Abstract
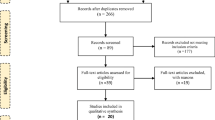
Systolic and diastolic functions of both ventricles play a crucial role in the progression of chronic heart failure (CHF). As data about the role of dietary habits in ventricular dysfunction are lacking, we aimed to evaluate the relationship between biventricular diastolic and systolic function and dietary habits in patients with CHF. During 2007, 372 consecutive CHF patients were enrolled. Biventricular systolic and diastolic function was evaluated through echocardiography. Dietary habits were recorded using a food frequency questionnaire, and adherence to a Mediterranean diet was evaluated using the MedDietScore. The MedDietScore was positively correlated with log Smv, left atrial EF and V p, and inversely correlated with log EA and log Emv/Amv levels (p < 0.05). After adjusting for potential confounders, only log E/A levels were inversely associated with the MedDietScore (p < 0.05). Following analysis per specific aliments, the log E/A ratio was inversely associated with fish intake and olive oil use; the log Emv/Amv ratio was inversely associated with fish intake; log Stv was positively associated with fish, olive oil and pasta intake; log LAKE was positively associated with olive oil use and alcohol drinking (all p < 0.05). This study demonstrated, in a cross-sectional design, a potential beneficial effect of a Mediterranean diet on biventricular systolic and diastolic function.
Similar content being viewed by others
Introduction
Despite therapeutic advances made over the past 15 years, heart failure remains one of the main components of the overall burden of cardiovascular morbidity and mortality [1]. Finding innovative ways to prevent cardiovascular death is a major challenge. Among other approaches, the role of lifestyle modification has attracted the interest of clinicians in the field of chronic heart failure (CHF).
During the past 20 years, several observational studies and clinical trials have provided scientific evidence that the Mediterranean diet, rich in fruits, vegetables, legumes, whole grains, fish and low-fat dairy products, with olive oil as the principal source of fat, is associated with a lower incidence of cardiovascular disease (CVD) and some cancer types [2–7]. In 1999, the Lyon Heart Study, a randomised secondary prevention clinical trial of coronary heart disease (CHD) patients, revealed the protective effect of this dietary pattern on cardiac complications of patients within the first 27 months of follow-up [3]. More recently, the GREECS study investigators, studying 2,172 acute coronary syndrome patients, observed that long-term adherence to a Mediterranean diet had a beneficial effect both on the severity of the event and on short- and long-term prognosis [4]. Several pathophysiological mechanisms have been proposed to explain the beneficial effects of a Mediterranean diet on the cardiovascular system, including the diet’s antithrombotic, anti-inflammatory and antioxidant effects [5–7]. Recently, adherence to a Mediterranean diet was shown to favorably affect heart rate (HR) variability, an established measure of cardiac autonomic dysfunction. In terms of nutrients, the traditional Mediterranean diet is a diet rich in oleic acid, omega-3 fatty acids (n-3 PUFA), fibre, B-group vitamins and various antioxidants, but low in saturated and polyunsaturated fats [8]. Given the compromised nutritional status of systolic heart failure patients, potentially related to increased cytokine levels [9], a dietary pattern addressing both issues of inflammation and insufficient micronutrient intake might favourably affect mortality and morbidity. Indeed, in the GISSI-HF trial, long-term administration of n-3 PUFA effectively reduced both all-cause mortality and hospital admissions for cardiovascular reasons in CHF patients [10]. This notion is consistent with the results of published epidemiological and experimental studies documenting reduction of neurohormonal responses and improvement in left ventricular diastolic function [11].
The study of diastolic function has attracted the interest of investigators, having a prognostic role in the progression of heart failure [12]. Both tissue Doppler imaging (TDI) of mitral annular motion and colour M-mode (V p) have been proposed to be pre-load-independent measures that correlate well with the time constant of the left ventricle pressure (tau) and act as a good non-invasive measures of left ventricular relaxation [12, 13].
