Abstract
The prevalence of focal cortical dysplasia (FCD) in pediatric patients with focal epilepsy is not exactly known because authors of publications in which the etiologies of epilepsies are listed, but which are not dealing specifically with epilepsy surgery issues, tend to lump together the many kinds of malformations of cortical development (MCD), of which FCDs, because of their relative frequency, are the most relevant subtypes. Out of 561 patients with MCD (children and adults) operated at centers in Europe who do feed data into the “European Epilepsy Brain Bank,” 426 (76 %) had FCD.






Similar content being viewed by others
References
Alexandre V Jr, Capovilla G, Fattore C, Franco V, Gambardella A, Guerrini R, La Briola F, Ladogana M, Rosati E, Specchio LM, Striano S, Perucca E (2010) Characteristics of a large population of patients with refractory epilepsy attending tertiary referral centers in Italy. Epilepsia 51(5):921–925
Bast T (2013) Outcome after epilepsy surgery in children with MRI-negative non-idiopathic focal epilepsies. Epileptic Disord 15(2):105–113
Bast T, Ramantani G, Seitz A, Rating D (2006) Focal cortical dysplasia: prevalence, clinical presentation and epilepsy in children and adults. Acta Neurol Scand 113:72–81
Benifla M, Sala F, Jane J Jr, Otsubo H, Ochi A, Drake J, Weiss S, Donner E, Fujimoto A, Holowka S, Widjaja E, Snead OC 3rd, Smith ML, Tamber MS, Rutka JT (2009) Neurosurgical management of intractable rolandic epilepsy in children: role of resection in eloquent cortex. J Neurosurg Pediatr 4:199–216
Bien CG, Szinay M, Wagner J, Clusmann H, Becker AJ, Urbach H (2009) Characteristics and surgical outcomes of patients with refractory magnetic resonance imaging-negative epilepsies. Arch Neurol 66(12):1491–1499
Blümcke I, Pieper T, Pauli E, Hildebrandt M, Kudernatsch M, Winkler P, Karlmeier A, Holthausen H (2010) A distinct variant of focal cortical dysplasia type I characterised by magnetic resonance imaging and neuropathological examination in children with severe epilepsies. Epileptic Disord 12(3):172–180
Blümcke I, Thom M, Aronica E, Armstrong DD, Vinters HV, Palmini A, Jacques TS, Avanzini G, Barkovich AJ, Battaglia G, Becker A, Cepeda C, Cendes F, Colombo N, Crino P, Cross JH, Delalande O, Dubeau F, Duncan J, Guerrini R, Kahane P, Mathern G, Najm I, Ozkara C, Raybaud C, Represa A, Roper SN, Salamon N, Schulze-Bonhage A, Tassi L, Vezzani A, Spreafico R (2011) The clinico-pathological spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc task force of the ILAE diagnostic methods commission. Epilepsia 52(1):158–174
Blümcke I, Vinters HV, Armstrong D, Aronica E, Thom M, Spreafico R (2009) Malformations of cortical development and epilepsies: neuropathological findings with emphasis on focal cortical dysplasia. Epileptic Disord 11(3):181–193
Chassoux F, Landré E, Mellerio C, Turak B, Mann MW, Daumas-Duport C, Chiron C, Devaux B (2012) Type II focal cortical dysplasia: electroclinical phenotype and surgical outcome related to imaging. Epilepsia 53(2):349–358
Chern JJ, Patel AJ, Jea A, Curry DJ, Comair YG (2010) Surgical outcome for focal cortical dysplasia: an analysis of recent surgical series. J Neurosurg Pediatr 6:452–458
Chugani HT, Shewmon DA, Shields WD, Sankar R, Comair Y, Vinters HV, Peacock WJ (1993) Surgery for intractable infantile spasms: neuroimaging perspectives. Epilepsia 34(4):764–771
