purpose
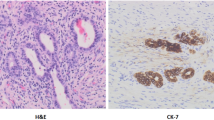
Ductal plate malformation (DPM) like arrays in the liver which resemble the characteristic persistent embryonal ductular structures have been shown to adversely affect the outcome of Kasai portoenterostomy (KPE) in biliary atresia (BA). We studied the impact of DPM on survival with native liver (SNL) in children with BA who underwent liver transplantation (LT) after KPE as well as those who underwent primary LT without KPE.
Methods
Records of children with BA who underwent LT in our institute were reviewed and divided into three groups—Group 1 had primary LT because of delayed diagnosis of BA and synthetic liver failure, Group 2 had LT for synthetic liver failure after a failed KPE, and Group 3 had LT despite clearing jaundice after KPE for other indications. The impact of DPM on SNL was analyzed using standard statistical means.
Results
In Group 1 (n = 26) and Group 2 (n = 26), the incidence of DPM was high and was associated with a significantly shorter SNL compared to children with no DPM. The incidence of DPM was significantly lower in Group 3 (n = 13).
Conclusion
DPM shortens SNL and influences the pathogenesis of disease progression in children with BA who had synthetic liver failure requiring transplantation either because of a failed KPE or due to a delay in diagnosis. Its incidence is low in children who cleared jaundice after KPE and needed transplantation for other indications at a later age. The presence of DPM signifies an adverse outcome for the disease.






Similar content being viewed by others
References
Davenport M, Tizzard SA, Underhill J, Mieli-Vergani G, Portmann B, Hadzic N (2006) The biliary atresia splenic malformation syndrome: a 28-year single-center retrospective study. J Pediatr 149:393–400. doi:10.1016/j.jpeds.2006.05.030
Desmet VJ (1998) Ludwig symposium on biliary disorders–part I. Pathogenesis of ductal plate abnormalities. Mayo Clin Proc 73:80–89
Low Y, Vijayan V, Tan CE (2001) The prognostic value of ductal plate malformation and other histologic parameters in biliary atresia: an immunohistochemical study. J Pediatr 139:320–322. doi:10.1067/mpd.2001.117003
Pacheco MC, Campbell KM, Bove KE (2009) Ductal plate malformation-like arrays in early explants after a Kasai procedure are independent of splenic malformation complex (heterotaxy). Pediatr Dev Pathol 12:355–360. doi:10.2350/09-01-0598-OA.1
Vukovic J, Grizelj R, Bojanic K, Coric M, Luetic T, Batinica S, Kujundzic-Tiljak M, Schroeder DR, Sprung J (2012) Ductal plate malformation in patients with biliary atresia. Eur J Pediatr 171:1799–1804. doi:10.1007/s00431-012-1820-7
Redston MS, Wanless IR (1996) The hepatic von Meyenburg complex: prevalence and association with hepatic and renal cysts among 2843 autopsies [corrected]. Mod Pathol 9:233–237
Shimadera S, Iwai N, Deguchi E, Kimura O, Ono S, Fumino S, Higuchi K (2008) Significance of ductal plate malformation in the postoperative clinical course of biliary atresia. J Pediatr Surg 43:304–307. doi:10.1016/j.jpedsurg.2007.10.023
Arii R, Koga H, Arakawa A, Miyahara K, Lane GJ, Okazaki T, Urao M, Yamataka A (2011) How valuable is ductal plate malformation as a predictor of clinical course in postoperative biliary atresia patients? Pediatr Surg Int 27:275–277. doi:10.1007/s00383-010-2793-0
Davenport M, Ville De, de Goyet J, Stringer MD, Mieli-Vergani G, Kelly DA, McClean P, Spitz L (2004) Seamless management of biliary atresia in England and Wales (1999–2002). Lancet 363:1354–1357. doi:10.1016/S0140-6736(04)16045-5
Lampela H, Ritvanen A, Kosola S, Koivusalo A, Rintala R, Jalanko H, Pakarinen M (2012) National centralization of biliary atresia care to an assigned multidisciplinary team provides high-quality outcomes. Scand J Gastroenterol 47:99–107. doi:10.3109/00365521.2011.627446
Fain JS, Lewin KJ (1989) Intrahepatic biliary cysts in congenital biliary atresia. Arch Pathol Lab Med 113:1383–1386
Dillon P, Belchis D, Tracy T, Cilley R, Hafer L, Krummel T (1994) Increased expression of intercellular adhesion molecules in biliary atresia. Am J Pathol 145:263–267
Takahashi A, Tsuchida Y, Hatakeyama S, Suzuki N, Kuroiwa M, Ikeda H, Hirado J, Kitamura T, Matsuyama S (1997) A peculiar form of multiple cystic dilatation of the intrahepatic biliary system found in a patient with biliary atresia. J Pediatr Surg 32:1776–1779
Tsuchida Y, Honna T, Kawarasaki H (1994) Cystic dilatation of the intrahepatic biliary system in biliary atresia after hepatic portoenterostomy. J Pediatr Surg 29:630–634
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Safwan, M., Ramachandran, P., Vij, M. et al. Impact of ductal plate malformation on survival with native liver in children with biliary atresia. Pediatr Surg Int 31, 837–843 (2015). https://doi.org/10.1007/s00383-015-3728-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3728-6