Despite evidence from observational studies and clinical trials concerning the beneficent effect of the Mediterranean dietary pattern or its components on the prevention of CHD, studies assessing the influence of the Mediterranean diet on the severity of systolic and diastolic ventricular function in CHF patients are lacking. Therefore, the main purpose of this work is to evaluate the relationship between adherence to this diet and: (1) left and right ventricular systolic function, (2) left atrial function and (3) ventricular diastolic filling pressures, as assessed by pulse wave and TDI study, in patients with stable CHF under optimal medical treatment.
Methods
Patients
We enrolled 372 consecutive patients (314 male, age 64 ± 13 years and 58 female, age 63 ± 13 years) with diagnosed chronic systolic (ejection fraction <40%) heart failure due to ischaemic or dilated cardiomyopathy. The number of enrolled participants is adequate to evaluate differences on echocardiographic markers in the range of 1 SD between diet groups at 5% significance level, achieving 87% statistical power. CHF due to ischaemic heart disease or dilated cardiomyopathy was diagnosed on the basis of the ESC criteria [1]. A detailed medical history was recorded, including all medications received. Blood pressure was measured, and patients with average blood pressure levels ≥140/90 mmHg or under antihypertensive medication were classified as hypertensive. Participants with total serum cholesterol levels >200 mg/dl or taking lipid-lowering agents were classified as hypercholesterolemic and those with blood sugar >125 mg/dl or under antidiabetic medication were classified as diabetic.
Demographic characteristics of patients were recorded. Smoking habits were recorded using a standardised questionnaire. Those smoking at least one cigarette per day were defined as current smokers. Participants who did not report any physical activities were defined as sedentary. Body mass index (BMI) was calculated as weight (in kilograms) divided by standing height (in metres) squared. Obesity was defined as BMI >29.9 kg/m2, while renal function was determined through the Cockcroft-Gault formula [14]. Other clinical variables (cardiomyopathy aetiology, NYHA class) were also registered.
Patients with atrial fibrillation were excluded from the study, since evaluation of diastolic indexes in this condition is of limited value.
The Institutional Review Board approved the study design, and all patients gave informed written consent. The investigation conforms to the principles outlined in the Declaration of Helsinki.
Dietary assessment and evaluation of adherence to the Mediterranean diet
Usual food intake over the year preceding hospitalisation was assessed in all patients based on a repeatable and validated semi-quantitative food frequency questionnaire [15], which included 75 items (foods and beverages commonly consumed in Greece). Serving sizes were included in the food frequency questionnaire in order to assist patients in reporting accurate information and to allow for quantification of dietary habits. Alcohol consumption was measured in wine glasses (100 ml) and quantified by ethanol intake (grams per drink)—one wine glass containing 12 g of ethanol. Moreover, the MedDietScore was calculated in order to evaluate the level of adherence to the Mediterranean diet [16]. In particular, intake of ten food groups was evaluated (i.e. non-refined cereals and products, fruits and nuts, vegetables, olive oil, dairy, fish, poultry, potatoes, pulses, red meat or meat products, and eggs), as well as alcohol drinking. Note the non-monotonic scoring of alcohol consumption, following the rationale of the Mediterranean dietary pattern that encourages the intake of 15–30 g of ethanol per day. Higher values of this diet score indicate greater adherence to the Mediterranean diet, and have been associated with global CVD risk as well as CVD risk factors reduction [16].
