Abstract
Purpose
We aimed to evaluate the rate and examine potential predictors of subsequent anti-reflux procedures in a population undergoing percutaneous endoscopic gastrostomy (PEG) insertion.
Materials
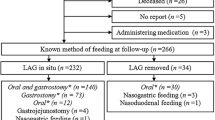
We retrospectively reviewed the pre- and post-operative clinical course of patients undergoing PEG insertion over a 10-year period with respect to indication, underlying co-morbidity, and GER investigation and management.
Results
We reviewed data on 170 patients. Neurological disability (e.g., cerebral palsy) was the most common underlying condition in those undergoing PEG insertion (n = 104) followed by cystic fibrosis (n = 29). Oropharyngeal dysphagia and failure to thrive were the commonest indications for PEG. Eight patients (4.7 %) reported increased frequency of vomiting after PEG, 6 (75 %) of whom had a pre-operative diagnosis of GER. Two (25 %) patients from this sub-group subsequently required anti-reflux surgery. Patient’s with neurological disease were not at increased risk of new-onset GER or increased vomiting following PEG insertion compared to those with non-neurological conditions (p = 0.259). In total, 8 (4.7 %) and 7 (4.1 %) patients underwent fundoplication and gastrojejunal tube insertion, respectively.
Conclusions
PEG insertion does not appear to induce symptomatic gastro-oesophageal reflux in the majority of children, suggesting that in the majority of cases, a concurrent anti-reflux procedure is unnecessary. Parents should be counseled accordingly.

Similar content being viewed by others
References
Van Biervliet S, Van Renterghem K, Vande Putte D, Vande Velde S, De Bruyne R, Van Winckel M (2014) Gastrostomy use in children: a 3-year single centre experience. Acta Gastroenterol Belg 77(1):8–12
Minar P, Garland J, Martinez A, Werlin S (2011) Safety of percutaneous endoscopic gastrostomy in medically complicated infants. J Pediatr Gastroenterol Nutr 53(3):293–295. doi:10.1097/MPG.0b013e318215c41b
Saitua F, Acuna R, Herrera P (2003) Percutaneous endoscopic gastrostomy: the technique of choice? J Pediatr Surg 38(10):1512–1515
Akay B, Capizzani TR, Lee AM, Drongowski RA, Geiger JD, Hirschl RB, Mychaliska GB (2010) Gastrostomy tube placement in infants and children: is there a preferred technique? J Pediatr Surg 45(6):1147–1152. doi:10.1016/j.jpedsurg.2010.02.079
Fox D, Barnard J, Campagna EJ, Dickinson LM, Bruny J, Kempe A (2012) Fundoplication and the pediatric surgeon: implications for shared decision-making and the medical home. Acad Pediatr 12(6):558–566. doi:10.1016/j.acap.2012.07.006
Toporowska-Kowalska E, Gebora-Kowalska B, Fendler W, Popinska K, Szlagatys-Sidorkiewicz A, Grzybowska-Chlebowczyk U, Wiernicka A, Borkowska A, Sibilska M, Wiecek S, Hapyn E, Kierkus J (2013) Diagnosis of gastroesophageal reflux and anti-reflux procedures among Polish children with gastrostomies: a 10-year nationwide analysis. Eur J Clin Nutr 67(11):1169–1174. doi:10.1038/ejcn.2013.164
Ponsky TA, Gasior AC, Parry J, Sharp SW, Boulanger S, Parry R, Ostlie DJ, St Peter SD (2013) Need for subsequent fundoplication after gastrostomy based on patient characteristics. J Surg Res 179(1):1–4. doi:10.1016/j.jss.2012.03.064
Ferluga ED, Sathe NA, Krishnaswami S, McPheeters ML (2014) Surgical intervention for feeding and nutrition difficulties in cerebral palsy: a systematic review. Dev Med Child Neurol 56(1):31–43. doi:10.1111/dmcn.12170