Colombo N, Salamon N, Raybaud C, Özkara C, Barkovich AJ (2009) Imaging of malformations of cortical development. Epileptic Disord 11(3):194–205
Colombo N, Tassi L, Deleo F, Citterio A, Bramerio M, Mai R, Sartori I, Cardinale F, Lo Russo G, Spreafico R (2012) Focal cortical dysplasia type IIa and IIb: MRI aspects in 118 cases proven by histopathology. Neuroradiology 54:1056–1077
Colombo N, Tassi L, Galli C, Citterio C, Citterio A, Lo Russo G, Scialfa G, Spreafico R (2003) Focal cortical dysplasias: MR imaging, histopathologic, and clinical correlations in surgically treated patients with epilepsy. AJNR Am J Neuroradiol 24:724–733
Cross JH, Jayakar P, Nordli D, Delalande O, Duchowny M, Wieser HG et al (2006) Proposed criteria for referral and evaluation of children for epilepsy surgery: recommendations of the subcommission for pediatric epilepsy surgery. Epilepsia 47:952–959
D’Argenzio L, Colonnelli MC, Harrison S et al (2012) Seizure outcome after extratemporal epilepsy surgery in childhood. Dev Med Child Neurol 5:995–1000
De Oliveira RS, Santos MV, Terra VC, Sakamoto AC, Machado HR (2011) Tailored resections for intractable rolandic cortex epilepsy in children: a single-center experience with 48 consecutive cases. Childs Nerv Syst 27(5):779–785
Dylgjeri S, Taussig D, Chipaux M, Lebas A, Fohlen M, Bulteau C, Ternier J, Ferrand-Sorbets S, Delalande O, Isnard J, Dorfmüller G (2014) Insular and insulo-opercular epilepsy in childhood: an SEEG study. Seizure 23(4):300–308
Eltze CM, Chong WK, Bhate S, Harding B, Neville BG, Cross JH (2005) Taylor-type focal cortical dysplasia in infants: some MRI lesions almost disappear with maturation of myelination. Epilepsia 46:1988–1992
Escayg A, Wong JC (2014) Toward routine genetics-based diagnosis for the epileptic encephalopathies. Epilepsy Curr 14(3):158–160
Fauser S, Sisodiya SM, Martinian L, Thom M, Gumbinger C, Huppertz HJ, Hader C, Strobl K, Steinhoff BJ, Prinz M, Zentner J, Schulze-Bonhage A (2009) Multi-focal occurrence of cortical dysplasia in epilepsy patients. Brain 132(8):2079–2090
Fogarasi A, Boesebeck F, Tuxhorn I (2003) A detailed analysis of symptomatic posterior cortex seizure semiology in children younger than 7 years. Epilepsia 44:89–96
Fogarasi A, Janszky J, Faveret E, Pieper T, Tuxhorn I (2001) A detailed analysis of frontal lobe seizure semiology in children under 7 years of age. Epilepsia 42:80–85
Fogarasi A, Jokeit H, Faveret E, Janszky J, Tuxhorn I (2002) The effect of age on seizure semiology in childhood temporal lobe epilepsy. Epilepsia 43:638–643
Gaillard WD, Chiron C, Cross JH, Harvey AS, Kuzniecky R, Hertz-Pannier L, Vezina LG, ILAE, Committee for Neuroimaging, Subcommittee for Pediatric (2009) Guidelines for imaging infants and children with recent-onset epilepsy. Epilepsia 50:2147–2153
Gaily EK, Shewmon DA, Chugani HT, Curran JG (1995) Asymmetric and asynchronous infantile spasms. Epilepsia 36(9):873–882
Gambardella A, Palmini A, Andermann F et al (1996) Usefulness of focal rhythmic discharges on scalp EEG of patients with focal cortical dysplasia and intractable epilepsy. Electroencephalogr Clin Neurophysiol 98(4):243–249