Echocardiographic/Doppler examination
Detailed echocardiographic assessment was performed in all patients during the 3rd day of hospitalisation. We only enrolled patients with left ventricular systolic dysfunction (LVEF <40% by Simpson’s method). Using a Hewlett Packard 5500 Sonos with a multifrequency transducer (2.5–4 MHz), equipped with TDI technology, images were acquired with patients in left lateral decubitus position. From the apical four-chamber view, a 10-mm3 sample volume was placed at the lateral mitral and tricuspid annulus, and spectral TDI was recorded, with the motion of annuli parallel to the TDI cursor. Pulse wave TDI was characterised by the systolic wave (Smv and Stv) and two diastolic waves (Emv, Emv and Etv and Atv, respectively). Furthermore, using pulse wave Doppler at the tips of mitral leaflets, early and late velocity waves (E and A) were recorded. HR was recorded as beats per minute. Left atrial volumes were measured at end diastole and systole, and the left atrial ejection fraction was calculated. Left atrial kinetic energy (LAKE) was calculated using the equation 1/2 × LASV × 1.06 × A 2; where LASV is the left atrial stroke volume [17]. The left ventricular outflow area was calculated from the left parasternal long axis view, while the cardiac index (CO) was calculated by the formula π/4 × (LVOT)2 × VTILVOT × HR, where VTILVOT is the time-velocity integral of the left ventricular outflow tract, as detected by pulse wave Doppler from the apical four-chamber view. All measurements were averaged on three to five measurements obtained during end expiration. Furthermore, using the colour M-mode by placing the M-mode cursor aligned parallel to the left ventricular inflow extending from the apex to the tips of mitral valve, we measured the propagation velocity (V p). V p is defined as the velocity with which blood moves from mitral annulus to apex. The slope of a line drawn over the colourised flow from the mitral valve into the left ventricular cavity during early diastole yields V p [18].
Data analysis
Normally distributed continuous variables (age, body mass index, Smv, Stv, left atrial EF and V p) are presented as mean values ± SD, while skewed variables (E/A, E/Emv, LAKE and Emv/Amv) are presented as median and quartiles. Skewed variables were log-transformed in order to be included in the regression analyses. Categorical variables are presented as frequencies. Normality was tested using the P-P plots. Associations between categorical variables were tested using Pearson’s chi-squared test. Comparisons between groups of patients in the case of normally distributed variables were performed using the Student’s t test, after testing for equality of variances. Correlations between normally distributed continuous variables were evaluated by the calculation of Pearson’s r coefficient, while correlations between skewed continuous or discrete variables were evaluated by the use of Spearman’s rho rank coefficient. Associations between left atrial function and systolic ventricular function markers (dependent variables) and MedDietScore (independent variable) were also tested through multiple linear regression analysis, after adjusting for various potential confounders. Results from regression models are presented as b-coefficients and 95% CI of the coefficient. Assumptions of linearity for the continuous independent variables and constant variance of the standardised residuals were assessed by plotting the residuals against the fitted values. Colinearity of the independent variables was tested using the VIF criterion. All reported p values are based on two-sided tests. SPSS 14.0 software (SPSS Inc. 2004, Chicago, IL, USA) was used for all statistical calculations.
Results
In Table 1 patients’ characteristics are presented. As seen, patients closely adhering to the Mediterranean dietary pattern had higher prevalence of ischaemic cardiomyopathy (p = 0.001), lower E/A (p = 0.009) and higher Smv values (p = 0.016).
The main medication therapy beyond furosemide included: β and α blockers, angiotensin-converting enzyme inhibitors, aldosterone antagonists, aspirin (in cases of ischaemic cardiomyopathy) and statins. No differences were observed between the low and upper quartile of a Mediterranean type of diet according to the type of medication. Furthermore, 82 patients (22%) were under cardiac resynchronisation therapy, with no significant differences between tertiles of diet.
In Table 2 patients’ echocardiographic indices are also presented. Unadjusted analyses revealed that the MedDietScore positively correlated with log Smv (r = 0.154, p = 0.009), left atrial EF (r = 0.133, p = 0.041) and V p (r = 0.129, p = 0.040), while inverse correlations were observed between the MedDietScore and log E/A (r = −0.224, p < 0.001), log Emv/Amv levels (r = −0.133, p = 0.041) and log LAKE (r = 0.17, p = 0.012). Statistically non-significant correlations with the diet score were observed regarding log Stv (r = 0.085, p = 0.163) and log E/Emv (r = −0.067, p = 0.279).