Barnhart DC, Hall M, Mahant S, Goldin AB, Berry JG, Faix RG, Dean JM, Srivastava R (2013) Effectiveness of fundoplication at the time of gastrostomy in infants with neurological impairment. JAMA Pediatr 167(10):911–918. doi:10.1001/jamapediatrics.2013.334
King M, Barnhart DC, O’Gorman M, Downey EC, Jackson D, Mundorff M, Holubkov R, Feola P, Srivastava R (2014) Effect of gastrojejunal feedings on visits and costs in children with neurologic impairment. J Pediatr Gastroenterol Nutr 58(4):518–524. doi:10.1097/MPG.0000000000000227
Wilson GJ, van der Zee DC, Bax NM (2006) Endoscopic gastrostomy placement in the child with gastroesophageal reflux: is concomitant antireflux surgery indicated? J Pediatr Surg 41(8):1441–1445. doi:10.1016/j.jpedsurg.2006.04.021
Gauderer MWL (2006) Gastrostomy. In: Puri P, Hollwarth M (eds) Pediatric Surgery. Springer, Berlin, Heidelberg, pp 181–196
Grunow JE, al-Hafidh A, Tunell WP (1989) Gastroesophageal reflux following percutaneous endoscopic gastrostomy in children. J Pediatr Surg 24(1):42–44 Discussion 44–45
Berezin S, Schwarz SM, Halata MS, Newman LJ (1986) Gastroesophageal reflux secondary to gastrostomy tube placement. Am J Dis Child 140(7):699–701
Jolley SG, Smith EI, Tunell WP (1985) Protective antireflux operation with feeding gastrostomy. Experience with children. Ann Surg 201(6):736–740
Mollitt DL, Golladay ES, Seibert JJ (1985) Symptomatic gastroesophageal reflux following gastrostomy in neurologically impaired patients. Pediatrics 75(6):1124–1126
Coben RM, Weintraub A, DiMarino AJ Jr, Cohen S (1994) Gastroesophageal reflux during gastrostomy feeding. Gastroenterology 106(1):13–18
Seekri IK, Rescorla FJ, Canal DF, Zollinger TW, Saywell R Jr, Grosfeld JL (1991) Lesser curvature gastrostomy reduces the incidence of postoperative gastroesophageal reflux. J Pediatr Surg 26(8):982–984 discussion 984–985
Gauderer MW (1988) Feeding gastrostomy or feeding gastrostomy plus antireflux procedure? J Pediatr Gastroenterol Nutr 7(6):795–796
Sheikh SI, Ryan-Wenger NA, McCoy KS (2013) Outcomes of surgical management of severe GERD in patients with cystic fibrosis. Pediatr Pulmonol 48(6):556–562. doi:10.1002/ppul.22630
Noble LJ, Dalzell AM, El-Matary W (2012) The relationship between percutaneous endoscopic gastrostomy and gastro-oesophageal reflux disease in children: a systematic review. Surg Endosc 26(9):2504–2512. doi:10.1007/s00464-012-2221-8
Vernon-Roberts A, Sullivan PB (2013) Fundoplication versus postoperative medication for gastro-oesophageal reflux in children with neurological impairment undergoing gastrostomy. Cochrane Database Syst Rev 8:CD006151. doi:10.1002/14651858.CD006151.pub3
Toporowska-Kowalska E, Gebora-Kowalska B, Jablonski J, Fendler W, Wasowska-Krolikowska K (2011) Influence of percutaneous endoscopic gastrostomy on gastro-oesophageal reflux evaluated by multiple intraluminal impedance in children with neurological impairment. Dev Med Child Neurol 53(10):938–943. doi:10.1111/j.1469-8749.2011.04031.x
Acknowledgments
The authors declare no conflict of interest. Due to the retrospective nature of the study ethical approval was not sought on the basis of local hospital guidelines. No sources of funding were utilized in the carrying out of this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kakade, M., Coyle, D., McDowell, D.T. et al. Percutaneous endoscopic gastrostomy (PEG) does not worsen vomiting in children. Pediatr Surg Int 31, 557–562 (2015). https://doi.org/10.1007/s00383-015-3707-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3707-y