Garbelli R, Milesi G, Medici V, Villani F, Didato G, Deleo F, D’Incerti L, Morbin M, Mazzoleni G, Giovagnoli AR, Parente A, Zucca I, Mastropietro A, Spreafico R (2012) Blurring in patients with temporal lobe epilepsy: clinical, high-field imaging and ultrastructural study. Brain 135:2337–2349
Hancock EC, Osborne JP, Edwards SW (2013) Treatment of infantile spasms. Cochrane Database Syst Rev. Issue 6. Art. No.: CD001770. doi:10.1002/14651858.CD001770.pub.3
Harvey AS, Cross JH, Shinnar S, Mathern BW, LAE Pediatric Epilepsy Surgery Survey Taskforce (2008) Defining the spectrum of international practice in pediatric epilepsy surgery patients. Epilepsia 49(1):146–155
Hemb M, Velasco TR, Parnes MS, Wu JY, Lerner JT, Matsumoto JH, Yudovin S, Shields WD, Sankar R, Salamon N, Vinters HV, Mathern GW (2010) Improved outcomes in pediatric epilepsy surgery: the UCLA experience, 1986–2008. Neurology 74(22):1768–1775
Hofmann PAM, Fitt GJ, Harvey AS, Kuzniecky RI, Jackson G (2011) Bottom-of-sulcus dysplasia: imaging features. Am J Roentgenol 196:881–885
Holthausen H, Fogarasi A, Arzimanoglou A, Kahane P (2012) Structural (symptomatic) focal epilepsies of childhood. In: Bureau M, Genton P, Dravet C, Delgado-Escueta A, Tassinari CA, Thomas P & Wolf P (eds) Epileptic syndromes in infancy, childhood and adolescence. John Libbey Eurotext, p 455–505
Holthausen H, Pieper T, Kudernatsch M (2013) Towards early diagnosis and treatment to save children from catastrophic epilepsy - focus on epilepsy surgery. Brain Dev 35(8):730–741
Holthausen H, Pieper T, Kudernatsch M, Blümcke I (2013) Outcome when malformations of cortical development (MCD) are the cause. In: Arts WF, Arzimanoglou A, Brouwer OF, Camfield C, Camfield P (eds) Progress in epileptic disorders—outcome of childhood epilepsies. John Libbey Eurotext, Montrouge, pp 203–215
Holthausen H, Teixeira VA, Tuxhorn I, Pieper T, Ebner A, Kerdar M, Schulz R, Pannek H, Lahl R (1997) Epilepsy surgery in children and adolescents with focal cortical dysplasia. In: Tuxhorn I, Holthausen H, Boenigk H (eds) Paediatric epilepsy syndromes and their surgical treatment. John Libbey & Company, London, pp 199–215
Hrachovy RA, Frost JD Jr (2003) Infantile epileptic encephalopathy with hypsarrhythmia (infantile spasms/West syndrome). J Clin Neurophysiol 20(6):408–425
Hur YJ, Lee JS, Kim DS, Hwang T, Kim HD (2010) Electroencephalography features of primary epileptogenic regions in surgically treated MRI-negative infantile spasms. Pediatr Neurosurg 46(3):182–187
Ikeda A, Sato T, Ohara S, Matsuhashi M, Yamamoto J, Takayama M, Matsumoto R, Mikuni N, Takahashi J, Miyamoto S, Taki W, Hashimoto N, Shibasaki H (2002) “Supplementary motor area (SMA) seizure” rather than “SMA epilepsy” in optimal surgical candidates: a document of subdural mapping. J Neurol Sci 202(1–2):43–52
Iwatani Y, Kagitani-Shimono K, Tominaga K, Okinaga T, Mohri I, Kishima H, Kato A, Sanefuji W, Yamamoto T, Tatsumi A, Murata E, Taniike M, Nagai T, Ozono K (2012) Long-term developmental outcome in patients with West syndrome after epilepsy surgery. Brain Dev 34(9):731–738
Jacobs J (2011) Rolandic spikes - the challenge to differentiate between benign and malignant pediatric epilepsies. Clin Neurophysiol 122(5):851–853
Jayakar P, Dunoyer C, Dean P, Ragheb J, Resnick T, Morrison G, Bhatia S, Duchowny M (2008) Epilepsy surgery in patients with normal or nonfocal MRI scans: integrative strategies offer long-term seizure relief. Epilepsia 49(5):758–764