Table 3 presents the results from multiple linear regression analyses that evaluated the association between echocardiographic indices of CHF patients and adherence to the Mediterranean diet. After adjusting for potential confounding factors (age, sex, physical inactivity, smoking habits, obesity, history of hypertension, hypercholesterolemia and diabetes mellitus, ejection fraction and years of heart failure) log E/A levels were inversely associated with the MedDietScore (p = 0.047). No other significant associations were observed regarding MedDietScore and other echocardiographic indices in the whole cohort of patients. When the data analysis was stratified according to the type of cardiomyopathy (ischaemic or dilated), linear regression analysis revealed that MedDietScore was found to be inversely related to E/V p (b = −0.225 ± 0.092, β = −0.782, p = 0.04) in patients with dilated cardiomyopathy, while no such significant relation was evident in the case of ischaemic cardiomyopathy, after adjustments were made for creatinine clearance, physical inactivity, hypertension, diabetes mellitus, smoking and left ventricular ejection fraction.
Regarding other investigated characteristics, age was inversely associated with E/A (p < 0.01), left atrial EF (p < 0.05) and Emv/Amv ratio (p < 0.05); sex was not associated with any of the studied systolic function indices; similarly, physical activity status showed statistically non-significant results, while smoking habits were inversely associated only with Emv/Amv ratio (p < 0.1). When pack-years of smoking or intension and duration of exercise were also considered in the analysis, no significant associations were found. Among clinical features, only diabetes was inversely associated with left atrial EF (p < 0.01).
Furthermore, food-specific analysis (frequency of specific foods consumption per week) showed that fish intake was inversely associated with log Emv/Amv ratio (b ± SE: −0.12 ± 0.07, p = 0.09) and log E/A ratio (b ± SE: −0.21 ± 0.08, p = 0.008), and positively associated with log Stv (b ± SE: 0.08 ± 0.04, p = 0.03); dairy product consumption was inversely associated with log Smv (b ± SE: −0.13 ± 0.07, p = 0.06); olive oil use in daily cooking and salads was positively associated with log Stv (b ± SE: 0.07 ± 0.03, p = 0.01) and log LAKE (b ± SE: 0.16 ± 0.09, p = 0.09), and inversely associated with log E/A ratio (b ± SE: −0.09 ± 0.05, p = 0.06). Finally, regarding alcohol drinking, it was inversely associated with log E/Emv ratio (b ± SE: −0.08 ± 0.04, p = 0.05) and log LAKE (b ± SE: −0.20 ± 0.09, p = 0.02), while no differences in the effect size measures were observed when the type of alcoholic beverage was taken into account.
Discussion
This study revealed that closer adherence to the Mediterranean type of diet may be associated with an improved left ventricular diastolic filling pattern in patients with CHF under optimal treatment. Furthermore, aliment-specific analysis revealed the potential beneficial effect of vegetables, fish and olive oil on left and right ventricular systolic and diastolic indices, illustrating an alternative non-pharmacological therapeutic strategy in these patients.
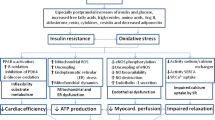
The Mediterranean diet has been shown in several studies to possess anti-inflammatory properties and have a beneficial impact on primary and secondary prevention [2–6]. Ancel Keys was the first to report the exceedingly low cardiovascular mortality rates in middle-aged men living in certain Greek islands, compared to the rest of the Seven Countries Study cohort. He attributed this finding mainly to their dietary habits [2]. Additionally, findings from several epidemiological studies and intervention trials provide evidence that constant exposure to meals rich in certain nutrients stresses the immune or metabolic system through generation of a pro-inflammatory milieu, leading to immune and metabolic disorders, ending and adding up to metabolic disease, vascular endothelial dysfunction and CVD [19]. In the field of heart failure there is evidence that inflammatory markers may correlate with diastolic dysfunction irrespective of systolic function, and this may be the key element for the progression from compensated to de-compensated heart failure [20–22]. The Mediterranean diet, due to its unique anti-inflammatory properties, may have a beneficial impact on diastolic filling pressures. Furthermore, dietary supplementation with omega-3 PUFA seems to attenuate pressure overload-induced LV dysfunction, in animal experimental models, and this effect was associated with elevated plasma adiponectin [23].