Jayakar P, Gaillard WD, Tripathi M, Libenson MH, Mathern GW, Cross JH (2014) Task force for paediatric epilepsy surgery, commission for paediatrics, and the diagnostic commission of the international league against epilepsy. Epilepsia 55(4):507–518
Jonas R, Asarnow RF, LoPresti C, Yudovin S, Koh S, Wu JY et al (2005) Surgery for symptomatic infant-onset epileptic encephalopathy with and without infantile spasms. Neurology 64:746–750
Kakisaka Y, Iwasaki M, Haginoya K, Kanno A, Tsuchiya S, Nakasato N (2011) Somatotopic distribution of peri-rolandic spikes may predict prognosis in pediatric-onset epilepsy with sensorimotor seizures. Clin Neurophysiol 122(5):869–873
Kang JW, Rhie SK, Yu R, Eom S, Hong W, Kim SH, Kang HC, Lee JS, Lee YM, Kim HD (2013) Seizure outcome of infantile spasms with focal cortical dysplasia. Brain Dev 35(8):816–820
Kessler-Uberti S, Pieper T, Eitel H, Pascher B, Hartlieb T, Getzinger T, Karlmeier A, Winkler PA, Kudernatsch M, Kolodzieczyk D, Blümcke I, Staudt M, Holthausen H (2011) 12 years of pediatric epilepsy surgery—the Vogtareuth experience. Neuropediatrics 42:S32–S33
Kim DW, Lee SK, Chu K, Park KI, Lee SY, Lee CH, Chung CK, Choe G, Kim JY (2009) Predictors of surgical outcome and pathologic considerations in focal cortical dysplasia. Neurology 72(3):211–216
Kim YH, Kang HC, Kim DS, Kim SH, Shim KW, Kim HD, Lee JS (2011) Neuroimaging in identifying focal cortical dysplasia and prognostic factors in pediatric and adolescent epilepsy surgery. Epilepsia 52(4):722–727
Komaki H, Sugai K, Sasaki M, Hashimoto T, Arai N, Takada E, Maehara T, Shimizu H (1999) Surgical treatment of a case of early infantile epileptic encephalopathy with suppression-bursts associated with focal cortical dysplasia. Epilepsia 40(3):365–369
Kotagal P, Bleasel A, Geller E, Kankirawatana P, Moorjani BI, Rybicki L (2000) Lateralizing value of asymmetric tonic limb posturing observed in secondarily generalized tonic-clonic seizures. Epilepsia 41(4):457–462
Krsek P, Maton B, Korman B, Pacheco-Jacome E, Jayakar P, Dunoyer C, Rey G, Morrison G, Ragheb J, Vinters HV, Resnick T, Duchowny M (2008) Different features of histopathological subtypes of pediatric focal cortical dysplasia. Ann Neurol 63(6):758–769
Krsek P, Pieper T, Karlmeier A, Hildebrandt M, Kolodziejczyk D, Winkler P, Pauli E, Blümcke I, Holthausen H (2009) Different presurgical characteristics and seizure outcomes in children with focal cortical dysplasia type I or II. Epilepsia 50(1):125–137
Kumar RM, O’Neill BR, Koh S, Laoprasert P, Knupp K, Park K, Chapman K, Handler MH (2014) Epilepsy surgery in infants under 1 year of age. Neurosurgery 61(Suppl 1):217
Leach JL, Miles L, Henkel DM, Greiner HM, Kukreja MK, Holland KD, Rose DF, Zhang B, Mangano FT (2014) Magnetic resonance imaging abnormalities in the resection region correlate with histopathological type, gliosis extent, and postoperative outcome in pediatric cortical dysplasia. J Neurosurg Pediatr 14(1):68–80
Lemke JR, Riesch E, Scheurenbrand T, Schubach M, Wilhelm C, Steiner I, Hansen J, Courage C, Gallati S, Bürki S, Strozzi S, Simonetti BG, Grunt S, Steinlin M, Alber M, Wolff M, Klopstock T, Prott EC, Lorenz R, Spaich C, Rona S, Lakshminarasimhan M, Kröll J, Dorn T, Krämer G, Synofzik M, Becker F, Weber YG, Lerche H, Böhm D, Biskup S (2012) Targeted next generation sequencing as a diagnostic tool in epileptic disorders. Epilepsia 53(8):1387–1398
Lerner JT, Salamon N, Hauptman JS, Velasco TR, Hemb M, Wu JY, Sankar R, Donald Shields W, Engel J Jr, Fried I, Cepeda C, Andre VM, Levine MS, Miyata H, Yong WH, Vinters HV, Mathern GW (2009) Assessment and surgical outcomes for mild type I and severe type II cortical dysplasia: a critical review and the UCLA experience. Epilepsia 50(6):1310–1335
Marín-Padilla M (2000) Perinatal brain damage, cortical reorganization (acquired cortical dysplasias), and epilepsy. Adv Neurol 84:153–172
Maton B, Krsek P, Jayakar P, Resnick T, Koehn M, Morrison G, Ragheb J, Castellano-Sanchez A, Duchowny M (2010) Medically intractable epilepsy in Sturge-Weber syndrome is associated with cortical malformation: implications for surgical therapy. Epilepsia 51(2):257–267
Mellerio C, Labeyrie MA, Chassoux F, Daumas-Duport C, Landre E, Turak B, Roux FX, Meder JF, Devaux B, Oppenheim C (2012) Optimizing MR imaging detection of type 2 focal cortical dysplasia: best criteria for clinical practice. AJNR Am J Neuroradiol 33(10):1932–1938
Montavont A, Kahane P, Catenoix H, Ostrowsky-Coste K, Isnard J, Guénot M, Rheims S, Ryvlin P (2013) Hypermotor seizures in lateral and mesial parietal epilepsy. Epilepsy Behav 28(3):408–412
Najm IM, Tassi L, Sarnat HB, Holthausen H, Russo GL (2014) Epilepsies associated with focal cortical dysplasias (FCDs). Acta Neuropathol 128(1):5–19
Noli D, Bartuluchi M, González FS, Kaltenmeier MC, Cersosimo R, Rugilo C, Princich JP, Lubieniecki F, Pomata H, Caraballo R (2013) Type II focal cortical dysplasia: electroclinical study and surgical outcome in 31 pediatric patients. Childs Nerv Syst 29(11):2079–2087
O’Callaghan FJ, Lux AL, Darke K, Edwards SW, Hancock E, Johnson AL et al (2011) The effect of lead time to treatment and of age of onset on developmental outcome at 4 years in infantile spasms: evidence from the United Kingdom infantile spasms study. Epilepsia 52:1359–1364
Osborne JP, Lux AL, Edwards SW, Hancock E, Johnson AL, Kennedy CR, Newton RW, Verity CM, O’Callaghan JK (2010) The underlying etiology of infantile spasms (West sydnrome): Information from the United Kingdom Infantile Spasms Study (UKISS) on contemporary causes and their classification. Epilepsia 51(10):2168–2174
Otsubo H, Chitoku S, Ochi A, Jay V, Rutka JT, Smith ML, Elliott IM, Snead OC 3rd (2001) Malignant rolandic-sylvian epilepsy in children: diagnosis, treatment, and outcomes. Neurology 57(4):590–596
Otsuki T, Honda R, Takahashi A, Kaido T, Kaneko Y, Nakai T, Saito Y, Itoh M, Nakagawa E, Sugai K, Sasaki M (2013) Surgical management of cortical dysplasia in infancy and early childhood. Brain Dev 35(8):802–809
Palmini A, Gambardella A, Andermann F, Dubeau F, da Costa JC, Olivier A, Tampieri D, Robitaille Y, Paglioli E, Paglioli Neto E, Coutinho L, Kim HI (1994) Operative strategies for patients with cortical dysplastic lesions and intractable epilepsy. Epilepsia 35(Suppl 6):S57–S71
Palmini A, Holthausen H (2013) Focal malformations of cortical development: a most relevant etiology of epilepsy in children. Handb Clin Neurol 111:549–565