There has been increasing recognition that diastolic ventricular function plays an essential role in the clinical progression of systolic heart failure, explaining differences in clinical symptoms between patients with similar degrees of systolic dysfunction [20]. Echocardiographic techniques allow for evaluation of systolic function and ventricular diastolic filling pressures of both ventricles. Doppler recordings of left ventricular filling velocities correlate closely with ventricular filling parameters measured by other invasive techniques [13]. The ratio E to A offers an accurate and repeatable index of left ventricular filling pressures. In this study, since the mean age of participants was high (65 years), a reduced E to A ratio is anticipated; increasing values of it may represent the progression from pseudonormalisation to restriction due to elevated diastolic pressures, although it depends on left ventricular pre-load, age and anthropometric measurements [24]. Additionally, TDI has been recognised as a useful echocardiographic tool for quantitative assessment of left ventricular systolic and diastolic function, irrespective of loading conditions. Recent studies have explored the prognostic role of TDI-derived parameters in major cardiac diseases, such as heart failure, acute myocardial infarction and hypertension. In these conditions, myocardial mitral annular or basal segmental systolic (Smv) and early diastolic (Emv) velocities have been shown to predict mortality or cardiovascular events [25, 26]. In this study, a higher MedDietScore, which represents closer adherence to the Mediterranean type of diet, seems to correlate with an improved left ventricular filling pattern, described as a reduced ratio of E/A and Emv/Amv, which represents the mildly impaired relaxation that accompanies compensated heart failure in middle-aged and elderly patients. Additionally, fish consumption was positively associated with Smv, suggesting a favourable effect on the intrinsic systolic capacity of the right ventricle, which has been associated with favourable clinical outcomes [27]. Long-term fish consumption has been associated, in previous studies, with antiarrhythmic and anti-inflammatory protection [28], while supplementation with eicosapentaenoic acid and docosahexaenoic acid from fish oil has recently been shown to prevent the development of heart failure through alterations in cardiac phospholipids that favourably impact inflammation and energy metabolism [29]. In accordance with these findings, fish consumption in this study showed beneficial effects on left ventricular diastolic filling patterns and right ventricle systolic function. Previous studies have demonstrated that right ventricular dysfunction in patients with systolic heart failure is common and is associated with increased mortality [30, 31]. Right ventricular systolic function may be assessed by TDI of the systolic wave of the tricuspid annulus (Stv). In our study, patients with greater consumption of olive oil and fish showed higher values of Stv, suggesting improved right ventricular systolic function.
Olive oil consumption has been shown to protect against the development of heart failure following an acute coronary event, mainly due to its anti-inflammatory and antioxidant properties that have beneficial effects on cardiac myocyte function [32, 33]. In experimental models, olive oil consumption was shown to reduce infarct size and protect re-perfused myocardium from oxidative damage in vivo [34].
Further evidence suggests that left atrial myopathy and failure may coexist or precede left ventricular myopathy and failure [35]. Indeed, left atrial contractile reserve impairment might be an early finding in the process of heart failure. In the early stages of left ventricular systolic dysfunction, early ventricular diastolic inflow is decreased, consequently atrial passive emptying is decreased, and the atrial active pumping function in late diastole is increased. Thus, left atrial reservoir, conduit and pumping functions are reorganised, maintaining ventricular filling. As heart failure progresses, left atrial function decreases because of increased afterload. Eventually, intrinsic left atrial dysfunction develops [36]. In this study, higher consumption of alcohol and salads, food items with increased antioxidant content, seems to benefit left atrial function, leading to improved diastolic filling.
Flow propagation (V p) is reduced in heart failure because of increased ventricular stiffness and impaired suction. Recently, it was shown that V p is relatively independent of loading conditions and correlates well with tau, especially in dilated cavities. V p values of <40 cm/s imply diastolic dysfunction with impaired relaxation [18]. In this study, two components of the Mediterranean diet, namely alcohol and legumes, have been shown to improve diastolic function, reflecting improved left ventricular relaxation and suction. In another study, moderate alcohol consumption appeared to protect against congestive heart failure, while heavier consumption was not associated with worsening of congestive heart failure in a community-based sample from the Framingham Heart Study [37]. Additionally the ratio E/V p was found to be inversely correlated to the MedDietScore only in non-ischaemic cardiomyopathy. The global hypokinesia of left ventricular segments in non-coronary heart failure reveals a more prominent impaired suction, as indicated by the V p values. In those patients the beneficial effect of the Mediterranean Diet could be more evident.