Pedespan JM, Loiseau H, Vital A, Marchal C, Fontan D, Rougier A (1995) Surgical treatment of an early epileptic encephalopathy with suppression-bursts and focal cortical dysplasia. Epilepsia 36(1):37–40
Rener-Primec ZR, Stare J, Neubauer D (2006) The risk of lower mental outcome in infantile spasms increases after three weeks of hypsarrhythmia duration. Epilepsia 47(12):2202–2205
Rheims S, Ryvlin P, Scherer C, Minotti L, Hoffmann D, Guenot M, Mauguière F, Benabid AL, Kahane P (2008) Analysis of clinical patterns and underlying epileptogenic zones of hypermotor seizures. Epilepsia 49(12):2030–2040
Rowland NC, Englott DJ, Cage TA, Sughrue ME, Barbaro NM, Chang EF (2012) A meta-analysis of predictors of seizure freedom in the surgical management of focal cortical dysplasia. J Neurosurg 116(5):1035–1041
Ryvlin P, Minotti L, Demarquay G, Hirsch E, Arzimanoglou A, Hoffman D, Guénot M, Picard F, Rheims S, Kahane P (2006) Nocturnal hypermotor seizures, suggesting frontal lobe epilepsy, can originate in the insula. Epilepsia 47(4):755–765
Salanova V, Andermann F, Olivier A, Rasmussen T, Quesney LF (1992) Occipital lobe epilepsy: electroclinical manifestations, electrocorticography, cortical stimulation and outcome in 42 patients treated between 1930 and 1991. Brain 115:1655–1680
Shewmoon DA, Shields WD, Chugani HT, Peacock WJ (1990) Contrasts between pediatric and adult epilepsy surgery: rationale and strategy for focal resection. J Epilepsy 3(Suppl):141–155
Tassi L, Garbelli R, Colombo N, Bramerio M, Russo GL, Mai R, Deleo F, Francione S, Nobili L, Spreafico R (2012) Electroclinical, MRI and surgical outcomes in 100 epileptic patients with type II FCD. Epileptic Disord 14(3):257–266
Taussig D, Dorfmüller G, Fohlen M, Jalin C, Bulteau C, Ferrand-Sorbets S, Chipaux M, Delalande O (2012) Invasive explorations in children younger than 3 years. Seizure 21(8):631–638
Thom M, Eriksson S, Martinian L et al (2009) Temporal lobe sclerosis associated with hippocampal sclerosis in temporal lobe epilepsy: neuropathological features. J Neuropathol Exp Neurol 68:928–938
Veeramah KR, Johnstone L, Karafet TM, Wolf D, Sprissler R, Salogiannis J, Barth-Maron A, Greenberg ME, Stuhlmann T, Weinert S, Jentsch TJ, Pazzi M, Restifo LL, Talwar D, Erickson RP, Hammer MF (2013) Exome sequencing reveals new causal mutations in children with epileptic encephalopathies. Epilepsia 54(7):1270–1281
Wang ZI, Alexopoulos AV, Jones SE, Jaisani Z, Najm IM, Prayson RA (2013) The pathology of magnetic-resonance-imaging-negative epilepsy. Mod Pathol 26(8):1051–1058
Widdess-Walsh P, Kellinghaus C, Jeha L, Kotagal P, Prayson R, Bingaman W, Najm IM (2005) Electro-clinical and imaging characteristics of focal cortical dysplasia: correlation with pathological subtypes. Epilepsy Res 67(1–2):25–33
Wieser HG, ILAE Commission on Neurosurgery of Epilepsy (2004) ILAE Commission Report. Mesial temporal lobe epilepsy with hippocampal sclerosis. Epilepsia 45(6):695–714
Williamson PD, Thadani VM, Darcey TM, Spencer DD, Spencer SS, Mattson RH (1992) Occipital lobe epilepsy: clinical characteristics, seizures spread patterns, and results of surgery. Ann Neurol 31(1):3–13
Zuberi SM (2013) Chromosome disorders associated with epilepsy. Handb Clin Neurol 111:543–548
Author information
Authors and Affiliations
Corresponding author
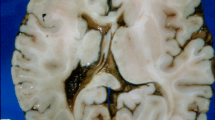
ADDENDUM: imaging in focal cortical dysplasia