Limitations
The main limitations of this study are due to its cross-sectional nature. Hence, the finding of a relationship between the Mediterranean diet and certain echocardiographic measurements does not imply causality, but rather generates a hypothesis for future research. A prospective observational study or a randomised clinical trial would better address the limitations of this work, and refute or confirm the presented findings. Moreover, residual confounding, unmeasured factors could always have an impact on the effect size measures reported here. The large number of multiple comparisons increased the likelihood of false-positive results (type I error), and therefore, p values much lower than 0.01 should be considered highly significant. Nevertheless, adherence to this dietary pattern is considered to be lifelong; thus, it could be hypothesised that participants were “exposed” to this healthy dietary pattern before the potential development of the disease. Moreover, an effort was made to account for potential confounding factors in the multi-adjusted analyses.
Conclusion
This study puts forth the hypothesis of a new pathophysiological mechanism concerning the role of diet in patients with systolic heart failure. In such patients, impairment of diastolic filling seems to correlate with increased dairy product consumption, while fish, alcohol, olive oil and the Mediterranean diet as a whole were associated with better left ventricular filling pressure and systolic function of both ventricles. These findings underline the need for future dietary interventions on patients with systolic CHF in order to establish or not the potential role of the Mediterranean type of diet as an additional therapeutic strategy [38].
References
Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, Klapholz M, Moser DK, Rogers JG, Starling RC, Stevenson WG, Tang WHW, Teerlink JR, Walsh MN (2010) Executive summary: HFSA 2010 comprehensive heart failure practice guideline. J Card Fail 16:475–539
Keys A, Mienotti A, Karvonen MJ, Aravanis C, Blackburn H, Buzina R, Djordjevic BS, Dontas AS, Fidanza F, Keys MH, Kromhout D, Nedeljkovic S, Punsar S, Seccareccia F, Toshima H (1986) The diet and 15-year death rate in the Seven Countries Study. Am J Epidemiol 124:903–915
De Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N (1999) Mediterranean diet, traditional risk factors and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation 99:779–785
Panagiotakos DB, Arapi S, Pitsavos C, Antonoulas A, Mantas Y, Zombolos S, Stefanadis C (2006) The relationship between adherence to the Mediterranean diet and the severity and short-term prognosis of acute coronary syndromes (ACS): The Greek Study of ACS (The GREECS). Nutrition 22:722–730
Carter SJ, Roberts MB, Salter J, Eaton CB (2010) Relationship between Mediterranean Diet Score and atherothrombotic risk: findings from the Third National Health and Nutrition Examination Survey (NHANES III), 1988–1994. Atherosclerosis 210:630–636
Chrysohoou C, Panagiotakos DB, Pitsavos C, Das UN, Stefanadis C (2004) Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults. The ATTICA Study. J Am Coll Cardiol 44:152–158
Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, D’Armiento M, D’Andrea F, Giugliano D (2004) Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA 292:1440–1446
Simopoulos AP (2009) Omega-6/omega-3 essential fatty acids: biological effects. World Rev Nutr Diet 99:1–16
Catapano G, Pedone C, Nunziata E, Zizzo A, Passantino A, Incalzi RA (2008) Nutrient intake and serum cytokine pattern in elderly people with heart failure. Eur J Heart Fail 10:428–434
Gissi-HF Investigators, Tavazzi L, Maggioni AP, Marchioli R, Barlera S, Franzosi MG, Latini R, Lucci D, Nicolosi GL, Porcu M, Tognoni G (2008) Effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet 372:1223–1230
Mozaffarian D, Geelen A, Brouwer IA, Geleijnse JM, Zock PL, Katan MB (2005) Effect of fish oil on heart rate in humans: a meta-analysis of randomized controlled trials. Circulation 112:1945–1952
Appleton CP, Hatle LK, Popp RL (1998) Relation of transmitral flow velocity patterns to left ventricular diastolic function: new insights from a combined hemodynamic and Doppler echocardiographic study. J Am Coll Cardiol 12:426–440
Gunes Y, Guntekin U, Tuncer M, Sahin M (2009) Improved left and right ventricular functions with trimetazidine in patients with heart failure: a tissue Doppler study. Heart Vessels 24:277–282
Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16:31–41
Tyrovolas S, Pounis G, Bountziouka V, Polychronopoulos E, Panagiotakos DB (2010) Repeatability and validation of a short, semi-quantitative food frequency questionnaire designed for older adults living in Mediterranean areas: the MEDIS-FFQ. J Nutr Elder 29:311–324
Panagiotakos DB, Pitsavos C, Stefanadis C (2006) Dietary patterns: a Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr Metab Cardiovasc Dis 16:559–568
Dardas PS, Pitsis AA, Tsikaderis DD, Mezilis NE, Geleris PN, Boudoulas HK (2004) Left atrial volumes function and work before and after mitral valve repair in chronic mitral regurgitation. J Heart Valve Dis 13:27–32
Garcia MJ, Smedira NG, Greenberg NL, Main M, Firstenberg MS, Odabashian J (2000) Color M-mode Doppler flow propagation velocity is a preload insensitive index of left ventricular relaxation: animal and human validation. J Am Coll Cardiol 35:201–208
Ueeda M, Doumei T, Takaya Y, Ohnishi N, Takaishi A, Hirohata S, Miyoshi T, Shinohata R, Usui S, Kusachi S (2011) Association of serum levels of arachidonic acid and eicosapentaenoic acid with prevalence of major adverse cardiac events after acute myocardial infarction. Heart Vessel 26:145–152
Chrysohoou C, Pitsavos C, Barbetseas J, Kotroyiannis I, Brili S, Vasiliadou K, Papadimitriou L, Stefanadis C (2009) Chronic systemic inflammation accompanies impaired ventricular diastolic function, detected by Doppler imaging, in patients with newly diagnosed systolic heart failure (Hellenic Heart Failure Study). Heart Vessels 24:22–26
Yan AT, Yan RT, Cushman M, Redheuil A, Tracy RP, Arnett DK, Rosen BD, McClelland RL, Bluemke DA, Lima JA (2010) Relationship of interleukin-6 with regional and global left-ventricular function in asymptomatic individuals without clinical cardiovascular disease: insights from the Multi-Ethnic Study of Atherosclerosis. Eur Heart J 31:875–882
Hughes CM, Woodside JV, McGartland C, Roberts MJ, Nicholls DP, McKeown PP (2010) Nutritional intake and oxidative stress in chronic heart failure. Nutr Metab Cardiovasc Dis. doi:10.1016/j.numecd.2010.08.006
Duda MK, O’Shea KM, Lei B, Barrows BR, Azimzadeh AM, McElfresh TE, Hoit BD, Kop WJ, Stanley WC (2007) Dietary supplementation with omega-3 PUFA increases adiponectin and attenuates ventricular remodeling and dysfunction with pressure overload. Cardiovasc Res 76:303–310
Wada H, Shinjo D, Kameda S, Ono K, Satoh N, Morimoto T, Osakada G, Nakano T, Fujita M, Shimatsu A, Hasegawa K (2010) Transmitral E/A ratio decreases in association with abdominal fat accumulation in patients with impaired glucose tolerance or mild diabetes without left ventricular hypertrophy. Heart Vessels 25:45–50
Zile MR, Brutsaert DL (2002) New concepts in diastolic dysfunction and diastolic heart failure: part I: diagnosis, prognosis and measurements of diastolic function. Circulation 105:1387–1393
Yu CM, Sanderson JE, Marwick TH, Oh JK (2007) Tissue Doppler imaging. A new prognosticator for cardiovascular diseases. J Am Coll Cardiol 49:1903–1914