ADDENDUM: imaging in focal cortical dysplasia
The principles of MRI with a very low expected rate of false-negative studies are simple: it increased visibility and diagnostic certainty due to the highest reasonably achievable spatial and contrast resolution combined with specialized evaluation of the study. This sounds simple and clear in theory but is in practice not easy to achieve. Recommendations for MRI tend to define a minimal basis and might be directed by common experience and compromise. This is not suitable for maximizing detection of lesions, which are often difficult to find, difficult to exactly define in their extension, and difficult to distinguish from pseudo-lesions and gyral variants. There was a rapid development in MR techniques and specific sequences, and guidelines, recommendations, or methods have been in very general and non-specific terms. Colombo et al. [12] mention T1-weighted inversion recovery as having the best gray-white matter differentiation. Our own experience started also with 2D techniques in patients who underwent pre-surgical evaluations until 2005 but with a higher resolution, particularly in T2 sequences (coronal 1-mm sections with in-plane resolution of 1.0 × 0.5 mm) which were used as 3D substitute.
In the meantime, 3D techniques being common in T1- and T2-weighted gradient echo sequences (T1 1 mm with in-plane resolution of 0.9 × 0.9 mm) were developed for FLAIR and T2 spin echo and were used during the last few years with a slice thickness and in-plane resolution of 0.6 mm in T2 space sequences (Siemens) and slice thickness of 1.2 mm and in-plane resolution of 0.9 × 0.6 mm in 3D FLAIR sequences. These sequences were tested against 2D T2 and 2D inversion recovery sequences and were found to be better regarding contrast than 2D T2 images and equal or slightly better regarding contrast than inversion recovery imaging. The 3D T2 spin-echo imaging was, however, far superior to all other images in 3D or three-planar evaluation, so that one plane of partitions (slices) is sufficient, which was axial for T2 and coronal for FLAIR. The problem with these sequences is the contrast resolution: in T2 space imaging, the spatial l resolution could be achieved in 15–20 min, but a very good contrast resolution needs a long TR of around 4,000 ms and TE of approximately 350 ms. To gain such a contrast with 1.5 T, the time is around 1 h for one 3D sequence. This time can only be reduced (but not halved) by performing the examination with a 3-T system. Another pre-requisition is that one needs very skilled pediatric anesthesiologists and dedicated technicians, as well as an adequate MRI machine to keep respiration- and vibration-induced head motions and inhomogeneities to a minimum. Last but not the least, one needs time and dedication for evaluation of the two 3D datasets (e.g., 320 images in T2 space), using three-planar and fusion techniques.
P. Winkler
(Pediatric Neurology)
Rights and permissions
About this article
Cite this article
Holthausen, H., Pieper, T., Winkler, P. et al. Electro-clinical-pathological correlations in focal cortical dysplasia (FCD) at young ages. Childs Nerv Syst 30, 2015–2026 (2014). https://doi.org/10.1007/s00381-014-2549-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-014-2549-6