Chrysohoou C, Antoniou CK, Kotrogiannis I, Metallinos G, Aggelis A, Andreou I, Brili S, Pitsavos C, Stefanadis C (2011) The role of right ventricular systolic function on long-term outcome in patients with newly diagnosed systolic heart failure. Circ J 75:2176–2181
Chrysohoou C, Panagiotakos DB, Pitsavos C, Skoumas J, Krinos X, Chloptsios Y, Nikolaou V, Stefanadis C (2007) Long-term fish consumption is associated with protection against arrhythmia in healthy persons in a Mediterranean region—the ATTICA study. Am J Clin Nutr 85:1385–1391
Shah KB, Duda MK, O’Shea KM, Sparagna GC, Chess DJ, Khairallah RJ, Robillard-Frayne I, Xu W, Murphy RC, Des Rosiers C, Stanley WC (2009) The cardioprotective effects of fish oil during pressure overload are blocked by high fat intake: role of cardiac phospholipid remodeling. Hypertension 54:605–611
Meluzin J, Spinarová L, Hude P, Krejcí J, Dusek L, Vítovec J, Panovsky R (2005) Combined right ventricular systolic and diastolic dysfunction represents a strong determinant of poor prognosis in patients with symptomatic heart failure. Int J Cardiol 105:164–173
Kjaergaard J, Akkan D, Iversen KK, Kober L, Torp-Pedersen C, Hassager C (2007) Right ventricular dysfunction as an independent predictor of short and long term mortality in patients with heart failure. Eur J Heart Fail 9:610–616
Chrysohoou C, Kastorini CM, Panagiotakos D, Aggelopoulos P, Tsiachris D, Pitsavos C, Stefanadis C (2009) Exclusive olive oil consumption is associated with lower likelihood of developing left ventricular systolic dysfunction in acute coronary syndrome patients: The Hellenic Heart Failure Study. Ann Nutr Metab 56:9–15
Chrysohoou C, Panagiotakos DB, Aggelopoulos P, Kastorini CM, Kehagia I, Pitsavos C, Stefanadis C (2010) The Mediterranean diet contributes to the preservation of left ventricular systolic function and to the long-term favourable prognosis of patients who have had an acute coronary event. Am J Clin Nutr 92:47–54
Andreadou I, Iliodromitis EK, Mikros E, Constantinou M, Agalias A, Magiatis P, Skaltsounis AL, Kamber E, Tsantili-Kakoulidou A, Kremastinos D (2006) The olive constituent oleuropein exhibits anti-ischemic, anti-oxidative and hypolipidemic effects in anesthetized rabbits. J Nutr 136:2213–2219
Chrysohoou C, Pitsavos C, Barbetseas J, Brili S, Kotroyiannis I, Papademetriou L, Metallinos G, Skoumas J, Tentolouris C, Stefanadis C (2008) Serum uric acid levels correlate with left atrial function and systolic right ventricular function in patients with newly diagnosed heart failure: the Hellenic heart failure study. Congest Heart Fail 14:229–233
Prioli A, Marino P, Lanzoni L, Zardini P (1998) Increasing degrees of left ventricular filling impairment modulates left atrial function in humans. Am J Cardiol 82:756–761
Walsh CR, Larson MG, Evans JC, Djousse L, Ellison RC, Vasan RS, Levy D (2002) Alcohol consumption and risk for congestive heart failure in the Framingham Heart Study. Ann Intern Med 136:181–191
Heart Failure Society of America (2010) Nonpharmacologic management and health care maintenance in patients with chronic heart failure. J Card Fail 16:e61–e72
Acknowledgments
The authors would like to thank Ms Christina-Maria Kastorini, MSc, and Ms S. Paspaliari, MSc, for their assistance in dietary data selection.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chrysohoou, C., Pitsavos, C., Metallinos, G. et al. Cross-sectional relationship of a Mediterranean type diet to diastolic heart function in chronic heart failure patients. Heart Vessels 27, 576–584 (2012). https://doi.org/10.1007/s00380-011-0190-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-011-0190-9